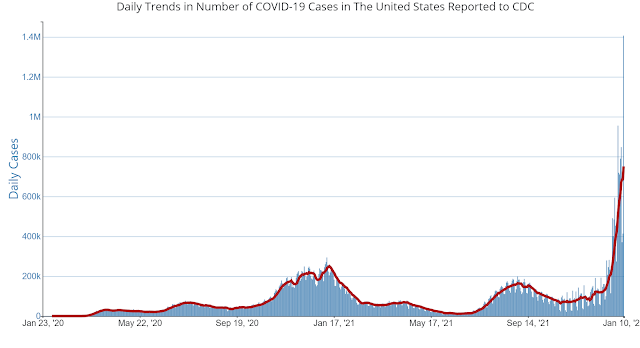
The public health measures seemed less effective. That
could be confirmed by a walk around Target or Walmart. At the absolute peak of
mask wearing in Minnesota, my estimates were up to 30% of shoppers were masked.
Half of those masks were loose fitting cloth masks and probably not very
effective. Today, at the height of the Omicron spike 10% of the people in my
coffee shop were masked and I was the only guy wearing an N95. Despite an increasingly vocal group of
aerosol scientists most people remain shockingly ignorant or willfully ignoring
the airborne route of transmission. The most easily observed scenario is
restaurant dining where the customers wear a mask to the table and then take it
off to eat and talk for the next two hours. There is no magical protection from
airborne virus in that scenario. Forget about the 6 feet safe distance rule at
the start of the pandemic. Looking for restaurants that have improved their
HVAC systems to improve airflow and air exchanges over time was also
disappointing. So far in the Twin Cities Metro area I have found 1 restaurant.
No restaurant or business as far as I know is posting their air exchanges per
hour or carbon dioxide measurements to describe the potential risk of their
environment. They are posting that they adhere to social distancing and all of
the surfaces are wiped clean between diners.
Despite all of that inertia, the restaurants are
packed. Typically, shutdown occurs when
a significant number of staff are ill with coronavirus and they cannot stay
open. I dodged a bullet at Christmas just as infections were increasing. My
wife and I were supposed to meet another couple at a restaurant. My suggestion
to get take out and eat it at either of our homes was met with resistance. I
was saved by a call from that restaurant that significant numbers of their
staff were ill and they would be closing until things improved.
The general cultural landscape has been even more grim. I
follow all of the experts in the media on a regular basis – Drs. Fauci, Hotez,
Jha, and Walensky. On an average day
they are awash in a sea of misinformation.
That sea contains the entrepreneurs who see the pandemic as a money-making
scheme as well as the purely irrational who find that conspiracy theories about
the virus, vaccine, and public health measures are easier to understand and
believe than the science. Political opportunists are in the mix and as recently
as today were suggesting that “white people” were being discriminated against
and were less likely to get the vaccine as a result. The Florida Governor made this
statement:
“We reject the biomedical security state that curtails
liberty, ruins livelihoods and divides society.”
Biomedical security state? The politicization of this
pandemic knows no bounds. It obscures both the science and goodwill toward the
scientific and medical communities. But
it doesn’t stop there. In some large
health care organizations 10% of the workforce has been fired for not complying
with workplace mandates on COVID-19 immunizations. Some of these workers are physicians who
should have been taught basic epidemiological concepts – the most basic being
that vaccinations are a rare medical miracle that have saved the lives of tens
of millions of people. Disease have been
eradicated, prevented, and the course of infectious diseases has been altered. And even if you are not a physician, everyone
has the experience of taking all of the mandatory vaccinations required to
attend school. Most of these
vaccinations had a significantly worse side effect profile than the currently
available COVID-19 vaccinations.
Apart from reducing rates of infection, hospitalization,
and death these modern vaccinations also reduce the risk of chronicity. Chronic
or “long COVID” symptoms might occur in as many as 70% of patients after the infection.
Remission rates and rates of disability are still being determined at this
time. Given the risk/benefit
considerations of the vaccinations it is difficult to see how any rational
person would refuse it. It is even more
difficult to understand how a rational person would not take basic measures to
protect themselves and their families from airborne virus or justify ignoring
the pandemic on the basis of a completely implausible conspiracy theory. In
some cases, the motivations are very clear.
Politicians would rather use various forms of rhetoric to attack the
idea of a pandemic and what it takes to resolve it for political gain rather
than taking positive steps recommended by experts. It is a standard political
tactic. That rhetoric has been advanced
to extreme levels and to the point where scientists and their families are
being threatened. Today the suggestion
that “white people” were being discriminated against struck me as white
nationalist rhetoric. It was viewed just
as another “falsehood” in the media. Certainly,
blind partisan acceptance of these statements is not very likely to exhibit
flexibility in thinking about the pandemic, the virus, or possible solutions.
The press has stepped in and commented on the process as a
“mass delusion” or “mass psychosis” as if the use of psychiatric jargon by a
journalist would add credibility to the criticism of many people thinking and
acting irrationally. Many of them are agitated, visibly angry, and can become
aggressive typically when confronted about pandemic precautions in schools and
businesses. Hardly a day goes by without
seeing an airline passenger or town hall meeting participant screaming until
they are red in the face and carted away by security. None of these people has
a psychiatric disorder. They can cool off
somewhere, suppress their irrational thoughts and the associated anger, and get
up and go to work the next morning. During the run up to the 2020 Presidential
election there was heated commentary about President Trump’s mental health and
fitness for office. There was some debate in the psychiatric community if it
was appropriate to discuss that issue based on Trump’s observed behavior rather
than a psychiatric assessment. This essay looks at the other side of that
debate. Why do so many people follow leaders who make repeatedly false statements
that in some cases are viewed as potentially inciting people to do the
wrong thing? And conversely – how do so many people accept the more obvious
rational path and reject all of the paranoia and conspiracy theories?
There are of course numerous theories about how this comes
about. The theories generally depend on
the same theories that have been used to describe normal development,
psychopathology, and normal learning processes.
In some cases the theories have a philosophical basis – that seem to be
fashionable these days. And despite many of these theorists incorporating a
neurobiological model – very little explanation about how that is relevant.
The relevance is obvious to me starting with the
relationship between emotion and cognition specifically decision making. In
order for it to be obvious, the relationship between emotions and normal decision
making needs a brief exploration. Human decision making typically occurs as an integrated
process in the frontal cortex. I won’t digress into any subdivisions or tracks
in this post. The key word here is integrated. That means the frontal cortex
takes a large number of inputs and uses them to varying degrees in the ultimate
decision. That includes a lot of memory input, specific types or learning,
emotional input, and real time sensory and perceptual data. The amount of input is large and much of it
occurs at an unconscious level. How it occurs is largely unknown at this point
but with our limiting inputs have been determined. One of those inputs is emotion. We know for
example from lesion studies that emotional input is absolutely critical for
normal day to day decision making. Of the vast number of potential decisions we
all have a subset that are associated with emotional valences that can affect
our preferences. Without access to those valences decision making slows and
grinds to a halt.
Restricting our consideration of the decision space to all
of the possible decisions about the pandemic and how to proceed – all of the
medical, scientific, personal, political, manipulative, and conspiracy theories
the possibilities are very large. If we have 300 million decision makers and
they all have unique conscious states and personal capacities for decision
making the potential outcomes are large. It is also a more complex scenario than
all of the typical explanations for pandemic denial. Each one of our 300 million decision makers
has unique experience affecting the emotional valences of their decisions. The
overt decisions may seem to coalesce at some points but for many different
reasons. For example, believing what a politician says despite the clear
documentation that they are lying can occur as the result of identification
with similar people in the past, identification with a general class attitude
or ethos that it represents, or it simply could be activated by the angry
emotion that politician effects. Those are just a few possibilities.
The pandemic vaccination vs. anti-pandemic antivaxx is by
definition a binary polarized debate – the reality based on what we know about
how the brain works it is far from that simple.
Even on what appears to be the rational side there is no Spock-like
analysis. The public health experts are
all accessing emotion when making their decisions. Rational thought is reward-based
learning and associated to one degree or another with a “Eureka” moment.
The key question going forward is what can be done to
address the degrees of freedom associated with the possible decisions of this
brain process. What can be done to
improve the process and by improve, I mean assure that civilization survives
the current and potentially more lethal pandemics. To that end, there are
numerous cinematic depictions of apocalyptic pandemics. Based on the depictions
prior to this pandemic they are probably fairly accurate. Once a lethal
pandemic takes hold, the decision space for survival collapses as fewer and
fewer decisions are possible. An intuitive writer or film maker knows that at
some level. Time to make it general
knowledge.
George Dawson, MD, DFAPA