I will address this issue one final time. I have written about it in the pages of this blog in past. Drapetomania was a pseudo diagnosis coined by Southern physician named Samuel A. Cartwright. He wrote the following in 1851:
“DRAPETOMANIA, OR THE DISEASE CAUSING NEGROES
TO RUN AWAY.
It is unknown to our medical authorities, although its diagnostic symptom, the
absconding from service, is well known to our planters and overseers...
In noticing a disease not heretofore classed among the long list of maladies
that man is subject to, it was necessary to have a new term to express it. The
cause in the most of cases, that induces the negro to run away from service, is
as much a disease of the mind as any other species of mental alienation, and
much more curable, as a general rule. With the advantages of proper medical
advice, strictly followed, this troublesome practice that many negroes have of
running away, can be almost entirely prevented, although the slaves be located
on the borders of a free state, within a stone's throw of the abolitionists.”
Characterizing running away from slavery as a disease and
physical punishment as a treatment was certainly a radical concept even
in the Southern states before the American Civil War. In subsequent paragraphs
Cartwright invokes divine providence to explain why white masters are destined
to remain in a superior role to slaves.
He was concerned about “two classes of person who were apt to lose their
negroes – the overly permissive defined as “treating them as equals” and the
cruel owners who denied slaves the ordinary necessities of life. His solution was to treat them well enough,
but not allow many freedoms, and physically punish them into a submissive state
“for their own good.” Since Cartwright
wrote these paragraphs the common interpretation is that his disease
characterization of a rational act is a prototypical misapplication of the
disease concept.
Not much has been written about criticism at the time.
Writing in the Buffalo Medical Journal Samuel Hunt provided a satirical
editorial on the original paper (2):
“Our purpose in this formal introduction, is to give due
importance to an article recently published in its pages by Dr. Samuel
Cartwright, of New Orleans. Characterized by the same cautious induction and
logical accuracy whichever attended the literary efforts of that gentleman, it
deserves careful consideration of the medical philosopher, the anatomical
statesman, and the benighted Saratoga convention.
Those of our readers who are in the habit of referring to Cullen’s
Nosology for the definition of diseases, will find no mention there of
Drapetomania. The ignorance of the ancients was surprising, and we need but
refer to Drapetomania as an evidence of this progressive spirit of the age in
which we live.
Dr. Cartwright has conferred this name, Drapetomania, upon
a disease peculiar to the south, and which is, we believe entirely confined to
that section, and only manifested at the north in certain analogous if not
identical forms, which we shall have occasion to mention when we have given our
readers time for the perusal the following extract from Dr. Cartwright’s able
article:”
After additional sarcasm following the extract, the author
goes on to close his editorial by describing a disease he calls Effugium discipulorum or a tendency of school
boys to leave school and spend time in the fields and orchards of rural
districts. He suggests that the same solution – whipping “have been sanctioned
by ages of experience in Effugium discipulorum; thus confirming the allied
nature of the 2 diseases and the correctness of Dr. C’s hypothesis.” Hunt’s
satirical editorial of 1855 and additional sources describing how the paper was mocked in the northern states is an indication of how serious this
“diagnosis” was taken by some physicians at the time.
Historian Christopher D. E. Willoughby (3) described a much
more nuanced environment and the multiple roles that Cartwright played. He was
apparently widely published on a number of medical topics and there was widespread
interest in the medical community about racial differences in medicine.
Cartwright portrayed himself as an expert in this area, but due to his
reputation he generally received deferential treatment – even when other
physicians disagreed with him. The
medical emphasis at the time was on anatomy and in terms of disease theory there
was a doctrine of specificity outlining the few factors relevant to how
a disease could be treated. One of those factors was race. A physician could be
regarded as a quack if one of these factors was disregarded – reinforcing the
role of racial medicine. Despite Cartwright’s medical and political role,
Willoughby describes his drapetomania as being so far outside of the
medical norms at the time that drapetomania was not adopted as a diagnosis by
many physicians and it was never a psychiatric diagnosis for the obvious reason
that psychiatry and its diagnostic systems did not exist.
.The sampling of how often the term was used over the
intervening decades both independently and relative to actual psychiatric
diagnoses is indicated in the following Google NGRAMS. To read about the graphing procedure consult
this source (4). (Click to enlarge)
A critical question is how a theory largely ignored at the time, now has more references than in the past? A lot of that may have to do with a reinterpretation of his image. The description of him as a respected surgeon who trained with Benjamin Rush at Pennsylvania Hospital was apparently due to mistakes in an early biographical history (3) and persist today in Wikipedia and many other places. Further reading suggests that he was in medical school as a teenager, dropped out to fight in the War of 1812 where he sustained injuries and then went back to complete his medical training. Looking at that timeline does it seem plausible? (click to enlarge)
What about the purported connection between psychiatry and Cartwright and his invented diagnosis? Per the timeline above psychiatry had not yet been invented. There was an organization of asylum superintendents at the time but they had no formal diagnostic system. The Association of Medical Superintendents of American Institutions for the Insane (AMSAII) was founded in 1844 and it had a total of 13 members - none of them were described as psychiatrists or alienists. Despite the fact that racism and proslavery attitudes were widespread, none of them used the term drapetomania or admitted asylum patients on that basis. In fact, only one asylum accepted slaves with mental illnesses at that time.
The American Medico-Psychological Association was established in 1892 and at that time the number of alienists versus psychiatrists was not known. In fact, it wasn’t until a meeting of the Alienists and Neurologists of America in 1917 (7) that anyone suggested specific training was necessary to treat asylum patients. In those proceedings there are three times as many references to alienists than there are to psychiatrists, despite Reil’s first use of the term in 1816. No mention at all of drapetomania but an interesting section on the importance of social diagnosis and social work. The main diagnostic focus was on alcoholism, catatonia, epilepsy, syphilis, dementia praecox, various forms of chronic illness, and intellectual disability described as “feeble mindedness”. None of the alienists or neurologists seem remotely concerned about drapetomania. This is the only reference to race in that 228-page document:
“Preservation of self and of the race are directly
dependent upon gratification of the appetites and this fact necessitates
reaction of man to his environment and appropriation of those things which
serve to fulfill his desires.”
It was included in a section on “Criteria of Defective
Mental Development”.
On the timeline, the initial forms of psychiatric
diagnostic manuals appeared in 1918 and 1952. Neither contained any reference
to drapetomania and most of the diagnoses proposed are recognized as being
similar or precursors to current diagnoses. One of the often-used tactics in
criticizing psychiatry today has to do with the diagnostic manual and what it
means. Contrary to the rhetoric, alienists
and psychiatrists involved in asylum care were often criticized for the lack of science
in those settings most notably by the neurologist Weir-Mitchell (8):
“I shall frankly have to reproach many of those
who still bear the absurd label of ‘medical superintendents'. Where are your annual
reports of scientific study of the psychology and pathology of your patients? We
commonly get as your contributions to science, odd little statements, reports
of a case or two, a few useless pages of isolated post mortem records and these
are sandwiched among incomprehensible and farm balance sheets”. He went on to state that neurologists believed
asylum care was care of “last resort”.
From the start psychiatric diagnostic manuals had the dual
role of diagnostic description and data collection in asylums, specialty hospitals,
specific populations, and for research purposes. Contrary to modern
antipsychiatry philosophy there was no goal to increase diagnoses or the number
of people with a diagnosis and no goal of social control through diagnosis.
I have established that Cartwright had no connection to
Benjamin Rush of the University of Pennsylvania medical school. I have also
established that drapetomania was certainly not accepted as a diagnosis and was
probably widely derided in some areas.
It was essentially a product of the racist south, inadequate diagnostic theory and medical racism, had medical and political implications, and was
written by a physician who owned 14 slaves and had a personal interest maintaining that practice. I have also established that it has
nothing to do with the field of psychiatry or its intellectual roots. It is
only through massive misinformation that these false ideas persist. That
misinformation landscape if so large at this point that it is not likely to
ever be corrected. I certainly doubt that this blog will have much of an effect
against what is now decades of drapetomania misinformation. Many of the people spreading that misinformation
are doing it in bad faith and by definition are not interested in correcting
it. There are also many (presumably) good faith errors such as recent statements from within organized psychiatry and in texts. A psychology colleague posted that every undergraduate Abnormal Psychology text uses drapetomania as an example of coercive psychiatry. Hopefully the good faith errors will correct themselves.
The modest goal of this post is to hope that I can keep all
of this misinformation out of the psychiatric literature. That will be no small task. Szasz is already
published despite the fact that he has been widely discredited. Even last month
I was reading the American Journal of Psychiatry (9) and came across
this statement:
“Over 60 years after the ratification of the US
Constitution, physician Samuel Cartwright played a prominent role in the rise
of racism in psychiatry. His
descriptions and characterizations of mental health conditions in enslaved
Africans, particularly drapetomania which he described as the illness of
enslaved people wanting to run away and escape captivity, and dysaethesia
aethopica, a disease of ‘rascality’, were the beginning justifications of
pathologizing normal behavioral responses to trauma and oppression.”
Based on everything I have established this is an
inaccurate statement. Cartwright was not a psychiatrist or even an alienist. He
was not trained in researching or diagnosis any mental health conditions and essentially made
these up. His isolated racist ideology has nothing to do with the subsequent
development of psychiatry or the way psychiatry is practiced today. Cartwright
and drapetomania have become a convenient meme with the imitators using it as
an indictment of psychiatry or the psychiatric diagnostic system – even though
it is unrelated to both. The latest
application has been the use of this meme by psychiatrists to acknowledge systematic
racism within the field as a basis for future correction. I have no problem
with acknowledging that racism in psychiatry and society exists – but let’s make
that acknowledgment on a realistic basis not an unconnected anecdote.
I expect a fair amount of opposition to this post. I base
that on a reaction I got in a psychiatry listserv when I suggested that
professional organizations should suggest the Rosenhan paper be retracted.
Although I got several very supportive replies and replies from people who were
shocked about the facts, there was also a very vocal contingent proclaiming
they want social justice. Social justice cannot be predicated on a misinformation,
even if that misinformation seems consistent with your overall message. And there is a much better way. That better way was in this weeks
New England Journal of Medicine (10) in an article highlighting the work
of W.E.B. Dubois and his colleagues who accomplished what can only be described
as landmark work in the area of structural racism. In it DuBois and colleagues
concluded that the excess mortality from tuberculosis in the black community
was a product of racial disparities secondary to social forces. The report was
published in 1899. DuBois also
successfully countered the theory of an insurance company actuary who suggested
that black people were “ill adapted to freedom but also doomed to imminent
extinction because of their biological differences from white people.” (note
the parallels with drapetomania). Dubois successfully refuted these claims and
showed that heredity could explain only a small part of differential mortality between
groups and that social inequity accounted for most differences. The work of
these social scientists and theorists is a solid place to start.
The solid scientific ground that we are on today is that we
know race is a non-specific factor and that biologically all of mankind comes from
the same place. We are much more biologically similar than different. Discrimination
and the resulting outcome disparities based on racism are the real problems to be
addressed and there has been a scientific basis for that since 1899.
George Dawson, MD, DFAPA
References:
1: Cartwright
SA. Diseases and Peculiarities of the
Negro Race. De Bow's Review. Southern
and Western States. Volume XI, New Orleans, 1851 Link
2: S. B. Hunt
(1855). "Dr. Cartwright on "Drapetomania"". Buffalo Medical
Journal. 10: 438–442. (full text). https://books.google.com/books?id=coBYAAAAMAAJ&pg=PA438#v=onepage&q&f=false
3: Willoughby
CDE. Running Away from Drapetomania: Samuel A. Cartwright, Medicine, and
Race in the Antebellum South. Journal of Southern History
The Southern Historical Association Volume 84, Number 3, August 2018 pp.
579-614; 10.1353/soh.2018.0164
4: Younes N, Reips
UD. Guideline for improving the reliability of Google Ngram studies: Evidence
from religious terms. PLoS One. 2019 Mar 22;14(3):e0213554. doi:
10.1371/journal.pone.0213554. PMID: 30901329; PMCID: PMC6430395.
5: Szasz TS. The sane slave. An historical note on the use
of medical diagnosis as justificatory rhetoric. Am J Psychother. 1971
Apr;25(2):228-39. doi: 10.1176/appi.psychotherapy.1971.25.2.228. PMID: 5553257.
6: Fried S. Rush:
Revolution, madness & the visionary doctor who became a founding father.
Crown Publishing Group, a division of Random House LLC; New York, 2018.
7: Alienists and Neurologists of America: Proceedings of
Sixth Annual Meeting. Chicago, IL July 10-12, 1917.
8: Shorter E. A History of Psychiatry: from the era of the
asylum to the age of Prozac. John Wiley
& Sons, Inc. New York, 1997: p.68
Weir-Mitchell’s criticism was delivered in 1894.
9: Shim RS. Dismantling Structural Racism in Psychiatry: A
Path to Mental Health Equity. Am J Psychiatry. 2021 Jul;178(7):592-598. doi:
10.1176/appi.ajp.2021.21060558. PMID: 34270343
10: White A, Thornton
RLJ, Greene JA. Remembering Past Lessons
about Structural Racism — Recentering Black Theorists of Health and Society. New England Journal of Medicine August 26,
2021 385(9):850. doi: 10.1056/NEJMms2035550
11: Callender JH. History and Work of the Association of Medical Superintendents of American Institutions For The Insane - President's Address. Am J Insanity. July 1883: p. 1-32.
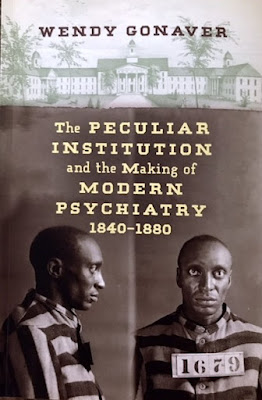
In this reference, the Association President reviews the first 40 years of progress and points out that 13 members started in 1844 but by 1880 there were 115 members representing 130 public and private institutions in the US or Canada and a total of 41,000 patients. In this same document the President refers to the distinguished members of the organization as alienists rather than psychiatrists. Gonaver (see below) refers to the physicians of the AMSII as "asylum doctors" or "psychopathists" but also points out that many had no specialized training at all in the treatment of the mentally ill.
Supplementary 1:
This reference was posted to me on Twitter. In it the author points out that the term drapetomania was not a diagnosis in the only asylum that treated slaves during the time when there was peak interest in the term:
"Readers may be therefore surprised by the conspicuous absence of these so-called conditions in the only insane asylum in which slaves were patients."
Gonaver W. The Peculiar Institution and the Making of Modern Psychiatry, 1840–1880. University of North Carolina Press, 2019.The ELA itself was housed in an inadequate physical plant
even in the pre-Civil War era. Sanitation was clearly a problem with inadequate
drainage and sewerage systems. Potable water was also problem. There were a
large number of fires on the campus for heating purposes until central heat
could be installed. Nutrition was also a problem. Although the patients got
about a pound of meat 5 days a week and fish 2 days a week several patients
were diagnosed with scurvy. That led to an emphasis on expanded gardening of
fruits and vegetables. Children of staff living on campus were not served regular meals but had to subsist on scraps.
One obvious conclusion is that there is much material in this book that could be used to blame psychiatry in much the same way that drapetomania has been used. But there are many qualifiers. Racism both overt and covert were clearly present in both the northern and southern states. Even though much of the events described in this book occurred 30 – 70 years after Benjamin Rush’s death there were no true abolitionists, not even reformer Dorthea Dix. John Galt supported his enslaved staff in many cases humanistically but from a pragmatic rather than a moral perspective. He clearly believed that blacks were socially and intellectually inferior, but he realized that his institution could not run without enslaved blacks. That led him to defend the quality of care provided by the enslaved staff at his institution. Racial stereotypes cut across the dimensions of religion, gender, and culture with African Americans receiving the harshest treatment and the greater work load. When John Galt died and the Civil War ended, the integrated ELA also ended and black patients were transferred to a segregated institution where their care was noticeably worse. During a transition period, multiple military physicians with no training in asylum care were appointed to run the ELA.
Politics factored prominently in the workings of the ELA
and whether Galt received any recognition for his work of ideas. Shortly after his arrival, a conflict
developed with the asylum board when they removed his hiring ability and blamed
him for the resulting problems. He was also resented by AMAII colleagues over
his advocacy for integrated asylums and eventually an outpatient community-based
model. Despite praise for innovation at their meetings he was never credited
for his ideas or his death mentioned in one of their meetings.
The author is a critical presence in this book. In places,
she is clearly suggesting that stressors, abuse, domestic violence, war, and
other forms of trauma may be the most important factors in why someone, but
particularly white, black, and enslaved black women ended up in the ELA. She
acknowledges that there may be a role for severe post-partum states. As I read
though these case reports, I had questions about the degree of detail available
as well as the primitive to non-existent diagnostic system. If all of the
details of stressful events were there – could they really not be considered
given the primitive state of medicine that was being used? The only treatment being supplied was
basically moral therapy and environmental containment to reduce the risk of
aggression, suicide, and starvation.
There were no trauma or stress based therapies available in the mid-19th
century. If there were it would take a much larger professional staff to
administer them.
All things considered, the logical conclusion is that the
ELA, like most institutions was not able to rise above the prejudices of the
population where it was located. The practices described in the book are common
overt and implicit racist themes – even today. Covert segregation still exists
even though school segregation ended in 1954. In keeping with the timeline of this
book, the Civil Rights Act of 1875 was supposed to have ended racial
discrimination but the Supreme Court overturned it in 1883 saying that
individuals and private business could discriminate on the basis of race.
The Peculiar Institution is a
very scholarly work. It is well written and I encourage anyone with an interest
in the history of this time or discrimination based on race or gender to read
it. My only other concern is with the
extended title – The Making of Modern Psychiatry. I would submit that it really contains very
little to do with modern psychiatry – and like Cartwright’s drapetomania
diagnosis is more the product of racism, politics, and an inadequate system of
care.
Supplementary 6: