I generally try to keep my research and posts confined to medical and scientific journals for a couple of reasons. First and foremost is that well documented bias against psychiatrists and whatever version of monolithic psychiatry that authors and editors in the popular media choose to embrace. Secondly, the information content of professional journals is much higher and the theories and concepts are what I have been studying for decades at this point. For the purpose of this post, I am making an exception and will be writing about a story from the New Yorker about hallucinogens (1).
Being child of the 1970s and a psychiatrist starting a
short time later, I have had plenty of academic and professional experience
with hallucinogens. Given that
experience, I am very skeptical about how the new wave of hallucinogens have
been portrayed as a panacea for psychiatric problems. Even more problematic is the portrayal that
these compounds are generally well tolerated and have no significant adverse
effects. I will be the first to acknowledge that there is a selection bias.
People don’t end up coming to see me because they had a good experience with
hallucinogens. They see me because they had a very bad experience and that is
generally severe anxiety, panic attacks, and hallucinogen persisting perceptual
disorder (HPPD). HPPD is a permanent change in perception after exposure to
hallucinogens. That can range from looking
down and seeing the carpet moving continuously to noticing that there are
trailers streaming from objects moving across your visual field.
If you research HPPD or hallucinogen side effects –
relatively little turns up in the medical literature. There are probably less
than 100 papers written on HPPD since the 1960s. They are typical case reports, anecdotal
treatment, and a call for more research on treatment. A major LSD study
documenting disability had to wait until recently for an analysis of side
effects. I contacted 2 current
hallucinogen researchers and asked them for a copy of the consent form they are
using for their research projects in order to see what adverse effects their
were advising their patients about. That was two years ago and I have yet to
receive a reply. It is against this backdrop that I am going to present some
concerns noted in the New Yorker article.
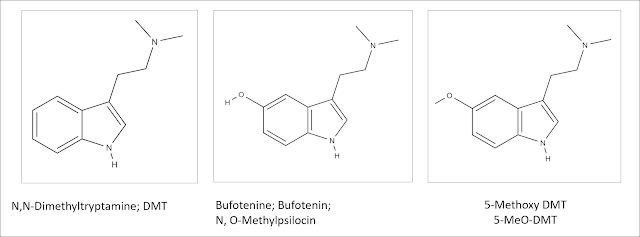
The bulk of the story involves a trained Mexican physician
who first gained some fame in 2013 when he gave a testimonial about overcoming
crack cocaine addiction by using a psychedelic produced by the Sonoran
Desert Toad – Incilius
alvarius. This
toad is in the family of true toads or Bufonidae and
that may be why the toad is also referred to as Bufo alvarius using an
incorrect genus name. The Sonoran Desert
extends through southern Arizona and California and along either side of the
Gulf of California down the Baja Peninsula on the West and contiguous Mexico on
the East. This toad secretes a toxin to
protect against predators. The article points out that dogs have died as a result of this toxin. The toxin has
been analyzed and it contains 5-methoxy DMT – the psychedelic claimed to treat
the addiction. Since the research literature uses the abbreviation 5-MeO-DMT
that is how I will refer to this compound. The usual superlatives are
used to describe the psychedelic experience. Endorsements from celebrities are
there endorsing the spread of toad medicine around the world. The actual experience is described in eerie
terms like: “completely dissolves reality as we know it” or “terror and a sense
of ego dissolution” followed by what is described by uncertainty over what
happened along the way. I have
abstracted the side effects listed in this article in the table below.
|
5-MeO-DMT Adverse Effects |
|
|
General |
Pain Shortness of breath |
|
Cardiovascular |
High blood pressure Tachycardia |
|
Neuropsychiatric |
Flashbacks Extreme anxiety Hyperventilation Insomnia
|
|
Intoxication |
Agitation Aggressive behavior Vomiting |
|
Death |
The article lists
about 6 deaths that occurred while smoking 5-MeO-DMT
– one of these deaths was attributed to anaphylaxis |
The main focus of the article is a single practitioner who is described as actively promoting this treatment and at the same time is considered problematic for inadequate monitoring of the patients he treats with 5-MeO-DMT. Doses are approximate, patient monitoring is lax to non-existent, and he has run into some legal problems, problems with practitioners of ethnic medicine, cultural problems with a local tribe, and ecological problems due to toad depletion. Against that backdrop are the usual testimonials that 5-MeO-DMT has cured intractable substance use problems and psychiatric disorders like depression and PTSD. There are also examples of substance use problems getting worse to the point of a fatality and the whole experience of causing PTSD as well as alleviating it. Expert opinion is included with the usual qualifiers about how clinical trials might provide clearer answers and venture capital funding being available for depression trials.
After reading the New Yorker article I went to
ClinincalTrials.gov and found 5 5-MeO-DMT current studies listed. Three appeared to be safety studies in normal
volunteers and one of these studies was a dose ranging study. There was another
study for treatment of depression. Three studies were completed with no results
available. The fifth study was not yet
recruiting subjects.
By way of contrast, I thought I would look at a paper that
surveyed subjects who had taken 5-MeO-DMT (3) at least once especially for the side
effect profile. This study used an
anonymous Internet survey to look retrospectively at the epidemiological
features of people who have used this compound. The study design is limiting in
this case because it likely screens for people who have had positive
experiences and in this case may be motivated to promote psychedelics (the
incentive for subjects was a very modest donation to an organization that promoted the study
and use of psychedelics. The researchers collected demographic data, data on
5-MeO-DMT and other substances used, patterns of use and the effects of use
(Mystical Experiences Questionnaire/MEQ) (4) and possible side effects through the
Challenging Experiences Questionnaire/CEQ (5) that was apparently designed to study
the challenging experiences associated with taking hallucinogens. I encourage
reading the entire paper for all of the details. The final version of the CEQ
is 26 items that have been factor analyzed to measure fear, grief, physical distress,
insanity (fear of losing one’s mind on a sustained basis), isolation, death,
and paranoia.
The authors basically conclude that users of 5-MeO-DMT do
in fact experience mystical experiences per the MEQ. The MEQ was originally studied for
hallucinogen experiences and the specific questions can be found in reference 4
as well as the body of reference 3. It is probably not surprising that a
hallucinogen creates a mystical experience.
The poll here suggests that it may be more intense than the subjects
experienced with other hallucinogens. At one point in the paper the authors
suggest that the mystical experience is thought to be curative, but that is
really unclear at this point. If it is true, the duration of the cure is also
unclear. From the New Yorker article there were testimonials that 5-MeO-DMT was
useful for substance use and some other psychiatric disorders – but there was
also a question of worsening.
Although this was not a clinical trial, medical literature typically describes adverse effects or adverse drug effects (ADEs) from any medical intervention used to elicit a specific therapeutic effect. Those ADE checklists are used to assess safety as well as producing the warning and side effect literature for the package insert of approved medications. The literature on psychedelics seems to have taken the direction that the focus should be on what are described as psychological effects (see second column in the following table under neuropsychiatric side effects). This is problematic because it seems to assumes that discrete bodily systems (other than the brain and perhaps the heart) are not involved with potential drug related side effects. The term side effects and adverse effects tend to be avoided other than to say that some people may have an adverse effect from the psychedelic experience. The New Yorker article and even the survey of 5-MeO-DMT users suggests that medical safety is a potential concern and that no matter what the setting a person needs to be carefully monitored after ingestion of this drug.
|
5-MeO-DMT Adverse Effects (References
3,4,5) |
||
|
General |
Pain Shortness of breath Nausea |
|
|
Cardiovascular |
High blood pressure Tachycardia |
|
|
Neuropsychiatric |
Flashbacks Extreme anxiety Hyperventilation Insomnia Fear Hallucinations Dissociation
|
Depersonalization Aggression Violence Confusion Paranoia Grief Insanity Isolation Death Paranoia |
|
Intoxication |
No clear distinction |
|
|
Other |
|
|
A reasonable summary of what is known about currently known
this drug at this point is that it is a powerful hallucinogen. The safety and
efficacy of this drug is currently unknown. Caution is required in looking at a
survey study where the primary interest in taking the drug is wanting a
mystical experience and treatment of a psychiatric disorder is a secondary
effect and yet the psychiatric disorder tends to improve. The New Yorker article is a cautionary
tale and a counterpoint to a lot of the hype around hallucinogens right now
that includes travelling to a foreign spa and having it administered by a self-proclaimed
guru. The deaths mentioned in that article and some places in the literature
are another red flag in contrast to the universal proclamations about hallucinogen
safety. People with complications and severe outcomes don’t generally participate
in surveys – therefore surveys are not the best ways to determine how a toad
toxin can be used on a therapeutic basis.
It always seems to come back to controlled randomized clinical
trials that are carefully optimized for patient safety. I have been the
medical person responsible for the safety of patients in many of these trials
and that typically involves weekly visits with physical examinations and any
indicated labs. It is a tedious and
expensive process and there are no good short cuts. Until then I advise extreme
caution with hallucinogens or psychedelics. It is always good to keep in mind
that human biology varies greatly. What some people tolerate without a problem
for years can cause severe side effects or even death for others. I expect that
will eventually be documented for hallucinogens.
George Dawson, MD, DFAPA
Supplementary 1: For past links to posts here on hallucinogens please see the following:
Are Hallucinogens the New Miracle Drugs: https://real-psychiatry.blogspot.com/2016/06/are-hallucinogens-new-miracle-drugs.html
JWH Compounds Make the NEJM: https://real-psychiatry.blogspot.com/2017/01/jwh-compounds-make-nejm.html
References:
1: De Greef K. Toad Smoke. New Yorker. 2022 Mar 28: 38-45.
2: Larsen JK. Neurotoxicity and LSD treatment: a follow-up
study of 151 patients in Denmark. Hist Psychiatry. 2016 Jun;27(2):172-89. doi:
10.1177/0957154X16629902. Epub 2016 Mar 10. PMID: 26966135.
Revisits the Danish LSD Study and concludes
that “Most of the patients suffered from severe side effects of the LSD
treatment many years afterwards.”
3: Reckweg JT, Uthaug MV, Szabo A, Davis AK, Lancelotta R,
Mason NL, Ramaekers JG. The clinical pharmacology and potential therapeutic
applications of 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT). J Neurochem. 2022
Feb 11. doi: 10.1111/jnc.15587. Epub ahead of print. PMID: 35149998.
4: Maclean KA,
Leoutsakos JM, Johnson MW, Griffiths RR. Factor Analysis of the Mystical
Experience Questionnaire: A Study of Experiences Occasioned by the Hallucinogen
Psilocybin. J Sci Study Relig. 2012 Dec;51(4):721-737. doi:
10.1111/j.1468-5906.2012.01685.x. PMID: 23316089; PMCID: PMC3539773.
5: Barrett FS,
Bradstreet MP, Leoutsakos JS, Johnson MW, Griffiths RR. The Challenging
Experience Questionnaire: Characterization of challenging experiences with
psilocybin mushrooms. J Psychopharmacol. 2016 Dec;30(12):1279-1295. doi:
10.1177/0269881116678781. Epub 2016 Nov 17. PMID: 27856683; PMCID: PMC5549781.
“…challenging psychological experiences during
the acute effects of psychedelics are not uncommon.” p. 1279
6: Murdaugh LB. Adverse drug reaction reporting. In: Competence
Assessment Tools. 2015. American Society of Health-System Pharmacists. Bethesda, MD.
Accessed Online: https://doi.org/10.37573/9781585284030.040
Great post. I just saw an article in The Daily Iowan (“Opinion: Iowa Lawmakers missed an opportunity to prepare Iowans for the future of psychiatry” by Gabe Conley). This was published just last year, March 7, 2021. It’s about psilocybin being promoted as a psychiatric treatment and calling for moving it out of its current Schedule I drug classification. Would it be worthwhile for you to update your post from 2016, “Are Hallucinogens the New Miracle Drugs?” Jim Amos MD
ReplyDeleteThat's a great idea Jim. I think looking at how the category has morphed over the years and then the specific evidence about the clinical use of these compounds is probably a good idea. It also happens to be a massive project - but one that is probably worthwhile. I continue to respond to the theme that these compounds are benign and the papers that the popular press gets these ideas from. That is what I liked about the New Yorker article - it is one of the few that discusses the downside.
DeleteI've been highly skeptical of the hype surrounding hallucinogens for a long time - glad to see this article.
ReplyDelete