Saturday, June 18, 2016
Being Suicidal - The Conscious State
The assessment of potential for suicide is a large part of a psychiatrist's work. Within the past decade these footnotes have popped up even in algorithms that are designed to guide decisions about psychopharmacology. They have always been present in treatment guidelines for most major psychiatric disorders. They are a major cause of anxiety for practitioners, because we all know that our predictive capacity is low, but more importantly we know that unlike Internists and Surgeons we have limited access to the resources necessary to address the problem.
Considering for a moment a typical outpatient crisis, for a person known in the practice with depression who is now clinically changed in an office assessment with suicidal thoughts, the options are very limited. In the case of an assessment of extreme risk, inpatient treatment may be offered. If the patient has any inpatient experience at all, he or she knows that inpatient units are generally miserable places where very little active care happens and where they are enclosed with a number of very ill patients. They may also know that there are an arbitrary number of hoops that must be jumped through in order to be discharged and that as a result they may be in that environment much longer than they need to be. They may also have had a typical experience of the inpatient psychiatrist not talking with their outpatient psychiatrist and making a number of abrupt medication changes that are neither necessary or indicated based on their brief familiarity with the case. For those reasons and also because most people are averse to sitting in hospitals - people will balk at the suggestion of inpatient care.
The suggestion of inpatient care also assumes there is the availability of that option in the community. Most hospitals in any given state do not offer inpatient psychiatric care. That level of care has been discriminated against at a political and financial level for 30 years and as a result hospital services and inpatient psychiatric beds have contracted in an expected manner. Patients are often transferred hundreds of miles within states to reach these beds. A related issue is the availability of electroconvulsive therapy (ECT) for severe depressions. In the case of high risk depression it may be the only effective option. Many states have no availability of this option for patients who need it.
The suggestion of emergency department (ED) care is an even bigger dead end. The vast majority of ED care is provided by mental health professionals who are not psychiatrists and who are making triage decisions that ED physicians can sign off on. The wait is hours and if a high risk determination is made it might be days in the ED before any disposition can be made. Patients are often discharged on the basis of whether their suicidal ideation is chronic or not and whether they are saying that they have a suicidal thought and an intent to harm themselves right at the time of the assessment.
All of the above factors generally place the burden of care back on the original treating psychiatrist, even when the risk is higher that he or she would want. Most psychiatrists recognize that if they are treating very ill patients, there needs to be an element of acceptable risk in order to provide treatment and the hope of recovery. Psychiatrists realize that resources are severely rationed, that their patient needs acute treatment, that the patient will only accept certain treatment, and that there is a societal expectation of medical paternalism if the patient in not able to remain safe. The psychiatrist and the patient are frequently operating in this zone of acceptable risk that is perceived very differently by others. Family members are the clearest case in point. Like society in general, many family members have their biases when it comes to psychiatry. Many have been instrumental in discouraging their family member from getting treatment. In some cases they have interfered with treatment and suggested that the family member discontinue treatment or throw away any medications that they have been taking. At the same time, family members generally favor a zero risk treatment environment. They would prefer that the patient's suicidal thinking resolve completely so that there is no risk that they will attempt suicide. They see suicidal thoughts as controllable and the product of a series of correctable decisions. They don't understand why the thoughts just can't be turned off by the patient, their psychiatrist, or in some cases - the medication the patient is taking. In extreme cases, they may threaten litigation if the patient suicides or makes a suicide attempt implying a volitional and controllable basis for suicidal thinking.
An understanding of human consciousness provides a way to analyze this situation and the misperceptions about suicidal thinking and behavior. The predominant model of risk assessment for both suicidal ideation and aggressive potential is risk factor analysis. It generally proceeds from an elaboration of the specific thoughts to past history of attempts, availability of lethal means, diagnostic risk factors, past history and analysis of attempts, and specific demographic risk factors associated with suicide attempts. Many texts like the Harvard Medical School Guide To Suicide Assessment and Intervention have detailed approaches to the problem and further conceptualizations like proximate and distal risk factors. In an earlier post, I discovered a checklist of risk factors that looked at the issue of Increased Reasons or Decreased Barriers to suicide called the Convergent Functional Information for Suicide Scale (CFI-S). Many institutions these days prefer the Columbia Suicide Severity Rating Scale (C-SSRS). All of these methods are essentially based on risk factor analysis. Some are more elaborate than others. There all estimate risk to one degree or another and in some cases factors that mitigate risk. I won't debate the merits of these methods here. All that I want to say about them is that after the risk has been estimated, the psychiatrist may still be working with a high risk patient who is unpredictable in both an inpatient and an outpatient setting. Interventions can be initiated to reduce the risk, but there is no assurance that they will be effective fast enough to prevent a suicide attempt. In many clinics where a standardized approach like this is used with an electronic health record and a cutoff score is used to determine risk, a psychiatrist may find the patient visits being flagged for months or longer based on these numbers.
Is there another model that might supplement or improve upon the risk factor analysis models? For about 15 years now, I have been looking at a model that considers the basic question of what happens when a human conscious state shifts from one that would never contemplate suicide to one that does or in the extreme state proceeds rapidly to suicide. The usual psychiatric model considers the development of an illness state like depression, bipolar disorder, borderline personality disorder, or alcoholism as a precursor state. The cognitive changes, like depressogenic thinking seen in the precursor states are seen as the basis for suicidal thinking. The intervention is generally directed at reversing the precursor state, acutely structuring the environment as necessary for safety, and direct verbal interventions to address the suicidal thinking.
It is possible to explore with people the transition of their conscious state from a person without suicidal thinking to a person who develops suicidal thinking and consider a broad array of associated factors. Just being able to recognize that this transition has occurred is an important part of any evaluation and intervention. Some people are so severely depressed that it seems like the suicidal thinking has been there forever. They can barely recognize a time when they felt better or were not suicidal. In many cases they are preoccupied with existential factors such as meaningfulness of their life, personal freedom, and of course life and death - factors that they were only peripherally focused on during their daily life. In some cases they are important psychodynamic factors such as the death of a family member or friend from suicide. I speculate that many psychiatrists have heard of or been involved in situations like this. These events are also described in some of the psychoanalytic literature but not necessarily the risk factor analysis literature. John Bowlby described some examples in his book Loss:
"From many examples from Cain and Fast we select two: one eighteen year old girl who drowned herself alone at night in much the same fashion as had her mother many years earlier; the other a thirty-two-year old man who drove his car over the same cliff that his father had driven over twenty-one years earlier. Some of these individuals, it seems, had lived for many years with a deep belief, amounting to a conviction, that they will one day die by suicide. Some quietly resign themselves to their fate. Others seek help." (p. 389)
Of course the complexity of this situation is much greater than Bowlby can capture in his brief explanation. Just at the psychodynamic level there is the issue of identification with the parent and their suicidal actions. Do they believe that they have a deeper understanding of the parent's action and consider them to be logical? Have they incorporated this into their worldview and consider it to be their fate? At the neurobiological end of the spectrum, is it a case of straight genetic vulnerability to suicide or were there epigenetic factors related to a severe disruption of the home environment that the suicide of a parent can cause? Do they remember an event or series of events during childhood when the affected parent seemed to transmit a tendency to anxiety or depression directly to them? All of these are relevant considerations when examining what is going one at the conscious level in an individual who has become suicidal.
Elementary risk factor analysis also benefits from the broader perspective of considering other conscious factors. It allows for an exploration of additional degrees of freedom. For example, the issue of firearms possession and the elaboration of risk often depends on possession and risky behavior with that gun. But what constitutes risky behavior and what needs to be asked? Have you had the gun in your hand when you were thinking about suicide? Was the gun loaded? Did you actually point the loaded gun at yourself? What were you thinking about at that time? The questions and responses cannot be anticipated in a linear risk factor analysis or algorithm.
A nonlinear consciousness approach can also incorporate an informed consent approach to provide active feedback to the patient on the current risk and the limitations of treatment. This often opens a window into the dynamics of how the patient conceptualizes risk and their ability to work with the psychiatrist in minimizing it. A more linear assessment often takes on the structure of the psychiatrist trying to guess whether or not the patient is going to kill themselves and leaves the patient as a relatively passive participant. A consciousness based approach recognizes that the patient has entered at least partially into a conscious state that is foreign to them, less predictable, and represents some degree of risk to them. They need to hear very clearly that they and the psychiatrist need to work together to restore their baseline conscious state and reduce risk in the meantime. The process encourages them to not leave the interview leaving something that is potentially important - unsaid.
George Dawson, MD, DFAPA
References:
1: John Bowlby. Attachment and Loss - Volume III: Loss - Sadness and Depression. Basic Books. New York. Copyright by the Tavistock Institute of Human Relations. 1980, p 389.
2: Douglas G. Jacobs (ed). The Harvard Medical School Guide to Suicide Assessment and Intervention. Jossey-Bass Publishers; San Francisco. Copyright by the President and Fellows of Harvard College. 1999.
Tuesday, June 14, 2016
Worst Mass Shooting in US History
I got up Sunday morning and the CNN headlines stated: "50 dead, 53 injured.....". What appears to have been a single shooter entered an Orlando nightclub last night at about 2AM and shot 92 people with an assault rifle. I saw Dr. Michael Cheatham of Orlando Regional Medical Center say that a mass casualty incident was declared and an additional 6 trauma surgeons and a pediatric trauma surgeon were brought in. The FBI is investigating it as an act of terror or a hate crime. The shooter was a 29 year old man who had been investigated by the FBI for possible ties to Islamic extremism. He had been working as a security guard for a company who provides services to the federal government. He was licensed to purchase firearms. He purchased two firearms shortly before the shooting - a Sig Sauer MCX Carbine 0.223 cal on June 4 and a Glock 19 9mm pistol on June 9 from the same gun shop. Some reports suggest he was also carrying a Walther P22 .22LR pistol, purchase date unknown. Prior to this incident the worst mass shooting incident was the Virginia Tech incident in 2007 that killed 32 people.
At the time of the attack the shooter called 911 and pledged allegiance to ISIS and mentioned the Boston bombers. President Obama came on the networks at 2PM and referred to the incident: "This was an act of terror or hate." He pointed out that this was an attack on all Americans and he encouraged solidarity. In an earlier commentary (posted above) he discussed solutions. He used the example of highway traffic fatalities and how they were approached from a scientific and public health standpoint. Vehicle safety improved. Driver behaviors especially driving while intoxicated was confronted. Although he did not mention it, the drinking age in the United States was increased to age 21 largely by political leverage using federal highway money granted to individual states. He pointed out that these same public health measures cannot be used in the case of firearm violence because Congress has blocked research on firearm deaths and violence. He discussed a situation that he had just encountered, where people being tracked by the FBI for frequenting ISIL web sites could be put on the no-fly list but they could not be prohibited from purchasing firearms. That legislation is blocked by a gun lobby with a primary thesis that some members of the government want to take away Second Amendment rights and firearms from law-abiding citizens. The President points out that nothing could be further from the truth and cited the fact that more firearms have been sold during his administration that practically any other time of the Republic. I think the manufacturing statistics might back up that claim at least based on a chart I created during the first half of his administration. Further information corroborating this statement is available at the document Firearms Commerce in the United States 2015 on the ATF website. There is plenty of data there to corroborate both the President's remarks and the potential financial conflict of interest of the firearms lobby. I am sure that the gun advocates will be the first to say they deserve credit for gun commerce rather than the President. My speculation is that they would deflect the conflict of issue by either wrapping themselves in the Second Amendment or as advocates for all of the law-abiding gun owners.
I think that most physicians agree with a public health approach to gun violence and would like to see more data and strategies. The existing data shows that gun availability is the single largest determinant when it comes to firearm deaths either due to suicide or homicide. It accounts for the greatest correlation with adverse outcomes from gun violence. By comparison psychiatric diagnosis does not.
The President's comments on the further political aspects of gun control legislation in the US especially people being investigated by the FBI, like the perpetrator was on two occasions cannot be prohibited from obtaining firearms. That speaks directly to the pro-gun argument that all we have to do is focus on existing laws and get the guns out of the hands of the bad guys. This law potentially puts guns directly into the hands of the bad guys and nothing is being done about it. The Obama video was posted 10 days prior to the Orlando attack.
I won't belabor the points I have already made in a series of posts on this blog. We are still seeing the same microanalysis and political opportunism that has become a routine part of mass shootings. We are still seeing the lack of solutions like we have seen in the past. The way it looks I can continue to post on the issue on out into the future it will probably be a problem long after I am gone. I heard a gun advocate on public radio this morning and what he said after this incident was not only depressing and disingenuous, but it typifies a rigid illogical stance that no place in science, medicine, or the 21st century. It illustrates why the gun lobby has Congress enact laws to stifle funding for epidemiological work on gun mortality and morbidity. I suppose at this point it is just a question of when we hit the tipping point. When will the majority of Americans start to reject this illogical philosophy?
If the gun advocates hit the street with this hard line attitude after the scope of a mass shooting like we witnessed in Orlando - I shudder to think of what the eventual human cost is going to be.
George Dawson, MD, DFAPA
Attribution:
Embedded video per PBS and the instruction on their site. Original video was from June 2, 2016
Sunday, June 12, 2016
Ophthalmology Styled Practice As A Goal For Psychiatry (And The Rest Of Medicine)
Over the years whenever I have thought of an ideal way to practice medicine ophthalmology comes to mind. I remember a good friend of mine telling me shortly before he became an ophthalmologist that the speciality seemed to have the ideal mix of medical and surgical interventions and they were mostly effective. He also had the great observation that no matter what field of medicine you specialize in - the information in that field will generally be contained in two or three large volume texts. The information always expands to that amount with specialization. My friend was a very bright guy.
Like most specialties, I have had my fair share of personal contact with them starting with a BB gun injury in the 8th grade. That's right - just like in the movie - I almost shot my eye out. And just like in the movie, my father told me shortly before the accident: "Be careful with that BB gun - you will shoot your eye out!" Within minutes, I was standing there in disbelief. A BB had ricocheted off a steel lamp cover in our basement and instantaneously hit me in the left eye. Within minutes I looked in the mirror and was more shocked to discover that my iris color had been replaced with blood inside the anterior chamber of the eye. The family doctor was called and advised my parents not to bring me to their office or the emergency room, but to see the new ophthalmologist in town. He was the only physician in town who could assess and treat this injury. I spent a week in the hospital with both eyes covered and eventually recovered with a traumatic cataract in the lens of my left eye. Every ophthalmologist since has said the same thing: "You are lucky that cataract is just off your visual axis and it does not affect your vision." Even more interesting, the last ophthalmologist I saw wanted to know about my experience of seeing with a traumatic cataract just off my visual axis. In what ways did it seem different than the other eye. After many questions he finally said: "I am just trying to find out what it is like for you to have this cataract." An ophthalmologist interested in my conscious state of vision?
These are some useful lessons from ophthalmology:
1. Precise assessments based on clear markers:
There is still room for interpretation. No two retinas are alike. As another example, an eye doctor told me recently that prominent retinal arteries may put you at risk for glaucoma. I saw a second eye doctor 2 weeks later who agreed that I may be in the subgroup of people with prominent retinal arteries but that does not put me at higher risk for glaucoma. In 50 years of annual eye exams my intraocular pressures have always been normal. I have also used the eye exam in lectures on diagnostic accuracy looking at the issue of the diagnostic accuracy of direct ophthalmoscopy versus indirect ophthalmoscopy, basically ophthalmologists versus everyone else. The ophthalmologists win by a wide margin when it comes to detecting retinal pathology. The odds that a primary care physician can detect these changes with direct ophthalmoscopy as a screening exam are no greater than chance. In the days when I did a lot of direct physical examinations of patients, I was convinced that most physicians either did a poor job of using an ophthalmoscope or were just focusing on major landmarks. They also seemed to ignore the general clinical status of the patient. I recall an agitated, hypertensive, young stroke patient and clear hemorrhages in the retina. I diagnosed the retinal hemorrhages and nobody else did, but they could confirm when I told them where to look. Like all of medicine the subjective factor is there, even in what appear to be objective assessments, but ophthalmology seems to have some of the greatest potential accuracy and reproducibility.
2. Interventions that are fast, safe and effective:
About 8 years ago I was interviewing a patient and looked down at the wood grain of the table. It started to swirl and move in one visual field. I was part of a big multidisciplinary clinic at the time. The information flow among the specialists was the best I have ever seen it. I called the ophthalmology clinic spoke with an ophthalmologist. After about 30 seconds of symptoms he said: "You have a retinal migraine. We can get you in this afternoon, but I doubt there is much else." I went with that advice and have had no similar problems since. A few years ago a family member called me on a Saturday morning and said he had sudden onset of veiled vision and floaters. He lives in a town of about 50,000 people. He was able to see a retinal specialist and get laser surgery on his torn retina in a matter of hours. I have had three other relatives with retinal surgery - all very successful. In my case about one month ago, I had a sudden onset of eye aching, massive floaters, and large bright halos surrounding the entire visual field of my left eye. I was triaged to ophthalmology in a few hours and diagnosed with an acute vitreous detachment with a plan to observe for any retinal damage in two weeks.
3. Interventions that clearly enhance quality of life:
Saving someone's vision needs to be at the top of anyone's list when it comes to quality of life. Surgical specialties are generally a very active intervention by physician with very good outcomes and some complications. From what I have seen the complication rates of eye procedures are very low and in some cases the advertised procedures being done are in excess of 10,000 - 100,000. In many cases there is an expectation that you will be seeing the doctor 2 or 3 times and that the chances of a good outcome that will improve your life are very high.
4. A clear path to getting well:
The majority of patients seeing ophthalmologists, don't have to do much to get well. Recognize the problem, discuss the treatment plan and risks/benefits of the surgical procedure and make the follow up appointments. In the case of medical treatment - use the required eye drops, visual aids, diet, and protective equipment and participate in the monitoring plan. In the patients I see with eye problems I know that many of them do not follow up. I routinely ask about a personal history of eye trauma, visual problems, glaucoma, and macular degeneration. In some cases I call their ophthalmologist directly about whether the medication I am about to prescribe would affect their treatment. But generally an optimal path to care with a good outcome is outlined form most ophthalmology patients and the burden of adherence is relatively low.
Contrast that with a patient walking into a psychiatric clinic. By that I mean a patient who gets a direct appointment with a psychiatrist. There is no precision in the assessment. There is a diagnostic manual that gives the appearance of precision, but it is fairly worthless unless the physician knows how to get at it and that generally involves having seen many patients with the problem. It also involves concluding that many DSM-5 categories are so nonspecific or unrealistic that it makes no sense to make the diagnosis. With a diagnostic manual that imprecise, markers are sorely needed and I am optimistic that we are on the verge of some. I am optimistic that with the correct markers we will be able to define categories and clearly define treatment paradigms on those categories, but I don't expect that to resemble a DSM or an RDoC for that matter. The burden of adherence is much higher. Polypharmacy and keeping all of those medications straight is certainly as big a problem in primary care and the medical specialties. Nobody else wants to see people back on an hourly basis for weeks, months, and years.
One of the fastest and safest interventions in psychiatry is electroconvulsive therapy. In many parts of the country it is unavailable. The FDA has some continuous program afoot to "reclassify" it. This is the second iteration of that program since I responded to the first one years ago. The only logical conclusion is that this is some kind of political maneuver being played out in a regulatory context. My understanding is that reclassification would mean new sets of clinical trials to get FDA approval for devices. It should not be surprising that very few places offer it, and thousands of patients go through endless clinical trials of antidepressants with no remission of their symptoms. TMS (transcranial magnetic stimulation) and VNS (vagal nerve stimulation) seem far less impressive in treatment resistant populations. Just last week a colleague also pointed out that there are probably thousands of patients who might benefit from ketamine infusions and that seems to be another procedure in limbo pending FDA considerations. Without FDA approval, health insurers will deem a treatment experiment and not pay for it. That is when treatment usually grinds to a halt.
Quality of life considerations should be high on any psychiatrists agenda since we learned that we treat conditions that are listed in the Top 10 of the World Health Organizations list of disabling conditions. Unless we get robust treatment responses, quality of life is not likely to improve. There are vast numbers of patients who are disabled and maintained on medications. They clearly need more than the medication but the only service offered by their health plan is a series of brief visits with a psychiatrist or a prescriber, generally focused on polypharmacy. There is no attempt at cognitive or vocational rehabilitation. Those services are available to stroke patients but not psychiatric patients.
The path to getting well and recovering from a mental illness or addiction is often not clear. The message has been oversimplified to "Take your medications as prescribed." The same patient may hear "Don't do drugs or alcohol." but typically only after a problem has been identified for a while. The average person with an addiction (according to survey literature) does not disclose that to a physician. Most people after an acute episode of a mood disorder or psychosis - don't know where to start. They don't know what happened to them and they don't know how to prevent it from happening again. They may hear that they need "therapy" or "counseling" and realize that after 5 or 6 sessions, they don't like the therapist or the sessions aren't going anywhere. What is left at that point? Go back and see the prescriber in 15 minute lots about medications that seem to hardly have an effect or a seemingly endless series of medication trials?
Instead of parsing words in somewhat meaningful categories we need to pick up the pace. In my experience the people who are willing to see psychiatrists for a long period of time for pharmacotherapy, psychotherapy or both are in the minority. It is clear that many psychiatrists end up seeing patients three or four times a year in what appears to be interminable treatment. All the while the patients have varying degrees of disability and problematic quality of life.
All of this care is delivered by 19,216 ophthalmologists who are addressing an impressive array of eye diseases and injuries. As previously noted there are 49,070 psychiatrists also addressing a lot of illness and disease. Just like my previous argument about orthopedic surgeons, I have never heard of any shortage of ophthalmologists.
Ophthalmology teaches us that there is a much better way and we should be designing those paths of care instead of the giving it over to the business people and politicians. A critical question on the idea of a shortage of psychiatrists is how much of that is due to the inefficiencies suggested above including interference from politicians and business organizations.
George Dawson, MD, DFAPA
Saturday, June 11, 2016
Lessons From Orthopedic Surgeons
I sprained my ankle last Friday. It was a curious experience because it is probably the first time I sprained an ankle in about 40 years. I just rolled it over coming off the bottom step of a stairway and then did the same thing at home the same day. Some pain but not bad. I was immediately able to walk on it and bear full weight on it. Over the next week it was a waxing and waning course. Still able to walk. Most of the stiffness and pain in the morning. About every other day I took a tablet of the naproxen in the morning and that seemed to alleviate the pain by evening. I went to work, at a job where I typically put in at least 10,000 steps per day on a fairly large campus. A week later it was unchanged, still painful at times and swollen. I thought I needed an x-ray to rule out a fracture. The question is - where to go? Emergency departments in my experience are the absolute slowest. I could also imagine the eye rolling when I tell them the injury is a week old. I could go to the local urgent care center, but they seem surprisingly ill equipped for most problems. I was there a few years ago for bronchitis and they shot a chest x-ray that was overpenetrated and useless for seeing infiltrates. I would not have lot of confidence in their ability to shoot an ankle film with adequate technique to take an optimal look for fracture sites. I could go to my primary care clinic, but that takes phone time and half a day of PTO. All I need to know - is there a fracture, do I need to see an orthopedic surgeon, and what do I do to take care of it. The last time I had an orthopedic problem and needed to get a splint, my primary care clinic referred me to a pharmacy that had a lot of medical equipment. They did not have much in onsite to help me.
Then I remembered seeing an ad for an orthopedic surgery specialty group. They had a number of new city-wide clinics. One of their features was an acute injury walk in clinic. No appointment was necessary. I had nothing to lose.
The clinic lobby looked like one that you might see in a luxury hotel. There were a bank of receptionists there to get the process going. After about 10 minutes of paperwork, I was taken to an exam room by an RN who examined the ankle and took additional history. A minute later, I was off to x-ray for three views of the ankle. A minute after I got back to the room, I was examined by a physician's assistant who immediately let me know that there was no sign of a fracture. She took additional history, and did a more extensive examination of the foot and ankle. he showed me very good resolution views of the ankle on her flat screen computer monitor. She Ace wrapped the ankle gave me some care advice, two extra Ace wraps and sent me on my way. The total time of the visit was 30 minutes - 20 minutes if you don't count the time I was filling out the forms. It was all very focused and very efficient.
According to the American Academy of Orthopaedic Surgeons, in 2014 here were 28,047 orthopedic surgeons in the United States. The American Association of Medical Colleges estimates 49,079 psychiatrists for comparable time period (2013) in the US. Various sources including the American Psychiatric Association release stories about the shortage of psychiatrists. I have not ever heard of a shortage of orthopedic surgeons. But what does that mean? Shortages are often measured by the ease of getting an appointment. In some cases managed care organizations are quick to point this out possibly because many psychiatrists have fled both their work environments and compensation schemes. The collaborative care models (there are several) are a work around in that patients can continue to go to their primary care clinics where there is a psychiatrist working behind the scenes - assuring that their medication therapy is rational and that their rating scale scores are trending in the right direction. As far as I can tell, the vast majority of patients in collaborative care will never see a psychiatrist. Problem solved right?
Nobody seems to be applying the model I just experienced in this very focused and efficient orthopedic clinic. The principles that I directly observed are:
1. Not everybody needs to see a psychiatrist - The criteria for seeing a psychiatrist are very subjective based almost entirely on what the patient or the psychiatrist wants. Many private practice psychiatrists want a set period of time to do an initial evaluation and follow ups. Employed psychiatrists have to use whatever time they are allotted by the masterminds who are managing their productivity. What is the lesson from the orthopods? Triage the patient and see only the patients with the most complex problems. As long as I did not have a complex ankle fracture, I could see a PA-C and get perfectly fine care.
2. The resulting structure of the clinic benefits from that hierarchy of complexity - There were numerous exam rooms with teams of PA-Cs, nurses, and x-ray techs, screening high numbers of walk ins and treating them rapidly and efficiently. The orthopods were on site doing ambulatory surgery and following up with complex post-op and non-operative patients. There were also a number of physicians on site who were not surgeons but who focused on the medical treatment of sports injuries and spinal problems. This has immediate applicability for psychiatry. The procedures in psychiatry that create bottlenecks are electroconvulsive therapy and more recently ketamine infusions and transcranial magnetic stimulation (TMS). Shifting psychiatrists away from more routine problems would immediately create greater capacity within systems to offer that higher level of care and it could be delivered in an ambulatory setting. It could potentially provide needed treatment to thousands of people with treatment resistant problems who do not have easy access to a more intensive level of care.
3. The culture of the orthopedic clinic was the care of the orthopedic patient, greatly enhancing the efficiency and focus of that process. Orthopods don't provide collaborative care in primary care clinics and there is no broad initiative to get them there. Specialization has its benefits and in my experience all of the clinic personnel being focused on orthopedic problems was a plus.
4. The orthopedic clinic had certain expectations of social behavior - it was not explicit but you needed insurance or an ability to pay. Everyone was well behaved and nobody there was agitated or angry. That may sound elitist, but for many mental health and addiction clinics there seems like an expectation that any behavior is tolerated and if the staff has to expend considerable time and effort to deal with the complex problem of aggression or agitated and otherwise inappropriate social behavior - they should also be prepared to provide those hours of care for free.
5. The orthopedic clinic was providing care that has traditionally been done in hospitals and they were quick to point out the differences - complex care being delivered in a setting in comfortable non-hospital surroundings with staffing ratio high enough to provide the level of care that people expect. Managed care hospitals and clinics often try to manage expectations by interviewing protocols prior to giving that patient a satisfaction survey. The approach used in this clinic is to redesign the clinic and service delivery first and then see what happens on the surveys.
6. The orthopedic clinic has state-of-the-art equipment - No x-ray machines from the 1980s. I saw high resolution images a few minutes after they were taken on a computer monitor in an exam room. The contrast was excellent.
I know that a lot of physicians reading this are thinking that I have lost it. Orthopedic surgery is a much more well compensated and well defined field than psychiatry. How would a group of psychiatrists attempting this model be able to pull it off financially? The biggest risk of course is managed care companies shifting most if not all financial risk to the clinic and poor reimbursement from public payers. In my opinion, a lot of that is because of the usual biases against psychiatric care, but it is also due to the lack of negotiating savvy on the part of psychiatric clinics. There is also a well known bias by managed care companies to get rid of psychiatric services or ration them either out of existence or to the point that any psychiatrist working for them is assured of providing a lot of work for free. A good place to start would be to study models like this one or radiology or anesthesiology groups and figure out what percentage of their customary fees do they negotiate for in contracting arrangements. Without that knowledge - you can't keep your doors open unless you adopt a straight fee-for-service arrangement with cash paying customers. It has been demonstrated time and time again that managed care companies shut down psychiatric clinics and reimburse so poorly that most practitioners cannot accept their patients.
There are a number of arguments out there - many by other psychiatrists on whether a clinic like the one I suggest should exist. The standard argument is that it will skim off the "worried well" and not treat serious psychiatric problems. My experience in numerous clinics and hospital settings would suggest otherwise. There are many people with acute crisis situations or stress responses who end up in the emergency department where they get admitted on emergency involuntary holds. They may go to a primary care clinic where they are referred to the ED if they are perceived as having suicidal ideation or just put on antidepressants. The majority of these patients do not have a serious psychiatric disorder and need a crisis care center where they can get active treatment. In this case the "worried well" have been mishandled for decades. Another resource that is needed is a safe place to treat hypomanic or manic patients who can't function at work or at home. None of these folks likes to be housed in a hospital active day treatment with some temporary housing may be possible in a large well resourced psychiatric clinic.
Psychiatry has been thoroughly fragmented by by managed care systems and governments. A large clinic like the orthopedic clinic I described, but focused on psychiatric services could potentially pull together many of the resources needed for comprehensive care and greatly improve quality. Anything moving psychiatric practice away from brief sessions focused on managing polypharmacy toward providing comprehensive services again would do the same.
George Dawson, MD, DFAPA
Attributions:
1. Left ankle is my actual ankle x-ray.
Sunday, June 5, 2016
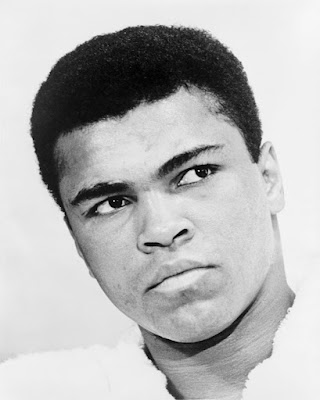
Muhammad Ali - The Social Context Of A 15 -year old
I occasionally post in a local political forum in Minnesota. I generally try to avoid it because politics in science is interesting at severals levels but the politics of American political parties is not nearly as interesting. The biases and political responses are always predictable. It is always a mystery to me why there are so few reasonable candidates. A few friends who have run for office and not made it on party ballots have given me their opinions, but this post is not about that. The other aspect of politics as I have stated hundreds of times on this blog is how it gets transacted in academia and professionally. The biases are again evident. In science nobody seems to take complexity into account on reproducibility issues or the unconscious biases of the researchers. In looking at conflicts of interest, nobody seems to take into account that in many cases (like the price of pharmaceuticals) that there are clearly some conflicts of interest that trump most of the others. But again, this post is about one aspect of politics and that is connectedness to the candidate.
Today - I was reading my e-mails from the political forum and I came across a statement about how Barack Obama did not connect well to the middle class. I think that the research shows no matter where you end up in life, your class identification stays where you were when you grew up. That would place me solidly in the middle class - in the lower half if socioeconomic status means anything. I have seen a lot of Barack Obama and can appreciate his charisma, intelligence, ability to communicate and personality. As a small "i" independent I don't always agree with his politics, but there is no doubt that this is a guy who I can relate to and I have very high regard for. I want nothing but the best for him. In thinking about why that might be, I reflected on another prominent American in the news this weekend - Muhammad Ali.
Listening to a lot of news this weekend about his passing - I like George Foreman's comments the best. This is an excerpt of a CNN video of George Foreman on meeting Muhammad Ali in New York City sometime after their fight in Zaire:
"....Everybody falls in love with him. You can't help it. He was one good looking, lovable guy. I was excited to meet him and happy to be his friend." - CNN - June 5, 2016.
I never came close to meeting Muhammad Ali. I have never attended a boxing match and even if I did, by the time I could afford it he would have been retired. My initial experience was as an early teenager in a remote outpost in northern Wisconsin. The communication in those days was primitive - just newspapers, magazines, radio and television broadcasted out from Duluth over the airwaves to your antenna. There were three television channels and on a good day - you could see two out of three. My grandfather would often say: "They've got kids running those TV stations." to describe the predicament. It was a long time before they could send a clear signal. Even in those primitive pre-Internet days, Muhammad Ali could dominate a long news cycle with his comments and the press and others reacting to those comments. There were a long series of controversies. As a young guy he was probably the most exciting sports figure to watch. He was verbose at times, articulate, and he had a great sense of humor. When he was saying something that many considered to be outrageous, he was smiling and I had the sense that he knew exactly what he was doing. He would also not back down from an argument even when he was being videotaped. No matter what he was saying, I found myself nodding in agreement with him. The other sports heroes I had at the time were shallow by comparison. No other sports figure could comment at length on American culture, religion, and philosophy. There were no other sports figures who had such an active relationship with their fans.
But the most striking thing I remember, is that older generations of men did not react the same way. Most of what Ali did made them very angry. And of course at times they characterized him in very ugly racist language. Racism was rampant at the time, and it was everywhere. In rural areas, it wasn't obvious because there were no black people. My father was a railroad engineer and as a special day, he would take me to the roundhouse with him. The roundhouse was the industrial side of the railroad. All of the engines were housed in a roundhouse, just off a large turntable that allowed them to be rotated 180 degrees and connected with the main line. There was a very plain locker room with various signs encouraging adequate hygiene. In the room at the far end was an area designated for porters. I asked my father who the porters were, but I never got an answer and I never saw a porter. Passenger traffic had just about ended by then and the only thing the trains were hauling was iron ore, coal, and large bundles of scrap paper for recycling.
As a 15 year old, I had to bite my tongue while the old guys in the room cheered for anyone to beat Ali or while they criticized his boxing skills or just made outrageous comments. But it was the 1960s and the culture was rapidly changing. Young people were getting louder and norms that had been in place for a generation were no longer accepted. It was easier at first to publicly agree with Ali's stand as a conscientious objector, but it soon became obvious that you were a fan of the athlete and then the man. I heard some commentators talk about the tumultuous times when Ali first grabbed the national spotlight, suggesting that had something to do with his fame. I would see it as being the other way around. A lot of young guys like me identified with him. At some level it was teenage hero worship, but unlike the other sports figures - he did not go away. He was an example of a sports legend who became a great man and on this weekend those stories abound. I found a kindred spirit where I work and we have been exchanging Ali stories, pictures, and clips for the past few years. Most of these stories are after his retirement from boxing and it is an impressive body of work.
Those were my associations to the notion that Barack Obama does not connect well with the middle class. It is easy to identify with charismatic, intelligent, articulate, and empathic people. I am sure that I am not the only 15 year old that had his eyes opened to that.
And I won't be the last.
George Dawson, MD, DFAPA
Attribution:
1967 portrait of Muhammad Ali by Ira Rosenberg [Public domain], via Wikimedia Commons at: https://commons.wikimedia.org/wiki/File%3AMuhammad_Ali_NYWTS.jpg
In 1967, I was 15 years old.
Friday, June 3, 2016
Are Hallucinogens The New Miracle Drugs?
 |
| See Attribution 1 for full reference |
Steve Jobs: "Taking LSD was a profound experience, one of the most important things in my life. LSD shows you that there's another side to the coin, and you can't remember it when it wears off, but you know it. It reinforced my sense of what was important - creating things instead of making money, putting things back into the stream of history and of human consciousness as much as I could." (ref 1)
Woodstock (Chip Monck): "To get back to the warning that I received. You may take it with however many grains of salt that you wish. That the brown acid that is circulating around us isn't too good. It is suggested that you stay away from that. Of course it's your own trip. So be my guest, but please be advised that there is a warning on that one, OK?" (ref 2)
Warning: The final few paragraphs of this post contain language that some may find offensive. I included it for a reason. In 30 years of practice and in my real life - I have found that many people talk this way. If profanity offends you don't read the end of this post.
Everywhere I turn these days - whether it is a blog or more traditional media I am struck by the same stories on hallucinogens. If you believe what you read out there, hallucinogens are magical drugs in that they are almost totally benign, consciousness expanding, and they can treat your anxiety or your depression. They have been actively discriminated against like other illegal drugs and that is the only reason we have not done the research to prove that they can treat many problems. Back in the 1970's we would have said that "The Man" is restricting access to valuable consciousness expanding drugs and if "The Man" was overthrown - the world would be a much better place. I have briefly reviewed the same lines of rhetoric that occur with cannabis. I have not heard similar arguments with ketamine, probably because fewer people have experience with it and it is a more difficult drug to use, even in a medical setting where the drug has a known concentration and purity.
Hallucinogens are a diverse set of compounds with a number of analogues of the parent compounds for each basic structure. The DSM-5 does very little in terms of organizing the category other than saying that it might make sense to classify the dissociative hallucinogens like PCP and ketamine as a separate category from more traditional hallucinogens like LSD. The DSM-5 does very little to attempt to classify the wide array of hallucinogens that are available at this point in time. Some authors (3-6) use the term serotonergic or classic psychedelics such as LSD, DMT, and psilocybin (and see above graph). I think it makes sense to classify any drug taken for the express purpose of creating hallucinations - a hallucinogen. Drugs with secondary hallucinatory effects like alcohol, cannabis, and stimulants remain in unique categories because they can all cause hallucinations but they are generally not taken for that purpose, More scientific classification approaches that are generally based on chemical structure are available in standard addiction texts.
As an addiction psychiatrist, my experience is that hallucinogens are problematic drugs from a number of perspectives. It is rare to see a pure hallucinogen user, at least until someone discovered that using high dose dextromethorphan (DXM) reliably produces hallucinations and delirium, is widely available, and inexpensive. To that subgroup of patients many of them have a very difficult time stopping DXM. The other problem with that drug is that excessive use of DXM in the predisposed person is common and the margin between the hallucinatory experience, toxicity and lethal overdose is not well characterized probably due to pharmacokinetic variability among subjects. Reports of lethal ingestions in the medical literature are rare (5). The hallucinogenic effect of DXM is from NMDA and PCP1 receptor antagonism. DXM is metabolized by hepatic CYP2D6 so that other drugs that are inhibitors and poor metabolizer status may lead to unexpectedly higher levels of the compound in the plasma. DXM is also a serotonin reuptake inhibitor and a 5-HT1 direct agonist and can cause serotonin syndrome another potential cause of death when used with other serotonergic drugs. PCP is another exception. In my experience both PCP and DXM users are much more likely to use those drugs in an uncontrolled manner and addictive manner than other types of hallucinogens. There are seemingly rare but significant and in some cases fatal side effects from hallucinogens. From a mental health standpoint, addiction specialists and general psychiatrists encounter patients with significant ongoing panic symptoms and perceptual disturbances that they attribute to the side effects of these medications. The question is what is the frequency of these side effects and their significance? An associated question is have there been any definitive studies?
Most of the recent epidemiology of hallucinogens has come from Krebs and Johansen. Their 2013 study in PLOS was widely quotes in the news media as illustrating that classic hallucinogens are benign substances with little health risk. Their work is based on the annual NSDUH survey of drug use in Americans. They look at two small (N=192, N=156) cohorts of pure hallucinogen users in the NSDUH survey. They outline the limited nature of this investigation based on the survey questions and the fact that this is a survey. They cite other literature looking at people given LSD in clinical trials and other research and conclude that there is very little evidence for lasting side effects. As an example, they could not corroborate that at least some people who taken hallucinogens have persistent problems with anxiety, panic attacks, or perceptual disturbances. These are familiar themes in the new research on LSD noted in several of the additional references. As a starter, I read the articles (7-10) and came up with several unanswered questions. Some are obvious in a technical sense and some are not so obvious. Rather than get into a detailed critique of this and other papers, I thought I would outline what I see as missing in the claims made for the benign side effects profiles and efficacy of these drugs and look at more details in subsequent posts.
Efficacy for what?
These drugs in the broadest sense are not used to treat any specific collection of symptoms or syndromes. Their popular indication for use has changed very little since the 1960s (3) and that is "mystical experiences, curiosity, and introspection." At that level there is no medical indication for use. They are being used to produce an altered state of consciousness like alcohol or any other recreational drug. At that level the issue resembles in many ways medical cannabis, with the exception that cannabis seems to have some very preliminary evidence that it might be useful for some medical problems. No such data exists for hallucinogens and psychedelics, but that is not for a lack of effort. A recent meta-analysis discussed in Nature suggests that alcoholics treated with LSD are more likely to stay abstinent than those who are not. The original experiments done in the 1970s, found no such correlation. A recent paper in Lancet Psychiatry discusses application for the existential anxiety of the terminally ill and to facilitate psychotherapy. So far the medical indications seem to be a bit of a stretch. Using cannabis as the prototype, it seems that many parallel arguments are being made for hallucinogens. From a rhetorical standpoint it is interesting that a common antipsychiatry criticism is that psychiatry has medicalized life in order to proliferate diagnoses and make more money for pharmaceutical companies. Nobody seems to have any problems with cannabis or hallucinogen proponents medicalizing life in order to provide a useful venue for cannabis or hallucinogens.
As an adjunct for psychotherapy?
There is a new recent review (14) of psilocybin and MDMA as assistive modalities in psychotherapy. My read of this review is that the authors are proponents of these therapies. They cite the lack of useful current therapies as a reason for exploring the therapeutic aspects of psychedelics. That may be true to some extent but the usefulness of current therapies also depends on how broad the access is. When I do a new assessment, I don't get the same global acceptance of therapy that some in the popular press suggest. The impression I get is that the psychotherapy experience that most people get is suboptimal at best - and not because of the therapeutic modality. It is often the technique of the therapist, economic considerations, managed care constraints, and/or the lack of any results. The authors suggest that exploring psychedelics in these settings might offer better results and faster results. I can't help but think about how therapy in real life, doesn't resemble what the psychotherapy in clinical trials is like. Many people in managed care settings get two or three cursory sessions and they are discharged as doing better. What happens if psychedelic assisted psychotherapy occurs in a managed care setting? My guess is that the complex therapy is eliminated and the sessions where the drug is administered is emphasized. The conditions for therapy reviewed include cancer anxiety, addiction (alcohol, tobacco and cocaine) and obsessive-compulsive disorder for psilocybin and PTSD, anxiety from life-threatening situations, and social anxiety in autistic adults for for MDMA. There is minimal detail on the psychotherapeutic technique apart from some lengthy sessions. Problems with blinding in controlled trials are discussed as an issue. Lower dose psychedelics as the active placebo don't work. Preliminary successes and speculation about the effect of the psychedelics and what they might be doing are discussed. The main argument seems to be that there is ample reason to continue research in psychedelics.
What can be measured?
All clinical trials in psychiatry lack objective measurements of both illness and improvement. In the case of psychedelics some of these standard problems are still there. Standard rating scales for anxiety and depression are used in some of these trials. There are additional instruments such as the Altered States of Consciousness Questionnaire (ASQ) and the Psychotomimetic States Inventory (PSI). It seems that an interest in purportedly consciousness expanding drugs may finally get some psychiatrists interested in consciousness as a dynamic multidimensional entity independent of syndrome definitions. The problem of course is that these states are all highly subjective and resistant to classification. It also highlights the question: "Is the psychedelic drug +/- psychotherapy supposed to target a typical syndrome of anxiety or depression or is there some other purpose, like altering the conscious state in some fundamental way?". If that is true, we really have no idea how that can be measured or translated into therapy. I would also suggest that it is outside the purview of physicians and psychiatrists. If it is effective, the one aspect of psychedelic assisted therapy that I thought would be very useful was that the patient only takes two or three doses of the drug over the course of psychotherapy and does not require a maintenance treatment.
Quality of subjective measurement aside, there is nothing more annoying to me as an interested reader than reading about a rating scale or questionnaire that is not readily available. I need to know what the specific questions are on those instruments. The statistics of the instrument is a secondary consideration. As far as I can tell neither the ASQ or the PSI is readily available in a readable form. I would go so far to encourage editors to suggest that in the original analysis of rating scales, questionnaires, and inventories include the scale as it was used with all of the direct wording and how it was rated. If that data is not included the article is essentially worthless to any clinician who talks to patients.
Are we measuring dimensions of consciousness?
I have addressed the general lack of concern over human consciousness in psychiatry and medicine in general. Human consciousness is generally regarded as a brain determined state, but we have no idea how that state arises from the underlying neurobiology. There are plenty of theories and there is a scientific society dedicated to the study of human consciousness. Consciousness is a highly subjective state and that makes it very difficult to study. Even a basic consideration of experiencing the color red can be as complex as considering that each human being (every human being has a unique conscious state) can experience the color red in a unique way. We all may be able to agree on a basic task that requires selecting the color red from other colors, but beyond that we can never be completely sure of how other people experience colors or other physical properties or more complicated states like pain, depression, aging, or the opposite gender. If all that is true about human consciousness - what would we expect to happen if we are taking a drug that alters our conscious state. For research purposes, if we alter a conscious state and we really don't have a good way to measure a baseline conscious state - how can we detect what changes. Are we going to depend strictly on self report of whatever comes to the person's mind?
Sweeping conclusions about the lack of toxicity?
Any pro-hallucinogen article will produce a steady stream of references looking at how benign these compounds are. There are usually quotes about millions of doses consumed and no deaths from LSD or other psychedelics. The authors generally assume that the methodologies being quoted are adequate indications of drug safety. These arguments fail at two levels. First, there is evidence in the literature from reasonable sources that LSD exposure is not entirely benign. The 1986 Danish LSD Damages Laws is a case in point. In this study, 400 patients treated with LSD between 1960 and 1973 were followed. 154 of these patients were compensated for long term harm with 2/3 of them having severe flashbacks. There was also one homicide, 2 suicides, and 4 suicide attempts in the group (12). There is the question of other sources such such as the DAWN system that looks at the number of emergency department visits (ED) per day due to substance use. This system looks at annual use of substances by 18-25 years olds, how much they use on an average day and the number of ED visits per day due to a specific category of drugs.
 |
| See Attribution 2 for full reference. |
In terms of drug safety and pharmacovigilance, there really has not been any with these drugs. The side effects tend to be case reports, anecdotal, from settings where there is likely a bias to under report side effects, and from carefully run clinical trials. In some cases researchers have a defined protocol for the safe design and running of clinical trials involving psychedelic drugs (15).
Medicine or recreational drug?
Cannabis legalization was basically dead in the water until the proponents adopted a political strategy that involved selling it as a medical treatment rather than a recreational drug. The preferred path seems to be starting with terminal illnesses or illnesses for which there are no current good treatments. Nobody ever seems to explore the question about why the legalization question doesn't seem to carry the argument on its own merit. The arguments for the therapeutic use of hallucinogens seems to be following that same pathway.
More rights and politics?
Some of the pro-hallucinogen literature promotes the use of hallucinogens including the legal right of people to use hallucinogens. I have no problem at all with activists trying to influence their favorite politicians in a way that they can more easily obtain their favorite intoxicant. I do have a problem when activists start to write medical literature from that perspective. I also think that an additional level of disclosure is needed at the editorial level. Authors that argue for the availability of hallucinogens (or for that matter any recreational intoxicant) should disclose that as a potential conflict of interest by specific compounds. An example would be: "Dr. Smith supports the widespread availability of LSD for both medical and recreational use". Explicitly stating that potential conflict of interest, is every bit as important as stating that your research has been supported by a pharmaceutical company, but it is more difficult to track.
Is there a better way to live?
There are always philosophical and ethical considerations. As I hope to show in a future post, philosophers generally are not too interested in telling people how to live (although there are a few notable exceptions). Psychiatrists certainly are not interested in that either no matter how much rhetoric is out there saying otherwise. The arguments to use or try hallucinogens are of the general form that it may improve you in some way or offer you valuable insights. It certainly may not or in the case of many leave them with a very negative residual memory of the personal experiment or some residual symptoms. Much of the rhetoric is the old legalization argument: "If it really is that harmless, who shouldn't I have the freedom to use it?" Add the corollary: "It is less dangerous than tobacco and alcohol!" and you have a full scale legalization argument on your hands. This debate has become stereotypical these days and nobody seems to ever ask the question: "Is this a reasonable way to live?" or "Should people get high just because we can?" Do you really have to take a drug to expand your consciousness or can you do something else? Focusing on only the legal aspect and the freedom to use drugs short circuits that larger question and it is a very significant question. Moreover - if your goal is expanding your consciousness how do you know that LSD is the best way to do that? How do you know it is just not a complete waste of time - time that you may not have to waste?
There is a phrase that is popular in the drug using vernacular and that phrase is "fucked up." It encompasses an entire spectrum from a highly desired state of intoxication to a very dysphoric state of toxic effects, withdrawal effects, and delirium. Interview people at either end of the spectrum and they will declare: "I am really fucked up!" with varying prosody to suggest the end of the spectrum they perceive themselves to be at that given moment. That is assuming that they are not too delirious to speak. Use of the term highlights how subjective drug use is as well as the full spectrum of use. It removes any pretense that a legal intoxicant will be used primarily in a therapist's office or a room full of intellectuals focused on expanding their consciousness. We can't use a 10 point scale with the term on either end. We are not really treating anything. How many days during your life can you spend "fucked up" - whether or not the intoxicant is medically dangerous to you? Probably not too many if you expect to have a work, a social and a family life where you depend on other people and they depend on you. Probably not too many if you live in a dangerous environment like Minnesota and you have to decide at some point that you need to be wearing enough protective clothing outdoors to prevent frostbite, exposure, and death.
Hallucinogens or psychedelics are probably not the new miracle drugs simply because they have already been sold that way and it didn't work out. As two authors (13) closer to the history of LSD put it:
"....In all likelihood acid will continue to ravage as many people as it liberates and deceive as many as it enlightens. Whether it will play a more significant role in the future remains a matter of conjecture, for the psychedelic experience carries the impress of a constellation of social forces that are always shifting and up for grabs. It's not over yet."
My only qualifier is always that people with addictions will generally do worse.
George Dawson, MD, DFAPA
References:
1: Walter Isaacson. Steve Jobs. Simon & Schuster. New York. 2011. p 41.
2: Woodstock: Music from the Original Soundtrack and More. Cotillion Records. 1970.
3: Glennon RA. The pharmacology of hallucinogens and designer drugs. in Principles of Addiction Medicine, Fourth Edition. RK Ries, DA Fiellin, SC Miller, and R Saitz (eds); Wolters Kluwer/Lippincott Williams & Wilkins; Baltimore 2009: pp 215-230.
4: Domino EF, Miller SC. The pharmacology of dissociatives. in Principles of Addiction Medicine, Fourth Edition. RK Ries, DA Fiellin, SC Miller, and R Saitz (eds); Wolters Kluwer/Lippincott Williams & Wilkins; Baltimore 2009: pp 231-240.
5: Pechnick RN, Cunningham KA. Hallucinogens. in Substance Abuse: A Comprehensive Textbook, Fifth Edition. P Ruiz, E Strain (eds); Wolters Kluwer/Lippincott Williams & Wilkins; Baltimore 2011: pp 267-276.
6: McCann UD. PCP/Designer Drugs/MDMA. in Substance Abuse: A Comprehensive Textbook, Fifth Edition. P Ruiz, E Strain (eds); Wolters Kluwer/Lippincott Williams & Wilkins; Baltimore 2011: pp 277-283.
7: Krebs TS, Johansen PØ. Psychedelics and mental health: a population study. PLoS One. 2013 Aug 19;8(8):e63972. doi: 10.1371/journal.pone.0063972. eCollection 2013. PubMed PMID: 23976938; PubMed Central PMCID: PMC3747247.
8: Johansen PØ, Krebs TS. Psychedelics not linked to mental health problems or suicidal behavior: a population study. J Psychopharmacol. 2015 Mar;29(3):270-9. doi: 10.1177/0269881114568039. Epub 2015 Mar 5. PubMed PMID: 25744618.
9: Krebs TS, Johansen PØ. Reply letter: Mental health of people who have used classical psychedelics and no other illicit drugs. J Psychopharmacol. 2015 Sep;29(9):1036-40. PubMed PMID: 26649373.
10: Krebs TS, Johansen PØ. Over 30 million psychedelic users in the United States. F1000Res. 2013 Mar 28;2:98. doi: 10.12688/f1000research.2-98.v1. eCollection 2013. PubMed PMID: 24627778; PubMed Central PMCID: PMC3917651.
11: Logan BK, Goldfogel G, Hamilton R, Kuhlman J. Five deaths resulting from abuse of dextromethorphan sold over the internet. J Anal Toxicol. 2009
Mar;33(2):99-103. PubMed PMID: 19239735.
12: Larsen JK. Neurotoxicity and LSD treatment: a follow-up study of 151 patients in Denmark. Hist Psychiatry. 2016 Jun;27(2):172-89. doi: 10.1177/0957154X16629902. Epub 2016 Mar 10. PubMed PMID: 26966135.
13: Lee MA, Shlain B. The Complete Social History of LSD: The CIA, The Sixties, and Beyond. Grove Press, New York, 1985: p 294.
14: Mithoefer MC, Grob CS, Brewerton TD. Novel psychopharmacological therapies for psychiatric disorders: psilocybin and MDMA. Lancet Psychiatry. 2016 May;3(5):481-8. doi: 10.1016/S2215-0366(15)00576-3. Epub 2016 Apr 5. Review. PubMed PMID: 27067625.
12: Larsen JK. Neurotoxicity and LSD treatment: a follow-up study of 151 patients in Denmark. Hist Psychiatry. 2016 Jun;27(2):172-89. doi: 10.1177/0957154X16629902. Epub 2016 Mar 10. PubMed PMID: 26966135.
13: Lee MA, Shlain B. The Complete Social History of LSD: The CIA, The Sixties, and Beyond. Grove Press, New York, 1985: p 294.
14: Mithoefer MC, Grob CS, Brewerton TD. Novel psychopharmacological therapies for psychiatric disorders: psilocybin and MDMA. Lancet Psychiatry. 2016 May;3(5):481-8. doi: 10.1016/S2215-0366(15)00576-3. Epub 2016 Apr 5. Review. PubMed PMID: 27067625.
15: Johnson M, Richards W, Griffiths R. Human hallucinogen research: guidelines for safety. J Psychopharmacol. 2008 Aug;22(6):603-20. doi: 10.1177/0269881108093587. Epub 2008 Jul 1. Review. PubMed PMID: 18593734.
Attribution:
1: Krebs TS and Johansen PØ. Over 30 million psychedelic users in the United States [version 1; referees: 2 approved]. F1000Research 2013, 2:98 (doi: 10.12688/f1000research.2-98.v1)
Attribution:
Copyright: © 2013 Krebs TS and Johansen PØ. This is an open access article distributed under the terms of theCreative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
2: Figures 2 and 5 are from Substance Abuse and Mental Health Services Administration (SAMHSA) Emergency Department Data.
2: Figures 2 and 5 are from Substance Abuse and Mental Health Services Administration (SAMHSA) Emergency Department Data.
Sunday, May 22, 2016
Medical Treatment Is Never A Zero Risk Decision
 |
| Harvey W. Cushing, MD |
Ever since Medical Errors - the Third Leading Cause Of Death came out the media and bloggers have been abuzz with the headline. It is only a matter of time before we hear about how many full 747s crashing would equal the number of patients that are killed by physician errors each year. There are any number of articles in the press each day about how there are algorithms or checklists from some committee or government agency that will eliminate risk in medical diagnosis and procedures. There are an equal number of stories about how machine intelligence or will eliminate all of this human error. There was a story a few weeks ago about a robot that could suture up operative wounds from surgery. After seeing that robot in action, I would not want it anywhere near me or anyone I cared about. There is often palpable conflict of interest involved in the news stories. Stories designed to generate interest or influence politicians. Stories to express a political viewpoint. Even in the professional literature, much of what is written is a political viewpoint often to develop leverage against physicians and force them to do things in a certain way. The selling point to the public and their elected officials is that medicine, particularly physicians would perform better and more uniformly if they would adhere to certain protocols and that these protocols need to include the input of people who have never been trained as physicians - most notably business managers.
I can illustrate why these analyses are absurd based on an experience I had about 6 years ago. At that time my wife was struggling with intense ear pain and the provider she was seeing wanted to start her on another course of antibiotics for ear pain. I had her see an ENT surgeon instead, who performed an examination that only an ENT physician can do and then read the CT scan that he ordered. That CT scan was read as normal by the radiologist. This ENT physician not only read it as abnormal, but got additional imaging studies to demonstrate that my wife had a pituitary tumor. Referral to an endocrinologist confirmed that it was a growth hormone secreting tumor, further explaining additional symptoms that she had described to various physicians over the years. I went to work at that point and found the neurosurgeon who was one of the pioneers in transsphenoidal adenoma resections in the world. Although not malignant, the prognosis of these tumors is not benign with disfigurement from acromegaly, progressive endocrine abnormalities, and eventual congestive heart failure all from the effects of excessive growth hormone secretion. There were also complications of inadequate excision and secondary procedures like gamma knife irradiation in an attempt to obliterate the tumor. We were sitting in the consulting room of the neurosurgeon as soon as we could arrange it.
He had pulled up a coronal section of the MRI scan showing the tumor wrapped around my wife's right internal carotid artery. He made the following statement: "This is the tumor and this is the artery (pointing to areas on an MRI coronal view of the pituitary gland and surrounding anatomy). I am going to try to remove as much of the tumor as possible. If I accidentally nick the carotid artery in this area, there is nothing that can be done about it. That complication happens and I know good neurosurgeons who have had that happen to them. I can assure you I will remove only as much tumor as possible. I will remove only as much as I would remove if you were one of my family members."
This is the unspoken truth about medical errors and whether they are preventable or not. In this case doing nothing results in an inevitable slow death and severely compromised quality of life. The procedure is not without risk. In this case the risk was minimized by selecting the most skilled neurosurgeon in the area, but he openly acknowledges that nicking the carotid artery in a place that cannot be repaired is not only a possibility, but it happens to the best neurosurgeons. Any cursory analysis should illustrate why. We are talking about an operation that occurs in about a 1 1/2 inch space at the tip of an endoscope on a tumor that extends away from that tip into a small crevice between the carotid artery and sphenoid bone. Anyone really interested in this can go to YouTube and view several videos of the procedure from the view of the surgeon. In this case our neurosurgeon explicitly talked about the issue of how much tumor could be removed. He was acutely aware that the risk involved in removing too much tumor may be unacceptably high. Incompletely removing the tumor involves the risk of continued exposure to excessive growth hormone and the secondary gamma knife procedure. The fact that this surgery can be done at all seems like is a miracle to me. Early in my career, I had treated a patient who underwent a transtemporal approach to the same kind of tumor and that had resulted in significant postoperative disability.
In the decision to proceed my wife clearly found the risk acceptable because acromegaly and a slow death from endocrine complications and further procedures were not. The operative procedure went perfectly and 6 years later her growth hormone, IGH levels, and serial MRI scans show no tumor recurrence. I don't have to speculate about what might have gone wrong in my wife's case because Henry Marsh (6) writes about it in his compilation of neurosurgical complications Do No Harm. In the chapter "Pituitary Adenoma" he did a transphenoidal procedure on a man with acromegaly. His description of the relevant anatomy: "There are however, two major arteries next to the pituitary gland that can, if the surgeon is exceptionally unlucky, be damaged during the operation." His patient did well until post-operative day number 3, when suddenly his right arm was paralyzed and he could not communicate. Brain imaging confirmed a major left hemispheric stroke. Having no actual operative complications Marsh concludes: "This must have been caused in some unknowable way by the operation."
But let's take a look at what would have happened in my wife's case if there had been a complication or series of complications using the methodology cited by the authors in the studies. First off, in the case of a complication where does the chain of errors begin. The misdiagnosis of otitis media and two antibiotic prescriptions? The misread CT scan of the sphenoid bone? It seems like those are two preliminary errors right there even though neither was immediately threatening. Combined with a surgical error that would be three medical errors had a complication occurred. And what about the self correcting aspects of this process? Does the ENT surgeon get any credit here for correcting the misdiagnosis of otitis media or the misreading of the CT scan? Any focus on medical errors never looks at the self correcting aspects - how many times they are caught and how many times standard second opinions from colleagues or trusted referrals modify the treatment plan. How much morbidity and mortality would occur without this level of self correction? How is it estimated? The best example I can recall of the problems of error determination was in a NEJM editorial to address the first report on medical errors by the Institute of Medicine.
In that editorial (5), the lead author of some of the most quoted studies discusses the issue of the definition of errors, the definition of preventability, and the subjective nature of these determinations. His preliminary analysis is that the IOM conclusion that 44,000 to 98,000 deaths caused by medical errors "create an impression that is not warranted by the scientific work underlying the IOM report." That number has been inflated to more than 250,000 according to the recent quoted report (1). He also expresses an opinion completely consistent with Marsh's observations and goes on to point out that the observation of error can not cannot be reliably made by third party observers:
"Even with the best surgical technique and proper precautions, however, a hemorrhage can occur. We classified most postoperative hemorrhages resulting in the transfer of patients back to the operating room after simple procedures (such as hysterectomy or appendectomy) as preventable, even though in most cases there was no apparent blunder or slip-up by the surgeon. The IOM report refers to these cases as medical errors, which to some observers may seem inappropriate." (6)
He goes on to elaborate on four important aspects of the IOM report, 2 of which have to do with politics and public perception. The first is the idea that either nothing is being done about safety or that things are getting more dangerous. In many ways this is analogous to the public perception that violent crime is high when it is at a 30 year low. He gives an even better example of Harvey Cushing's accomplishments during his neurosurgical career. In 1913, the mortality rate for craniotomies for brain tumors was 80%. In twenty years it was reduced to 13%. Currently it is 1%. All of that without the IOM or any of the current federal or state regulators. The whole idea that physicians are motivated more by adhering to what politicians or regulators want rather than what is in the best interest of their patients has always been an incredible one to me. I guess it makes sense only if you are a politician or a regulator and you really believe that your naively designed incentives and disincentives have meaning. The second complication is increased reporting requirements and all of the complications that involves including the impact on confidential peer reviewed complications. Every physician has participated in some form of complications conferences or what surgeons used to call morbidity and mortality conferences. The modern goal of these conferences is to try to identify procedures and interventions to improve patients safety. Opening that system up to increased reporting and subjecting it to the "dead weight of the litigation system" is something the author cautions against, but is often explicit in the news headlines.
Makary thought the IOM missed the boat on the issue of how malpractice litigation is a risk against internally driven safety initiatives. I think they and subsequent authors missed the boat on the issue of biological variability. To some degree is it addressed by the subjective determination of preventability but not entirely. If a neurosurgeon is observed to have performed an errorless operation and the patient sustains significant complications, what are all of the factors that go into calling that an error or not? A lot of it may have to due with the baseline state of the patient. Are they already compromised by injury, illness or congenital variations. Neurosurgeons after all are not operating on healthy people. The example also applies to medicine and psychiatry. As an example, I usually tell people up front these days that there is about a 40% chance that they will noticeably improve with an antidepressant if their symptoms are significant. There is another 20 or 30% chance that they will feel somewhat better but not get back to their baseline state. There is a 10-20% chance that they will get significant side effects and not want to continue the medication and in a small number of cases (1-2%) there is a chance of really severe side effects from the medication. Pharmacogenomics suggests that it can be invaluable in this process, but there is variability between predictions using the available analyses from the same manufacturer and between manufacturers. Even with that warning there are a number of people who will consider it an "error" that they received a medication that caused them to get a rash or in the worst case serotonin syndrome. I think that there is a natural tendency for some to see any medical procedure that does not go well to be attributable to error on the part of the physician. I think that the personal experience of most physicians will bear that out.
Another less well known intervention in psychiatry is the care of the chronically suicidal person. Many of these persons have a history of serious suicide attempts and remain at significant risk. The usual risk factor analysis of their suicide potential does not add very much. There are frequently inadequate resources to treat them or they refuse to access what is available. Frequent short term admissions to inpatient units adds nothing to their care. The psychiatrist who accepts their care usually is seeing them more intensely and accepting more crisis calls from them than other patients. Until a sufficient therapeutic alliance develops, there may be many sessions with a lot of depression and anger and very little objective information on what the patient is thinking. The psychiatrist and patient in this case need to accept that the risk involved in this situation from suicide or a suicide attempt - is necessary to make progress and enhance the patient's ability to function and enjoy life.
My main point here is that people currently need to assume some risks in order to get better. There is nobody more than physicians who would want medicine to be a no risk endeavor, but the reality is that is not going to happen anytime soon. All patients realize this at some level, but that may do little to mitigate the anger or disappointment when it occurs. Every family has a tale to tell about a medical miracle or a medical mistake. In the situations like my wife faced with my support, people are clearly willing to take the risk in face of undesirable consequences. The physicians involved see this as very serious work. Should the classification of medical errors be refined and analyzed? Of course they should - but the approach being used in the press invoking planes full of patients being sent to their death by physicians being equated to terrorists is not accurate or helpful. The backlash is significant and impairs the ongoing error analysis and correction process. Equating a heterogenous collection of complications classified by different methods as errors and listing them as a standard cause of death is also not accurate or helpful to the science of medical error analysis and correction.
George Dawson, MD, DFAPA
References:
1: Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ. 2016 May 3;353:i2139. doi: 10.1136/bmj.i2139. PubMed PMID: 27143499.
3: Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, Hebert L, Newhouse JP, Weiler PC, Hiatt H. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991 Feb 7;324(6):377-84. PubMed PMID: 1824793.
4: Localio AR, Lawthers AG, Brennan TA, Laird NM, Hebert LE, Peterson LM, Newhouse JP, Weiler PC, Hiatt HH. Relation between malpractice claims and adverse events due to negligence. Results of the Harvard Medical Practice Study III. N Engl J Med. 1991 Jul 25;325(4):245-51. PubMed PMID: 2057025.
5: Brennan TA. The Institute of Medicine report on medical errors--could it do harm? N Engl J Med. 2000 Apr 13;342(15):1123-5. PubMed PMID: 10760315.
6: Marsh H. Do No Harm: Stories Of Life, Death, And Brain Surgery. Thomas Dunne Books/ St. Martin's Press; New York, NY; 2014.
Attribution:
Portrait of Harvey Cushing, MD by Edmund C. Tarbell [Public domain], via Wikimedia Commons at https://commons.wikimedia.org/wiki/File%3ADr_Harvey_Cushing_Edmund_Tarbell_1908.jpeg accessed on May 22, 2016.
Supplementaries:
Supplementary 1: Another excellent example of biological variability is joint replacement surgery. I see patients, friends and family members who have mixed experiences. The majority turn out very well, in some cases extremely well. In the case of extremely good joint replacement surgery, according to all of these people I talk to, the surgeon seems to discourage them talking to other people about how good the results were, generally by telling them that they had an extraordinary result in terms of how the replaced joint functions.
Supplementary 2: A good example from a recent post about the aggressive treatment of pain and the risk of addiction and overdose deaths. 20 years ago when physicians were being criticized by various factions for not aggressive enough use of painkiller prescriptions and the use of opioids for chronic noncancer pain - the risk of death by overdose was minimized by those proponents. Now that there is a clear cause of death from overuse of opioids and the rates of addiction have increased - physicians are faulted for not knowing how to prescribe opioids. It seems like they had a better idea 20 years ago before yielding to the critics. From the perspective of this post - there is always risk either way. Only politicians and regulators can deny that.
Supplementary 3: The Twitter graphic ( and yes I am serious). The IOM did not start until about 1970. None of these entities has a track record remotely close to Harvey Cushing in the 1920s and 1930s.
6: Marsh H. Do No Harm: Stories Of Life, Death, And Brain Surgery. Thomas Dunne Books/ St. Martin's Press; New York, NY; 2014.
Attribution:
Portrait of Harvey Cushing, MD by Edmund C. Tarbell [Public domain], via Wikimedia Commons at https://commons.wikimedia.org/wiki/File%3ADr_Harvey_Cushing_Edmund_Tarbell_1908.jpeg accessed on May 22, 2016.
Supplementaries:
Supplementary 1: Another excellent example of biological variability is joint replacement surgery. I see patients, friends and family members who have mixed experiences. The majority turn out very well, in some cases extremely well. In the case of extremely good joint replacement surgery, according to all of these people I talk to, the surgeon seems to discourage them talking to other people about how good the results were, generally by telling them that they had an extraordinary result in terms of how the replaced joint functions.
Supplementary 2: A good example from a recent post about the aggressive treatment of pain and the risk of addiction and overdose deaths. 20 years ago when physicians were being criticized by various factions for not aggressive enough use of painkiller prescriptions and the use of opioids for chronic noncancer pain - the risk of death by overdose was minimized by those proponents. Now that there is a clear cause of death from overuse of opioids and the rates of addiction have increased - physicians are faulted for not knowing how to prescribe opioids. It seems like they had a better idea 20 years ago before yielding to the critics. From the perspective of this post - there is always risk either way. Only politicians and regulators can deny that.
Supplementary 3: The Twitter graphic ( and yes I am serious). The IOM did not start until about 1970. None of these entities has a track record remotely close to Harvey Cushing in the 1920s and 1930s.
Subscribe to:
Posts (Atom)