Yes – I am Retired
Last January I posed the question ”Are there any good jobs
left for psychiatrists?” Eleven months
later – I have the answer and the answer is NO.
For the past 11 months I have been looking and have seen at least a
hundred jobs descriptions forwarded to me by various people. I have also
interviewed and negotiated a couple of times only to get a contract that was
completely unworkable. I am not an
attorney but I don’t think you have to be when you see a contract suggesting
that you are going to indemnify and hold harmless a large corporation for
any problems that might arise during the course of your employment. I did incorporate that experience into a CME lecture I gave in
November about telepsychiatry and encouraged legal consultation with contracts.
The job postings that I considered were remarkable for the
obvious amount of leverage they would create for employers and some of those
employers had clearly never worked with psychiatrists in the past. What do I mean by leverage? Leverage is bullet points in the job
description. When I started out back in 1986 – job descriptions were
straightforward. I can still recall the
first interview I had at a community mental health center where I was eventually
hired as medical director. They asked me about my treatment philosophy in
psychiatry and my exposure to community mental health. They asked me if I would be comfortable
supervising the community support staff and psychotherapists. I asked them about
the medical resources in the area, where I could do physical examinations if
necessary and where I could get laboratory testing done. All of the stuff psychiatrists are trained to do.
Current job postings list a number of bullet points that
seem irrelevant to the job of a psychiatrist. Things like customer and
stakeholder focus, change management, systems thinking, courage, commitment,
emotional resilience, training (prescribing appropriate medications,
documentation, collaborating with therapists, considerable annual HR rules),
and so on. The term “stakeholder” is
cringeworthy. For 36 years I have treated people who had the toughest psychiatric
and medical problems. All of that treatment was based on establishing a relationship
with the person. In many cases that
involved foreign language interpreters, deaf/hearing-impaired/ASL interpreters,
and various attorneys, advocates, ombudsmen, case-managers, and social workers.
Family involvement is often critical. If
there are any stakeholders besides me and the patient – those would be the
stakeholders. But in the business world – the stakeholders are other businesses
and bureaucrats. They also include middle managers in any business that hires
me. I may go in to work one day and find a team of bureaucrats angry with the
way I am doing things – not from a quality-of-care perspective but from a business
perspective. They may decide to make my life a living hell until I do what they want me to do. All of the irrelevant
bullet points also come in handy at the annual review. A supervisor may
solicit anonymous opinions about whether or not I am fulfilling the requirements
of corporate citizenship irrespective of my work as a psychiatrist. That is all corporate leverage. It has happened too many times and I am done
with it. As far as I can tell that eliminates me from the pool of psychiatrists
eligible for employed positions.
I have considered private practice options and gotten a lot
of advice about it. The problems at this stage are considerable due to the up-front
investment and the issue of tail coverage or malpractice insurance coverage
necessary when I eventually stop working. Establishing a reliable documentation
and medical records system as well as the necessary network security and
insuring that is also a wild card. Private practice seems like an option if I
hit the lottery but not before. It does lead me to give out the advice that starting all of these essentials for private practice earlier in a medical career is probably a good idea. As an example, I have talked with psychiatrists younger than me who have carried their own malpractice policies independent of their employer's policy. That is something I never considered, but today see it as a great idea.
I did a CME presentation in November and I think that went
relatively well. I could do more – but doubt that will ever develop into
anything sustainable. This blog will keep me going in the foreseeable future. I
like reading about psychiatry, medicine, neuroscience, and basic science. I have an interest in staying current as well as knowing where the research is headed. One of the reasons I started this
blog was because I had a significant number of psychiatrists approach me and
ask what I was reading and how I kept up on recent research. This blog has enabled me to reach
psychiatrists around the world and correspond with many on relevant issues. I have never capitalized this blog in order to avoid any appearance of financial conflict
of interest. So, like most retirees I will be living on Social Security income
and retirement savings.
I don’t anticipate many existential issues in retirement
apart from the typical death anxiety from time to time. One of my goals has been to live as long as
possible, and based on my family history I have lived this long just by
avoiding cigarette smoking, exercising, and getting timely medical care. My diet has gradually transformed to a relatively
healthy one. Being married to an
extrovert means that I am never socially isolated. Retirement has resulted in a massive amount of
freedom to finally do what I want.
For decades I was constantly working or worried about work – initially the
patients but eventually the bureaucrats and patients. I also worked too long and
found that I was living somewhat of an alternate existence. I did not know what
it was like to go to a shopping mall in the afternoon – I was working. All of
those daytime everyday activities were available to me during vacations where
most of my time was spent recovering.
The freedom to go to a mall or Target or even to a local coffee shop for
a mocha anytime I want to is something I really have not experienced since the
first two years of medical school. I
plan on using it to the max as the pandemic clears.
Freedom also means much more time. I have about 4,000 books in my library and a
steady stream of incoming subscriptions of medicine and science journals. Not
all of those books were meant to be read cover-to-cover, but I want to make
sure that I read those that were meant to be read that way. At some point I will probably reread Zen
and the Art of Motorcycle Maintenance for a final time. That book is a mysterious
connection to my past as well as one of my all-time favorites.
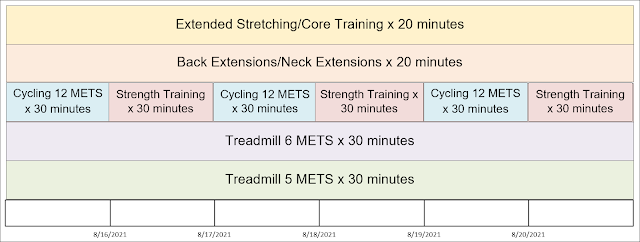
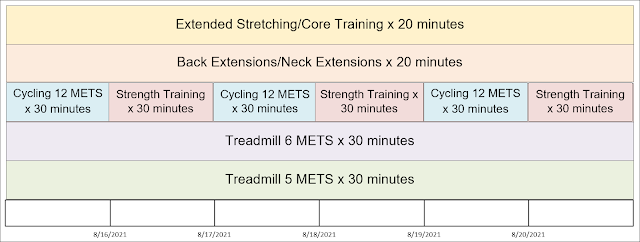
More time for exercise will be a challenge. I decided to
adopt a treadmill strategy for workouts so that when a cardiologist orders
another stress test I will be ready. So far that strategy has worked well. My only limitation is joint pain and back
pain. I think a lot about the day that
pain might not go away and necessitate surgical intervention. This is my
hopeful exercise routine going into retirement (I have actually bumped the 6
MET treadmill routine to 8 METS). The
cycling section is currently on hold after doing about 71 sessions due to a
medical problem.
I plan to push this as far as possible, but the writing is
on the wall based on 4 decades of high levels of activity. The decision about
surgery will depend on how things are going at the time as well as the quality
of consultation. The insight I have developed here is that maintaining high
levels of activity as you age is more than determination. It is a matter of
back and joint preservation and what can be done to restore it, as well as what
other medical problems exist.
The final existential issue in retirement is the one that
many people seem to fear and that is meaningfulness. I can recall running early retirement groups
as part of residency training that were based on that theory, but it was never
evident to me that was really the issue. I certainly have not found any
physicians who found retirement to be a problem. I have a number of goals in place that
involve writing. A senior psychopharmacologist
sent me an email and suggested that I cover mechanisms of action of biological
treatments in psychiatry. I will certainly try to maintain the position of
being an advocate and defender of the profession for the basic reason that
nobody else seems to be willing to do it.
I explain how this has evolved and happened in the
past few decades and the previous post on this blog captures some of my thinking on this
topic. Several papers are in the works on the diagnostic method in psychiatry, rhetoric
used against psychiatry, and sleep transitions.
I am also in the process of outlining a book on diagnostic and treatment
methods in psychiatry. My goal with the book
is too keep it as short as possible and not to get into all of the trivia seen
in typical textbooks. The target audience will be trained, early career
psychiatrists, and like most old people – I hope to pass on some wisdom that
will prevent common mistakes.
Along with the meaningfulness, a few words about ageism
are required here. I have encountered it
in blatant forms in the past 5-10 years from psychiatrists. It bothers me only
in that these psychiatrists seemed to be unaware of their attitude and I have
the position that psychiatrists need to be aware of their biases. To some degree
it is expected of physicians in their 30 and 40s. Medical training encourages competitiveness and
it takes a while to develop a collegial attitude. Is that transition is the same in psychiatry as in other specialties? There are
several reasons why it might be lagging. First and foremost is the constant
barrage of negative and inappropriate criticism the field is under compounded by
the lack of response by any leaders in the field or professional organizations.
That atmosphere encourages people to come forward and say: “I am not like the
rest of the psychiatrists who you are criticizing. Your criticism does not apply to me
and here is why?” That is an attitude I
was explicitly critical of when I started to write this blog but probably did
not articulate that well. I did say that my experience with psychiatrist-colleagues
is that they are thoughtful, professional, and very competent with few
exceptions. I don’t accept the unique psychiatrist defense against
inappropriate criticism even though many authors of these articles come off that way. If the competitiveness and the unique psychiatrist
defense is in the background, does it make ageist biases more likely? I think that it does. I have experienced the comments and the smirks
from people who should have known better – even not counting the obvious
gaslighting comments here on my blog. Psychiatrists should know better.
Another factor are special interest groups like the managed care industry and recertification boards. The managed care industry has emphasized at times that younger physicians are more "managed care savvy" (as if that is a good thing) and the need to train residents with that same goal in mind. The implicit suggestion is that older physicians who generally do not like managed care are less "savvy". Medical boards, after rolling out years of questionable recertification processes and data to suggest that older physicians may know less than younger recertified physicians have apparently come around to the position that a lifelong continuing medical education approach is now acceptable for board recertification. That was where all of this started. In the meantime there has been about 20 years of rhetoric suggesting that older physicians, especially those who were grandfathered in to lifelong certification were self-serving and had less knowledge than the people being run through the recertification mill. In reality, there was not a single older physician who did not believe that lifelong education rather than an arbitrary recertification examination was a superior process. Managed care and the recertification boards were essentially splitting physicians based on age and facilitating ageist biases.
The meaningfulness dimension also includes
collaborating with others. I am currently working with a friend of mind on postmodernism. He happens to be an expert in all things postmodern
and I am running my theory about postmodern rhetoric by him. I hope to collaborate with other researchers
on theory and even experimental design and analysis for a number of problems in psychiatry. I also like making basic
graphics and would consider collaborating on that. I don’t need any
reimbursement for the right projects – authorship credit will do.
The most significant aspect of meaningfulness for many physicians
is realizing how your profession has impacted your family. For too many years, physicians are emotionally involved with strangers often to the point of exhaustion.
That process takes its toll on the people who you are supposed to be the most
emotionally involved with and that is your spouse and your family. The
increased freedom of retirement allows for a fuller realization of that
emotional involvement and reflecting on what has happened over the decades of work.
That is my current retirement process. I will post any
changes here on the blog. I hope there
will be a noticeable improvement in the quality of writing here on the
blog. I know there is information contained
here that can’t be found anywhere else and I am satisfied with that
accomplishment as well adhering to the general goals that I started out with. If anyone reading this has any suggestions
for topics that I should be covering feel free to post it in the comments
section below or send me an email.
George Dawson, MD, DFAPA
Supplementary 1:
With no good jobs being available for psychiatrists what are the options? Unless you can identify a funding source and open up a free clinic there really aren't many. People in my situation can simply retire and I think that many are. In fact, one of my medical school colleagues told me that all it took was the pandemic on top of the current administrative headaches to make that decision. I am sure that somewhere somebody can find a niche and avoid some of the administrative headaches. Learning what it takes for private practice at an early age seems like a possibility but the administrative costs are shockingly high. I recall an internist telling me that for his 2 physician practice they required 3 full time office staff just to handle the billing and coding requirements for hundreds of insurance companies. In my 3 psychiatrist outpatient clinic we needed 1 fulltime staff person to handle phone calls and prescription refills and could have used nurse just to handle the prior authorization calls. The business world has conveniently set things up so that the barrier to private practice is high and it is easier to settle for one of their problematic jobs. I am not sure there is much that can be done to reverse this.
Supplementary 2:
To paraphrase an old automotive commercial: "Quality is no longer job one!" I was a quality and utilization reviewer for psychiatric hospitalizations in both Minnesota and Wisconsin in the 1980s and 1990s. We had stringent criteria for reviewing records and making these decisions. As the federal government invented the managed care industry and turned control over to them including all of the reviewing - quality dropped off the radar. Now what consumers see are media polls of "Top 100" hospitals and curiously most of the hospitals that you drive by seem to have made that list. The same administrative processes that have removed physicians from the decisions about program design and how patients are seen in a clinic have also removed them from monitoring quality and designing quality improvement programs. I know because I have been in the meetings where administrators presented their ideas about quality. They were clearly less knowledgeable about healthcare than Toyota is about producing cars. At least Toyota listens to the people making the cars.
Supplementary 3:
I have always dreamed about working. It is always inside a
massive hospital that is staffed like you would expect a university hospital to be staffed – teams of specialists and
their residents and medical students. None of the buildings look familiar –
they are all brain fabricated and in technicolor. The people in those dreams
all look, sound, and move realistically. The predominate mood in the dream is
anxiety. Some of it is the real anxiety of
everyday medical practice – did I miss anything and have I remembered everything? It is the anxiety that you experience when you are under pressure and on the
edge of being overwhelmed. It is the kind of anxiety that leads to physical
symptoms like accelerated heart rate, palpitations, muscle tension, and
restlessness. Last night (01/08/2022) I dreamed I was in another large medical
center. In this case I was on both a
Renal Medicine team and an Internal Medicine team. I could sense that I was a resident and
paying attention to multiple deadlines and schedules. In real life no resident would do rotations
on both of those services at once. There
is just too much work and it would never happen. I was looking at labs and
notes on Renal patients and figuring out what I needed to do – but then
realized I needed to be on Medicine rounds and started to get increasingly panicked.
I recall thinking that this was an
impossible position and asking myself how that came about. I woke up with a fast heart rate and feeling
anxious but immediately realizing it was just another working dream. Various interpretations
of that dream are possible ranging from the affective tone of the dream (work anxiety)
to possibly wishing I was still at work.
I have definitely experienced elements of both. In medical school Renal
Medicine was one of my favorite rotations and I was one of a few people who rotated
through Renal, Infectious Disease, Cardiology, and Endocrinology in addition to
the required Medicine and Surgery rotations. There was very little that I did
not like about medical school or training. On the other hand it was extremely
stressful and I was never able to lose that stress and anxiety in 35 years of practice.
If anything, the way I practiced tended to increase the stress and anxiety. So
here it is almost a year since seeing my last patient and medicine is still
very much on my mind. With any luck it
will get to the point that I can stop working in my dreams.
Photo Credit: Eduardo Colon, MD