The New York Times came out with an article on prolonged grief disorder. I thought I would write about it because in some ways it is a continuation of the criticism that started with the DSM-5 release in 2015. The response to that piece is one of the most read articles on thisblog. As I pointed out in that article and several since, the release of the DSM-5 has been a predicted non-event. There were no scandalous developments based on releasing a document that hardly anyone reads and is not even owned by most of the people who prescribe medications for psychiatric indications – primary care physicians.
The new piece based on the release of DSM5-TR is much more
balanced. A well-known psychiatric
researcher Katherine Shear, MD is quoted as well as an epidemiologist Holly Prigerson,
PhD who discovered data supportive of the diagnosis and studied the reliability
and validity. Paul Appelbaum, MD is the
head of the committee to include new diagnoses in the manual and he also
explains the rationale.
What did I not like about the article? It starts out with the old saw about how the
DSM 5 is sometimes known as psychiatry’s bible. I appreciate the
qualifier but let’s lose the term bible in any reference to the DSM. That descriptor is wrong at several levels –
the most important one being that it is a classification system. Please refer to it as psychiatry’s phone
book or catalogue from now on, even though it is nowhere near as
accurate as a phone book or any commercial catalogue.
The author goes on to describe the inclusion of prolonged
grief disorder into the latest revision of DSM as controversial and then
collects opinions on either side of what I consider to be an imaginary
controversy. Why am I so bold to call this controversy imaginary? Maybe it is not entirely imaginary, but it
certainly is not as big a deal as it is portrayed in the article and here is
why.
The first argument is that including it in the DSM means
that professionals can now bill for it. In fact, all hospitals, clinics, public
payers, and insurance companies require ICD-11 codes and not DSM codes. Granted, the DSM codes are typically
coordinated to match ICD-11 codes but there is not a perfect match. ICD-11 codes are available for free and do
not require a copy of the DSM 5 TR. The diagnosis of prolonged grief
disorder was included in the ICD-11 in 2020 (2) and it is easier to make
the diagnosis. Quoting from reference 2:
“To meet PGDICD-11 criteria one
needs to experience persistent and pervasive longing for the deceased and/or
persistent and pervasive cognitive preoccupation with the deceased, combined
with any of 10 additional grief reactions assumed indicative of
intense emotional pain for at least six months after bereavement. Contrary
to the 5th revision of the Diagnostical and Statistical Manual of Mental
Disorders [DSM-5; (11)] and
the 10th revision of the International Classification of Diseases [ICD-10; (12)],
the ICD-11 only uses a typological approach, implying that diagnosis
descriptions are simple and there is no strict requirement for the number of
symptoms one needs to experience to meet the diagnostic threshold.”
The insurance company billing is further complicated by the
fact that there are many other current diagnoses that can be used to treat a
person severely incapacitated over a prolonged or severe course of grief. Per my original blog Paula Clayton, MD
explained this 45 years ago based on her research that also showed a small
percentage of people become depressed during grief and require treatment. A
prolonged grief disorder (PGD) diagnoses is not necessary and, in some cases,
may lead to problems with insurance companies. It is well known that some
insurance companies will not reimburse for some diagnoses that they think do
not require treatment by a mental health provider. What they think of a PGD
diagnosis is unknown at this time.
The second argument is that it may lead to biological
treatments for the disorder. They cite a naltrexone trial for this disorder.
Let me be the first to predict that the naltrexone will probably not work but I
will also point out it is a medication that could be prescribed right now
without putting PGD in the DSM 5 TR. The author states this may set off a
competition among pharmaceutical companies for effective medications. That may
be true – but what will the likely outcome be?
We already know that many people with PGD actually have treatable
depression and respond to conventional treatments. We also know that those
medications are all generics, very inexpensive, and the pharmaceutical benefit
managers control most prescriptions for expensive drugs. These factors combined
with the low prevalence of this disorder and well as the responsiveness to psychotherapy
and supportive measure will not produce a windfall for Big Pharma.
There is an inherent bias by some against medical
interventions for any disorder that seems to start out as a phenomenon seemingly
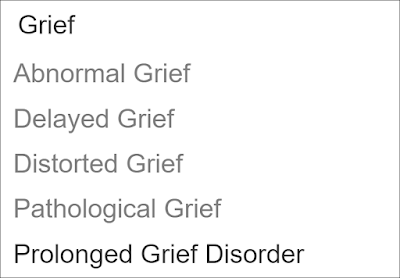
explained by social or psychological factors. Grief was listed as one of the
four major causal factors for depression in Interpersonal Psychotherapy (IPT)
and there were no complaints. IPT has
been around for 40 years. Is that because the treatment emphasized was
psychotherapy? Throughout my career I
have always had resources available for people who were grieving. Clergy are a
professional resource but with the continued secularization of the country it
is common to find that most people do not have an identifiable clergy person.
Grief support groups are very common – both as self-help groups and groups run
by professionals. The question is what if those resources are not enough to assist
the grieving person?
The third argument is that there will be “false positives”
or people given the diagnosis when they are emerging from the symptoms. That
supposes that the doctor has no discussion with the patient about what might be
helpful including non-medical supportive measures and watchful waiting. It also
supposes that the patient’s interest in what is happening with them
specifically how it is affecting their life and whether they want to do
anything about it is never discussed. I
don’t think most doctors – even if they are in a hurry operate that way.
The fourth argument is the danger of making a diagnosis and
how that impacts the person. Grief is a universal phenomenon that everyone
experiences many times in their life. Everyone knows that through experience. Empathically
discussing with a person that this episode of grief is affecting them differently
than others does not seem to be discounting or minimizing their emotions or
experience to me. The very definition of empathy is that the patient agrees
with the empathic statements as adequately explaining their experience.
A fifth argument buried in there is that clinician want to
rapidly classify people so that they can get reimbursement. I have already
addressed each half of that argument about but let me add – does naming a
disorder mean that it did not exist before? There are thousands of examples in medicine
and psychiatry of new diagnoses that basically classify earlier conditions
where the diagnosis was never made before. A striking example from psychiatry
is autoimmune encephalitis. It was
previously misdiagnosed as either a psychosis or bipolar disorder until the
actual diagnosis was discovered. Rapid classification leads to many paths other
than reimbursement. In the case of autoimmune encephalitis – life saving
treatment.
The fundamental problem in writing articles about human
biology from a political perspective is that it fails to address the biology. The
biology I am referring to here are unique human conscious states and all of the
associated back up mechanisms that make them more or less resilient,
intelligent, and creative. Is the general classification “grief” likely to
capture a large enough number of possibilities to qualify as a rigorous definition?
We have known for some time that is not supported by the empirical evidence and
that evidence has become more robust over the past 20 years. A small number of
people experiencing grief will have a much more difficult time recovering and,
in some case, will not recover without assistance. In spite of that, there
remain biases against studies that focus on elucidating biological mechanisms
or treatments. It is easier to invoke emotional
rhetoric like medicalization or psychiatrization and try to avoid the issue. To the author’s credit none of those terms
were used.
There is also the issue of what this new diagnosis suggests
in terms of the science of psychopathology. Does this mean we are closer to
classifying all of the possible problems of the human psyche and developing
treatments? It reminds me of what one of my psychoanalyst supervisors used to
say about the state of the art. In those
days there were basically biological psychiatrists and psychotherapists.
He referred to anyone without a comprehensive formulation of the patient’s
problem as a dial twister. Are we closer to becoming dial twisters? I have some concerns about the checklist
approach associated with the diagnosis and its understudied phenomenology. That
is compounded by the limited time clinicians have to see patients these days
and the predictable electronic health record templates with minimal typing of
formulations.
Practical considerations aside only time will tell if the
new research leads to better identification and treatment of people with clear
complications of grief. That does not mean that science has all of the answers.
It should be clear that the science of prolonged grief disorder like most of
psychiatry only deals with the severe aspects of human experience. There are clearly other ways to conceptualize
grief and learn about it without science. The science is useful for mental
health practitioners charged with providing treatments to the severely distressed and with grief the vast majority of people (90+%) will never see a practitioner and even fewer than that will ever see a psychiatrist.
George Dawson, MD, DFAPA
1: Ellen Berry. How Long Should It Take to Grieve? Psychiatry
Has Come Up With an Answer. NY Times March 18,2022.
2: Eisma MC, Rosner
R, Comtesse H. ICD-11 Prolonged Grief Disorder Criteria: Turning Challenges
Into Opportunities With Multiverse Analyses. Front Psychiatry.
2020;11:752. Published 2020 Aug 7. doi:10.3389/fpsyt.2020.00752
Excerpted per open-access article distributed under the
terms of the Creative Commons Attribution License (CC BY).
3: Prigerson HG,
Horowitz MJ, Jacobs SC, Parkes CM, Aslan M, et al.
(2013) Correction: Prolonged Grief Disorder: Psychometric Validation of
Criteria Proposed for DSM-V and ICD-11. PLOS
Medicine 10(12): 10.1371/annotation/a1d91e0d-981f-4674-926c-0fbd2463b5ea.
4: Lenferink LIM,
Eisma MC, Smid GE, de Keijser J, Boelen PA. Valid measurement of DSM-5 persistent
complex bereavement disorder and DSM-5-TR and ICD-11 prolonged grief disorder:
The Traumatic Grief Inventory-Self Report Plus (TGI-SR+). Compr Psychiatry.
2022 Jan;112:152281. doi: 10.1016/j.comppsych.2021.152281. Epub 2021 Oct 21.
PMID: 34700189.
5: Shear MK,
Reynolds CF, Simon NM, Zisook S. Prolonged grief disorder in adults:
Epidemiology, clinical features, assessment, and diagnosis. In Peter P
Roy-Byrne and D Solomon (eds) UpToDate https://www.uptodate.com/contents/prolonged-grief-disorder-in-adults-epidemiology-clinical-features-assessment-and-diagnosis#H210445955
accessed on 03/21/2022
6: Klerman GL,
Weissman MM, Rounsaville BJ, Chevron ES.
Interpersonal Therapy of Depression.
Basic Books, New York, 1984.
7: Ratcliffe M. Towards
a phenomenology of grief: Insights from Merleau-Ponty. European Journal of Philosophy 2019; 28:
657-669 DOI: 10.1111/ejop.12513
8: Clayton PJ. Bereavement in Handbook of Affective of Disorders. Eugene S. Paykel (ed). The Guilford Press. New York. 1982 pages 413-414
Supplementary 1:
Quote from an initial post on this subject 9 years ago as written by Paula Clayton, MD:
"There are many publications that deal with treating psychiatric patients who report recent and remote bereavement. It is possible to find a real or imagined loss in every patient's past. However, for the most part, because there is little evidence from reviewing normal bereavement that there is a strong correlation between bereavement and first entry into psychiatric care, those bereaved who are seen by psychiatrists should be treated for their primary symptoms. This is not to say that the death should not be discussed, but because these people represent a very small subset of all recently bereaved, they should be treated like other patients with similar symptoms but no precipitating cause. A physician seeing a recently bereaved with newly discovered hypertension might delay treatment one or two visits to confirm its continued existence, but treat it if it persists. So the psychiatrist should treat the patient with affective symptoms with somatic therapy but only if the symptoms are major and persist unduly. A careful history of past and present drug and alcohol intake is indicated. Then, the safest and most appropriate drugs to use are the antidepressants. Electroconvulsive therapy is indicated in the suicidal depressed." (Paykel p413-414)
The pervasiveness, persistence, and pathological qualities mandated by the SCID examination are still the best way we have of distinguishing depressions that have more of a pathological physiology (major depression) from those which appear to be, to use the old term, more functional (dysthymia). The first responds best to antidepressants usually, and the latter to psychotherapy. Sometimes it is hard to tell the difference due to symptom overlap, but not usually. Our brain science simply is not yet good enough to use as a diagnostic tool. Clearly, severe psychological stressors can trigger an episode of major depression, which I think is what you seem to imply when you talk about a grief reaction turning into major depression.
ReplyDeleteThe dichotomy between biological psychiatrists (dial twisters?) and psychotherapists reminds me of other medical subspecialty divisions and the difficulty of integrating medical and psychological diagnostic and treatment formulations into daily clinical practice. I wrote a blog post from my previous blog (The Practical Psychosomaticist) with the title “The Time has Come for 'Ergasiology' to Replace 'Psychosomatic Medicine?' “Ergasiology” was a word coined by Adolph Meyer and emphasized the combination of biological, social, and psychological factors operating in patients—yet favored the view that mental illness didn’t have anything to do with brain dysfunction. My post was tongue-in-cheek but Psychosomatic Medicine changed its name in 2016 to something which fit what we actually do—Consultation-Liaison Psychiatry (CLP)—which Don R. Lipsitt was pleased about. He wrote Foundations of Consultation-Liaison Psychiatry: The Bumpy Road to Specialization (2016). The road to integrating medicine and psychiatry continues to be very bumpy.
ReplyDeleteJim - Interesting that you should mention it - I started reading Pathologist of the Mind by SD Lamb at the suggestion of a Hopkins psychiatrist who mentioned that Ch 1 was required reading by their residents. It is the biography of Meyer. It is part of my project to construct a realistic timeline of how psychiatry came to be in the US. I also got a preview of an outstanding paper looking at the issue of neuropsychiatrists and will post here on that paper when it is published.
Delete