Like them or not the FDA is the critical agency in terms of pharmaceutical regulation and the politics of pharmaceuticals. It is easy to confuse the politics of drugs with pharmaceutical science. Clear examples include special interest groups lobbying the FDA and members of Congress for rapid access to medications that have not been approved for specific indications. Some of those medications have significant side effects and very low therapeutic efficacy. At the same time, the FDA is criticized for approving medications that add nothing to the existing pharmacopeia or that have marginal evidence for efficacy. If you view medications as tools that need to be applied in various on and off label ways by practicing physicians, that is by definition a lower threshold for regulatory approval than the standard that a medication must be very effective and very safe. It turns out that there are very few medications with that profile. Some problems and inconsistencies are more glaring than others.
I was surprised to get a recent warning letter from the FDA on an inhaled preparation of loxapine called Adasuve. Loxapine is an antipsychotic drug of medium potency. Back in the late 1980s we had a drug trial of loxapine versus haloperidol on one of the inpatient units I was running at the time. It was a fairly effective drug for acute symptoms of psychosis and was less potent than haloperidol so it has fewer neurological side effects. It never seemed like a very popular medication with psychiatrists. There was some recurrent interest around the issue of first and second generation antipsychotics with some authors suggesting that it had a receptor profile that was more similar to second generation or atypical antipsychotics. During the initial period when it was approved and marketed under the brand name Loxitane it was available in both oral and injectable forms.
I could only locate one study at PubMed on the Adasuve in the current medical literature searching on the brand name. There were 20 studies at clinicaltrials.gov web site but unfortunately no results were posted. Some of them appear to be very interesting including one that looks at the QTc interval effects of inhaled loxapine. A review of the Adasuve web site shows that bronchospasm is a black box warning and that there is a Risk Evaluation and Mitigation Strategy (REMS) to assess prior to prescribing and monitoring the patient after each administered dose. It looks like it can only be given in a registered health care facility by personnel who can assess and manage any pulmonary complications. Although the pulmonary conditions that contraindicate use seem fairly straightforward (asthma, COPD, any pulmonary diagnosis associated with bronchospasm) the actual diagnoses are probably more complex due to a number of factors including smoking status, body weight, and the complexity of the underlying pulmonary syndromes. Staff administering this medication should assess the patient for pulmonary problems at every episode and not depend on historical diagnoses.
From a philosophical standpoint, there needs to be an active debate about new patents or patent extensions on medications that are currently generic drugs like loxapine. During the time it was primarily used it certainly did not demonstrate any superior efficacy or side effect profile relative to other typical or atypical antipsychotics. Loxapine is metabolized to amoxapine, an FDA approved antidepressant that has been used on a limited basis in psychiatric practice and is generally not considered a first or second line antidepressant. The metabolic relationship led some authors to speculate that the combination may be effective in psychotic depression but that application was never realized. So in this case we have a drug with limited applications that has been repackaged in a riskier dosage form. That seems like several steps in the wrong direction. The details about the pharmacokinetics are available in the package insert. Looking at this data, the main advantage appears to be the short time is takes to reach maximum plasma concentration (1-2 minutes). A useful study here would have looked at a subgroup of patients taking parenteral loxapine and similar pharmacokinetic measures. In the study I alluded to from the 1980s loxapine was compared directly to haloperidol for acute agitation in schizophrenia or bipolar disorder.
With this medication released into practice, if I was still working on an acute inpatient unit I would be very skeptical of using this medication for acute agitation. Use is limited to a single dose in a 24 hour period. The people who need this medication are generally medically complex, may still have street drugs in their system, are generally cigarette smokers and their pulmonary and in many cases their cardiac status may be unknown. If the initial dose is not effective, the question becomes - now what? Patient preference may be an issue since some patients request a fast acting medication but they do not want parenteral injections. Patients with an addiction history may have used drugs by insufflation, inhalation, and intravenous injection and that may be a factor in their decision making. All other factors considered there have been studies of patient preference for specific medications to treat acute agitation and of the antipsychotic class of medications only olanzapine is highly rated. Besides the degree of acceptance, post marketing surveillance will be important in terms of medication side effects. The current approval was based on pooled data from three studies looking at a total of 259 patients getting the active medication and 263 patient receiving placebo. That is not many doses of this medication.
Zohydro probably requires less discussion. Zohydro is advertised as the only acetaminophen free, extended release form of hydrocodone available in the United States. It is available in dosage forms ranging from 10 mg to 50 mg intended as a twice-a-day dose schedule. Zohydro comes with the following black box warning:
The interesting part of this approval process was that the scientific advisory panel, for the FDA voted overwhelmingly against approving this medication, but it was approved anyway. We are currently in the midst of an opioid epidemic based on a number of metrics including emergency department visits for complications, deaths from accidental overdose, per capita consumption of opioids relative to the rest of the world, and the increasing number of people addicted to opioids. We are also entering a period of increased policing of physicians by numerous agencies for opioid prescribing practices. There is fairly good evidence that the "opioid epidemic" started with a pain treatment initiative suggesting that physicians were not treating pain aggressively enough. The pendulum has swung to the point where there will be clear blame for at least some physicians who are using opioids to treat chronic pain.
There are a couple of additional problems with the FDA approved package insert for Zohydro. The first is the Indication or reason the FDA approved this drug in the first place. The indication for Zohydro is: ".....the management of pain severe enough to require daily, around-the-clock, long-term opioid treatment for which alternative treatment options are inadequate." That is a shockingly inadequate description of a pain syndrome. In keeping with a medication as a tool model for regulatory approval this is acceptable. But any physician prescribing this medication should have a more specific pain diagnosis that specifically addresses the chronicity of the pain and why this might be an acceptable approach.
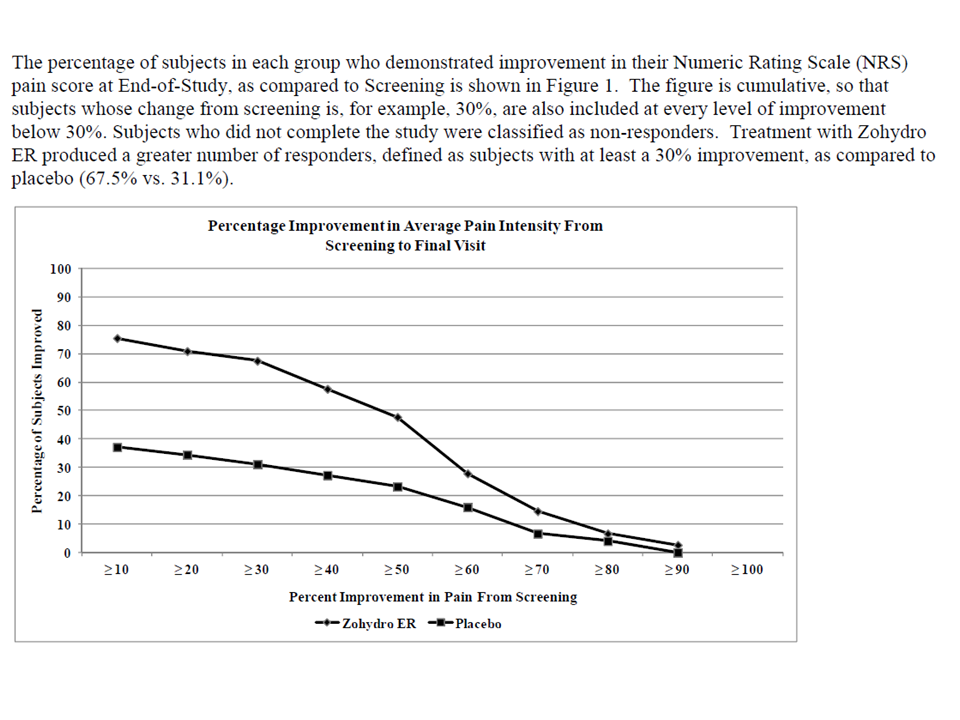
The second problem on my first read through of the package insert is the following graphic of the efficacy of this medication. It plots the results of an study of Zohydro versus placebo in 510 subjects who were already on chronic opioid therapy for chronic back pain.
I think that these examples highlight the fact that the FDA does not seem to have any guiding philosophy when it comes to some new drug approvals of repackaged generics other a Darwinian free market approach. Since the original drug passed the safety and efficacy standards why wouldn't the repackaged generic? Physicians should demand a more specific regulatory approach. At the minimum there needs to be clearer evidence of an advance in pharmacotherapy in terms of increased efficacy or a better side effect profile. Repackaging generic drugs without that kind of guidance and obvious risks seems like a mistake to me. There also needs to be a better approach to chronic pain and drugs that are clearly addictive and a more uniform methodology for measuring efficacy. Most studies looking at opioid use in chronic pain show modest pain relief at best. In clinical practice, the relief is generally on the order of what is expected with non-opioids on population wide comparisons. There should be an easy way to operationalize that knowledge and instruct pharmaceutical manufacturers on the appropriate design of clinical trials to answer these questions. There is also the issue of conflict of interest and the need for complete disclosure of who is advocating for the use of the medications in question.
From an addiction standpoint, hydrocodone and acetaminophen compounds are some of the most frequently diverted and abused compounds. It is not uncommon to get a history of people taking amounts that are the equivalent of chronic overdoses with the acetaminophen component. Many if not most of the people with this addiction are aware of the risks of the acetaminophen component but when the chronic phase of the addiction develops they will continue to use it and ignore that danger. Patient preferences can be a factor in the decision to prescribe an opioid. Hydrocodone combination medications are in high demand on the street indicating to me that is is a preferred product to many addicts. The package insert contains remarkably little useful practical information on abuse, dependence, and addiction. We are told that there is a REMS strategy and that the FDA is requiring manufacturers of newly approved long acting opioids to conduct long term follow up studies to look at the "serious risks of long term use."
I think it would be a lot easier if FDA regulators just looked at the current data on the CDC web site about the addiction risk of opioids and answer the question: "Why would Zohydro be any different?"
George Dawson, MD, DFAPA
FDA. Adasuve Full Prescribing Information. (Click on appropriate link).
European Medicines Agency. Adasuve EPAR (European Public Assessment Report).
Additional Clinical Note 1: On 1/14/2014 the FDA issued a recommendation that health professionals stop using combination products that contain more than 325 mg acetaminophen. That same page has a link to a letter that will be sent to manufacturers that these dose strengths be withdrawn over the next three years. Based on their rationale (no increased efficacy with acetaminophen and risk for hepatotoxicity), I don't know why 325 mg acetaminophen is the magic number. The addiction experience with combination products suggest that people will routinely use potentially toxic doses as part of their addiction, even when they know that there is a potential problem with the amount of acetaminophen. This new rule may increase increase the amount of opioids prescribed.
Thursday, January 9, 2014
Monday, January 6, 2014
It Is Cold Outside
I was driving into work this AM. I drive a six year old Toyota Van. The thermometer on my rearview mirror hovered between - 20 and -21 Fahrenheit, but every bank I passed said -24. Before I left home this morning I added a layer of polyester, packed additional headgear, and wore my Sorel boots. This is serious weather even if you are born and raised here and you need to be prepared for the worst. Standing outside for even a few minutes without adequate cover can result in frostbite or worse. The Governor of Minnesota closed down all of the schools today to prevent frostbite injuries and so far there have been no arguments with that decision. The drive home at night was slightly warmer at -16 degrees. The sky was so clear it was like being in outer space. I had to stop for gas and the driver's side door froze open. I had to hold it shut for about 6 miles until it thawed to the point I could slam it.
Apart from the pragmatics of winter survival, the cold weather also triggers a lot of associative memories - starting with my Sorels. I got these boots originally in 1971 in order to do a Limnology experiment on Lake Superior.
A friend of mine helped me and we went out onto the ice for a about 5 hours and pumped about 200 gallons of lake water through a plankton net to look at the winter plankton population. It was about -5 degrees that day. A few years earlier he had a case of frostbite after walking about 10 blocks to school wearing nothing but a pea coat. Like a lot of people in the northern US and Canada, I have found that these boots absolutely protect your feet in subzero weather.
I lived in Duluth, Minnesota for a while and can recall trying to speedskate when it was -10 to -15 degrees. At that temperature, a skate blade cannot compress and liquefy the ice enough to support much glide so the skating motion and its mechanics are seriously disrupted. I was wearing two layers of polyester, a layer of Lycra, and a layer of fiber. Unlike Sorels - speedskates even with neoprene boot covers don't protect much against the cold. When I got home I had to lay on top of a radiator under a blanket for 30 minutes in order to warm up. The coldest I have ever been in the winter usually happens after falling through the ice. I can recall walking across a creek and just getting ready to step up onto the far bank when I fell through the ice up to my chest in icy water. The sensation that occurs when that happens is incredible. Your breathing stops for a while followed by rapid gasping as you struggle to get out of the water. That is followed by the desperate run home. In my case it was only about 7 blocks and by the time I got there my clothes were frozen solid. A friend of mine was skating on Lake Superior and fell through the ice catching himself only by his fingertips. He ran home about the same distance but he had been totally submerged.
My more recent memories are about how the cold has been a factor in my role as a psychiatrist. Most psychiatrists in the Midwest have first-hand experience with the complications of cold weather. We have seen people with frostbite injuries both on burn units and after they have been transferred. We know many of the people who are caught in the endless inpatient unit -> emergency department -> homeless cycle that seems like a permanent artifact of our managed care inpatient and county mental health systems. We have seen the human interest stories that tend to run in the papers when the potentially lethal cold weather hits and the temporary concern about whether or not there are enough shelter beds.
Weather this cold does not allow you to make a lot of mistakes. Sometimes all it takes is the idea that you can run out to the trash can without putting on a jacket and finding that you have locked yourself out of the house. People with memory problems and disorientation can wander off and get lost. People with drinking problems can pass out or just take too long to get home. All it takes is a decision that keeps you out in the subzero weather for minutes too long and you can be in serious trouble.
Potentially lethal cold weather is also an integral part of treatment decisions. You can't really watch people coming in to appointments wearing summer clothing in this weather without doing an assessment for cold weather safety. It becomes part of the discharge decision making. Exactly how stable is the person's housing and how likely are they to keep themselves safe? Can they walk 10 blocks from the hospital to their apartment wearing a sweat suit, basketball shoes, and no hat? Should they be discharged to the street, even if they want to be? Should they be discharged if a managed care reviewer says that they should be discharged? We are generally talking about people who have chronic problems with insight and judgment. What about people with suicidal ideation? What about the person with chronic drug problems who has a history of drug induced blackouts and waking up on park benches? What about the person with Alzheimer’s disease who does not have 24 hour supervision?
How do you make an unbiased decision in that context? I can say that you don’t. You don’t because as a psychiatrist you are aware of all of the adverse outcomes. The continuum of severe frostbite injuries to the hypothermic who could not be resuscitated to those who were found frozen to death. You don’t want to see that happen to anyone. You don’t care if somebody wants to call that paternalistic. You don’t really care if it costs a managed care company or (more likely) a hospital a few bucks. You have been there yourself and you know you cannot take any chances in subzero weather. It’s not about a fear of being sued, it’s about concern for a fellow human being.
There are implications for the imminent dangerousness standard that is commonly applied to involuntary holds. I have argued with enough county attorneys over the years to understand that the standard itself is purely subjective and arbitrary. No matter how it appears on paper you will hear ten different interpretations from 10 different county attorneys. There are a few states where a gravely disabled standard applies. That standard states that a person may have problematic judgment to the point that it potentially impacts their ability to secure adequate food, medical care, or housing. That standard probably generally applies in these situations, but if you happen to be in a state where there is no statute or the county courts ignore it for convenience or financial reasons it may not be available for use.
Those are the kinds of things I think about when it gets this cold. I do get the occasional lighthearted thoughts – making sure I recall the thermodynamic equations that show my car battery dependent on temperature and telling myself that I am going to call Columbia and ask them if they make some type of expedition wear that is warmer than my current Titanium coat. But mostly – I hope the most vulnerable among us get the help they need and nobody gets injured or killed. Hopefully someday people will think about the fact that some people have a hard time protecting themselves - irrespective of the air temperature.
George Dawson, MD, DFAPA
Andy Rathbun. Regions Hospital Sees "Record-Breaking" Number of Frostbite Cases. St. Paul Pioneer Press. January 6, 2013.
From the article:
"Most of the people that come in with severe frostbite are "in some way compromised," he said. A small number are physically or mentally disabled, but a majority are people who have consumed too much alcohol or were abusing drugs and didn't realize how cold it was outside, Edmonson said."
Wednesday, January 1, 2014
What Is Really Going On At The Minnesota Security Hospital?
The Minneapolis StarTribune posted a recent story about the Minnesota Security Hospital (MSH) on December 27, 2013 that was updated today. The article raises concerns about patient treatment and safety at this facility both for patients and staff. It should be read by everyone with an interest in how state mental hospitals function. It is of particular interest to Minnesota residents who may have a relative being treated at this facility but also anyone concerned about the image of the state and how it treats residents with severe mental illnesses. From a policy standpoint it should be an issue of great importance for both local psychiatric societies and the American Psychiatric Association (APA).
Let me preface my remarks by saying that I have no inside knowledge of what is occurring at the MSH beyond what I read in the papers. The first concern is about the information base for the article and who is interpreting that information. That is contained in the fourth paragraph of the article at the very end of that paragraph:
"Nearly two years after the hospital's professional psychiatric staff departed in a mass resignation, the state still has not hired a full complement of psychiatrists, documents show. Basic medical record-keeping has been neglected, employees have been placed in danger and patients have been discharged with inadequate safeguards, according to internal memos, federal records, and agency files reviewed by the Star Tribune."
The problem here is that there is nobody at the Star Tribune who is an expert in the treatment of patients with severe mental illness and aggression. The second problem is that there is a significant conflict of interest anytime a journalist has access to clinical material with a potential sensational interpretation. From my experience journalists will make that interpretation out of ignorance or for the purpose of enhancing the dramatic impact of the story. In this article the names of two patients are disclosed. Journalists are not confidentiality bound to not disclose the names of patients and there may be some public documents with the names of these patients. My experience with journalists has been that they want to talk to actual patients with real names, and really do not understand the problems with that. There are always many potential weaknesses when considering a journalistic source.
There is a precedent for the review of confidential hospital records by expert unbiased reviewers and that was the Medicare Peer Review Organizations (PRO) system. In that process, physicians who were experts in the field in question were rigorously screened for conflicts of interest. As an example, they could not have any affiliation however peripheral with the hospital or clinic being reviewed. The compensation for reviewing the records was trivial and you could not make a living at it. Reviewers were expected to be practicing medicine full time and not be an administrator. As a reviewer, I reviewed tens of thousands of pages of hospital records - many from state hospitals for both quality problems and utilization problems. A newspaper reporter looking at a patchwork of records, memos, and files from multiple sources is hardly an adequate standard to draw any conclusions. A reporter can make it seem like the hospital is a "bad" place for restraining people or in this case failing to restrain a person.
A potentially rich source of information is the hospital's former medical director - Dr. Jennifer Service. She has one quote in the article about how the MSH is "broken", but it provides no details. My speculation is that there is nobody who had a better front row seat to what happened than Dr. Service and possibly the previous medical director. In the treatment of severe mental illness and aggression the medical director or clinical director has a critical role in making sure that there are no administrative factors that adversely affect the treatment team or their ability to provide care and a safe environment. A common mistake is that administration believes it can effect change and they do not pay close enough attention to the impact on the clinicians providing care. When treating aggressive people any environmental change like that can result in increasing aggression and chaos in the treatment environment. The Legislative Auditor's Report suggests several areas where the therapeutic neutrality of the environment and staff cohesion were problematic. During 23 years of conducting team meetings, my experience was that psychiatrists are an integral part of the team and should be the team member most experienced in team dynamics, countertransference, and approaches to violence prevention. There is no indication that occurred on teams at the MSH and in fact, participation is described as marginal.
There are other potential conflicts of interest here that potentially bias the story. Minnesota Department of Human Services apparently administers the place. In this case Commissioner Anne Barry talks about the goal of increasing the likelihood of discharge by making community living environments more available. Since DHS also administers all of those environments in the state it should be a relatively easy task. Why is it not being done? Are there people who realistically cannot be discharged without recreating a hospital environment for them in the community? In the cases where that has happened have there been more adverse outcomes? Are those environments more humane than the hospital environment where the patient was initially? The Deputy Commissioner talks about accountability, but DHS seems like one of the most opaque state agencies out there. Lately they seem to have moved into the area of micromanagement of the treatment providers especially around the issue of aggressive behavior. Are the administrators of DHS responsible for the failed programs at the MSH? Commissioner Barry talks about a more "therapeutic environment". Is she qualified to determine what that is? And finally the Legislative Auditor's Report alludes to a report by previous consultants. Who were these consultants and where is that report?
Another good illustration of how conflicts of interest potentially bias the StarTribune article was the issue of accusations of maltreatment by professional staff. The first is an allegation that a psychiatrist "committed maltreatment" by threatening an uncooperative patient with electroconvulsive treatment. DHS investigators concluded that this happened but their finding was overturned by the DHS Inspector General. The State Ombudsman for Mental Health and Developmental Disabilities apparently believed it happened and made a request for the DHS Commissioner to reconsider the finding. The Inspector referred the matter to the Board of Medical Practice. In the second case, 2 nurses were accused of maltreatment. From the way the article is written it appears to be related to the incident where the patient was "slamming his head repeatedly into a concrete wall" and they were unable to get an order to physically restrain the patient. The nurses were fined and reported to the nursing board. Based on the incidents of maltreatment and another incident where a patient did not receive timely assessment for a stroke the DHS Commissioner extended the hospital's probation through 2014. There are many problems with employees paying the price for chaos in the system. Administrators often do not recognize the professional obligations of the staff. I have personally seen quality psychiatric staff paralyzed by indecision that was brought about by administrative mandate or personnel problems. The other problem here is that DHS appears to be the administrator, investigator and judicial process rolled into one. We have a number of political appointees (DHS, Ombudsman, Board of Medical Practice) charged with deciding the professional fate of a physician who seems to be practicing in the worst of possible scenarios. It should not be too surprising that MSH is unable to recruit and hire psychiatric staff.
The Legislative Auditor's Report is probably a better source of information than the newspaper report, but it has the same lack of input from experts. It is useful from the perspective of bureaucratic information on the details that can be counted like the number of psychiatric contacts, number of hours of therapeutic contact, number of staff injuries for a certain period of time, etc. One of the areas that is most interesting to me as a psychiatrist is the frequency of patient contact by psychiatrists. The report gives an example of a recent census of 321 patients. It provides an exhibit showing that from a policy standpoint the suggested frequencies of contact are monthly, quarterly, or semi-annually. These frequencies are interestingly lower than the frequency of contact in some 19th century German asylums. I can recall that Binswanger made a point of seeing all 200 patients in his asylum every week. The report said that of the 321 patients in the study 45% had been seen in the previous month, an additional 24% 1-2 months earlier, 17% 2-3 months before and 4% greater than 3 months before. Going from a full complement of eight psychiatrists to a total of two psychiatrists and 1 nurse practitioner is an obvious problem in terms of contact. Actual contact with psychiatrist is an insufficient metric for treating patients and other quality measures need to be developed.
If the article and the Legislative Auditor's report are even partially accurate with regard to facts, the glaring problem here appears to be that there is nobody in charge who knows how to run a hospital that treats people with severe mental illness and problems with aggression. It is probably more correct to say that at this point we have not been presented with any positive evidence that there is a person in charge with the necessary qualifications. The information presented in the StarTribune article does not suggest a clash of cultures. There is no psychiatric hospital culture that I am aware of where there is confusion about whether or not a patient should be allowed to injure themselves. The second problem is that this hospital needs psychiatrists who are trained to treat severe mental illness and aggression. They do not need to be forensic psychiatrists, but they do need expertise in treatment of severe mental illness. Forensic psychiatrists are basically needed to perform specific evaluations of criminal responsibility but the priority here is described as patient and staff safety. The people needed in this situation currently work in a number of acute care and community settings. They are very comfortable with the treatment of major psychiatric disorders and the associated medical comorbidity. It is safe to say that they enjoy working with these problems and talking with the people who have them. They are also sensitive to the needs of their co-workers and can establish the necessary environment of mutual trust and neutrality needed to succeed.
There may not be anyone around who remembers that Minnesota has solved a similar problem in the past. The year was 1990 and there were significant problems staffing the major state hospital in the system - Anoka Metro Regional Treatment Center. At that time, a Medical Director who was recently out of training was hired and he hired several colleagues from the same generation. They were all enthusiastic and interested in providing quality care. The state offered them competitive salaries. Within a very short period of time a cohesive staff developed and they became a favored training site for medical students. Treatment at the state hospital improved dramatically and several of the psychiatrists in that cohort went on to become leaders in the state in the provision of psychiatric services to patients with severe mental illness.
That still seems like a good idea today.
George Dawson, MD, DFAPA
Paul Mcenroe. Minnesota Security Hospital: Staff In Crisis Spreads Turmoil. StarTribune, December 27, 2013.
Office of the Legislative Auditor. Evaluation Report: State-Operated Human Services. February 2013.
Additional Clinical Note 1: Looking back over my post it is clear that I do not answer the question that is the title. Like most people I am speculating based on an imperfect data set. The main difference is that I am also speculating as an expert based on what needs to happen to provide the safest scientifically based treatment for people who are mentally ill, aggressive, and may have failed most if not all of the available treatments. I also recall that some past state hospital problems were resolved that has not been brought up in the discussion so far.
Let me preface my remarks by saying that I have no inside knowledge of what is occurring at the MSH beyond what I read in the papers. The first concern is about the information base for the article and who is interpreting that information. That is contained in the fourth paragraph of the article at the very end of that paragraph:
"Nearly two years after the hospital's professional psychiatric staff departed in a mass resignation, the state still has not hired a full complement of psychiatrists, documents show. Basic medical record-keeping has been neglected, employees have been placed in danger and patients have been discharged with inadequate safeguards, according to internal memos, federal records, and agency files reviewed by the Star Tribune."
The problem here is that there is nobody at the Star Tribune who is an expert in the treatment of patients with severe mental illness and aggression. The second problem is that there is a significant conflict of interest anytime a journalist has access to clinical material with a potential sensational interpretation. From my experience journalists will make that interpretation out of ignorance or for the purpose of enhancing the dramatic impact of the story. In this article the names of two patients are disclosed. Journalists are not confidentiality bound to not disclose the names of patients and there may be some public documents with the names of these patients. My experience with journalists has been that they want to talk to actual patients with real names, and really do not understand the problems with that. There are always many potential weaknesses when considering a journalistic source.
There is a precedent for the review of confidential hospital records by expert unbiased reviewers and that was the Medicare Peer Review Organizations (PRO) system. In that process, physicians who were experts in the field in question were rigorously screened for conflicts of interest. As an example, they could not have any affiliation however peripheral with the hospital or clinic being reviewed. The compensation for reviewing the records was trivial and you could not make a living at it. Reviewers were expected to be practicing medicine full time and not be an administrator. As a reviewer, I reviewed tens of thousands of pages of hospital records - many from state hospitals for both quality problems and utilization problems. A newspaper reporter looking at a patchwork of records, memos, and files from multiple sources is hardly an adequate standard to draw any conclusions. A reporter can make it seem like the hospital is a "bad" place for restraining people or in this case failing to restrain a person.
A potentially rich source of information is the hospital's former medical director - Dr. Jennifer Service. She has one quote in the article about how the MSH is "broken", but it provides no details. My speculation is that there is nobody who had a better front row seat to what happened than Dr. Service and possibly the previous medical director. In the treatment of severe mental illness and aggression the medical director or clinical director has a critical role in making sure that there are no administrative factors that adversely affect the treatment team or their ability to provide care and a safe environment. A common mistake is that administration believes it can effect change and they do not pay close enough attention to the impact on the clinicians providing care. When treating aggressive people any environmental change like that can result in increasing aggression and chaos in the treatment environment. The Legislative Auditor's Report suggests several areas where the therapeutic neutrality of the environment and staff cohesion were problematic. During 23 years of conducting team meetings, my experience was that psychiatrists are an integral part of the team and should be the team member most experienced in team dynamics, countertransference, and approaches to violence prevention. There is no indication that occurred on teams at the MSH and in fact, participation is described as marginal.
There are other potential conflicts of interest here that potentially bias the story. Minnesota Department of Human Services apparently administers the place. In this case Commissioner Anne Barry talks about the goal of increasing the likelihood of discharge by making community living environments more available. Since DHS also administers all of those environments in the state it should be a relatively easy task. Why is it not being done? Are there people who realistically cannot be discharged without recreating a hospital environment for them in the community? In the cases where that has happened have there been more adverse outcomes? Are those environments more humane than the hospital environment where the patient was initially? The Deputy Commissioner talks about accountability, but DHS seems like one of the most opaque state agencies out there. Lately they seem to have moved into the area of micromanagement of the treatment providers especially around the issue of aggressive behavior. Are the administrators of DHS responsible for the failed programs at the MSH? Commissioner Barry talks about a more "therapeutic environment". Is she qualified to determine what that is? And finally the Legislative Auditor's Report alludes to a report by previous consultants. Who were these consultants and where is that report?
Another good illustration of how conflicts of interest potentially bias the StarTribune article was the issue of accusations of maltreatment by professional staff. The first is an allegation that a psychiatrist "committed maltreatment" by threatening an uncooperative patient with electroconvulsive treatment. DHS investigators concluded that this happened but their finding was overturned by the DHS Inspector General. The State Ombudsman for Mental Health and Developmental Disabilities apparently believed it happened and made a request for the DHS Commissioner to reconsider the finding. The Inspector referred the matter to the Board of Medical Practice. In the second case, 2 nurses were accused of maltreatment. From the way the article is written it appears to be related to the incident where the patient was "slamming his head repeatedly into a concrete wall" and they were unable to get an order to physically restrain the patient. The nurses were fined and reported to the nursing board. Based on the incidents of maltreatment and another incident where a patient did not receive timely assessment for a stroke the DHS Commissioner extended the hospital's probation through 2014. There are many problems with employees paying the price for chaos in the system. Administrators often do not recognize the professional obligations of the staff. I have personally seen quality psychiatric staff paralyzed by indecision that was brought about by administrative mandate or personnel problems. The other problem here is that DHS appears to be the administrator, investigator and judicial process rolled into one. We have a number of political appointees (DHS, Ombudsman, Board of Medical Practice) charged with deciding the professional fate of a physician who seems to be practicing in the worst of possible scenarios. It should not be too surprising that MSH is unable to recruit and hire psychiatric staff.
The Legislative Auditor's Report is probably a better source of information than the newspaper report, but it has the same lack of input from experts. It is useful from the perspective of bureaucratic information on the details that can be counted like the number of psychiatric contacts, number of hours of therapeutic contact, number of staff injuries for a certain period of time, etc. One of the areas that is most interesting to me as a psychiatrist is the frequency of patient contact by psychiatrists. The report gives an example of a recent census of 321 patients. It provides an exhibit showing that from a policy standpoint the suggested frequencies of contact are monthly, quarterly, or semi-annually. These frequencies are interestingly lower than the frequency of contact in some 19th century German asylums. I can recall that Binswanger made a point of seeing all 200 patients in his asylum every week. The report said that of the 321 patients in the study 45% had been seen in the previous month, an additional 24% 1-2 months earlier, 17% 2-3 months before and 4% greater than 3 months before. Going from a full complement of eight psychiatrists to a total of two psychiatrists and 1 nurse practitioner is an obvious problem in terms of contact. Actual contact with psychiatrist is an insufficient metric for treating patients and other quality measures need to be developed.
If the article and the Legislative Auditor's report are even partially accurate with regard to facts, the glaring problem here appears to be that there is nobody in charge who knows how to run a hospital that treats people with severe mental illness and problems with aggression. It is probably more correct to say that at this point we have not been presented with any positive evidence that there is a person in charge with the necessary qualifications. The information presented in the StarTribune article does not suggest a clash of cultures. There is no psychiatric hospital culture that I am aware of where there is confusion about whether or not a patient should be allowed to injure themselves. The second problem is that this hospital needs psychiatrists who are trained to treat severe mental illness and aggression. They do not need to be forensic psychiatrists, but they do need expertise in treatment of severe mental illness. Forensic psychiatrists are basically needed to perform specific evaluations of criminal responsibility but the priority here is described as patient and staff safety. The people needed in this situation currently work in a number of acute care and community settings. They are very comfortable with the treatment of major psychiatric disorders and the associated medical comorbidity. It is safe to say that they enjoy working with these problems and talking with the people who have them. They are also sensitive to the needs of their co-workers and can establish the necessary environment of mutual trust and neutrality needed to succeed.
There may not be anyone around who remembers that Minnesota has solved a similar problem in the past. The year was 1990 and there were significant problems staffing the major state hospital in the system - Anoka Metro Regional Treatment Center. At that time, a Medical Director who was recently out of training was hired and he hired several colleagues from the same generation. They were all enthusiastic and interested in providing quality care. The state offered them competitive salaries. Within a very short period of time a cohesive staff developed and they became a favored training site for medical students. Treatment at the state hospital improved dramatically and several of the psychiatrists in that cohort went on to become leaders in the state in the provision of psychiatric services to patients with severe mental illness.
That still seems like a good idea today.
George Dawson, MD, DFAPA
Paul Mcenroe. Minnesota Security Hospital: Staff In Crisis Spreads Turmoil. StarTribune, December 27, 2013.
Office of the Legislative Auditor. Evaluation Report: State-Operated Human Services. February 2013.
Additional Clinical Note 1: Looking back over my post it is clear that I do not answer the question that is the title. Like most people I am speculating based on an imperfect data set. The main difference is that I am also speculating as an expert based on what needs to happen to provide the safest scientifically based treatment for people who are mentally ill, aggressive, and may have failed most if not all of the available treatments. I also recall that some past state hospital problems were resolved that has not been brought up in the discussion so far.
The Real Conflicts of Interest in Medicine and Psychiatry Today
I noticed some confusion around the GSK article that was recently posted. I decided to start the New Year examining conflicts of interest (COI) in medicine and psychiatry because they are widespread. These COI are much more widespread than the press or politicians have stated. That is because there are more players than physicians involved and these other players are hardly ever mentioned. You would never realize that by reading the papers largely because COI is always described as a problem with physicians. Nothing could be further from the truth.
My goal is to outline as many as possible and hopefully readers here will be able to fill in any that I might have missed. Because I am just one guy working in his spare time, it will not be an encyclopedic listing but it will be more comprehensive than you will find anywhere in the press or possibly the existing medical literature. It will also be more comprehensive than the typical political analysis that usually suggests that the only relevant conflicts of interest have to do with physicians making money or prescribing drugs in exchange for certain rewards. As you will see, these may be some of the least important conflicts of interest.
A good starting point is this diagram I made that looks at all of the important conflicts of interest that impinge on physicians. The diagram is not exhaustive. (click to enlarge)
Not all of the links are drawn and there are many smaller entities involved that have not been graphed. As you can see I have 13 major areas here that directly impact on physicians. It is important to keep in mind the main goal or interest is the practice of medicine. It flows from an ethical relationship with a physician. That relationship is defined as the physician acting toward the patient in a way that is only in the best interest of the patient in exchange for a professional fee. The modern relationship makes an important distinction in that the physician needs to be practicing scientific medicine. The American Psychiatric Association (APA) has a policy statement with some useful definitions. The APA defines the primary interest as "the highest level of evidence based practice, ethically based and scientifically valid research, and quality continuing education for the benefit of patients, the profession and society." They define secondary or personal interests such as personal, financial, or professional that: "may inhibit, distract, or unduly influence their (physicians) judgment or behavior in a manner that detracts from or subordinates the primary interest of patients and may be perceived by some as undermining public trust." Six examples of situations that may require vigilance to prevent conflict of interest issues are given and 5 of 6 can be seen as derivative of physician relationships with the pharmaceutical industry.
The Institute of Medicine (IOM) definition of conflict of interest is: "a set of circumstances that creates a risk that professional judgment or actions regarding a primary interest will be unduly influenced by a secondary interest." Note that the IOM makes no distinction about conflict of interest versus the appearance of conflict of interest. It turns out that the appearance of conflict of interest is the common standard that is used to indict the medical profession. The classic example that is typically given in the media is the influence of pharmaceutical representatives on physician prescribing behavior. The recent GSK disclosure confirms that that pharmaceutical representatives were paid based on the number of product prescriptions that the physicians they visited actually wrote. The idea is that promotional items of widely variable value (pens to pizza to golf outings to trips) and free samples led to increased prescriptions. Free samples provided to clinics was probably also a major factor and became a mainstay for many patients with limited or no mental health benefits. Typical press coverage suggests that the results of this type of conflict of interest are widespread and certain, but I would suggest that the great majority of physicians including many of those who were paid consultants by the pharmaceutical industry were not laboring under any conflict of interest.
Consider for a moment the conflicts of interest (COI) listed across the top of the diagram starting on the left with Managed Care COI. I have reviewed those conflicts of interest in great detail in previous posts. As an example consider the conflicts of interest in this post on how physician employees are managed by managed care companies. In all cases, there is a direct conflict of interest between physicians interest and the interest of the company and its managers. In every situation that I am aware of the physicians lose. That is typically viewed as a plus by the business managers running the company because it allows them to do whatever they want to do in terms of closing clinics and programs, firing physicians, firing support staff, coming up with business based performance metrics that are divorced from clinical reality, and denying care when they want to. When the conflict is framed as entitled doctors being managed for the first time in order to be fiscally responsible - apart from the obvious rhetoric the real impact on patients is lost. That has included the rationing of psychiatric services, the destruction of inpatient psychiatry services, the elimination of psychotherapy services, and the wholesale shifting of care for people with the severest forms of mental illness to deficient state operated services and correctional facilities.
Managed Care COI is almost always transacted by an army of intermediaries. There are so-called physician reviewers or utilization reviewers who look at records from a distance and second guess physicians actually treating the patient. They can say that they don't think a patient needs a particular service such as hospitalization and the patient is invariably discharged. These days many hospitals owned by managed care companies employ non-physician case managers who function the same as utilization reviewers and tell physicians when to discharge patients from the hospital. This review process represents what I consider to be the largest conflict of interest affecting the decision making process in medicine and it is the least transparent. You are not likely to hear about it until you or a family member are hospitalized and you are told that it is "time to go" based on an insurance company decision. You can see from the diagram that this COI is enmeshed with federal and state governments, think tanks, and some of the other managed care rationing tactics - Pharmaceutical Benefit Manager COI and Insurance Company COI. All of these bureaucracies can produce insurmountable obstacles to physicians trying to care for patients by denying diagnostic and treatment modalities and denying appropriate settings for care.
Staying on the Managed Care COI for a moment what do some of the other relationships imply? A full description of those relationships would require several books to explain. This all started about 30 years ago as a concerted anti-physician movement. Several political forces had an interest in making the argument that the reason for the high cost of American medicine was that physicians were greedy and they did too many procedures. The federal government set up a complex subjective billing and coding system to slow down physicians. It was a mechanism that could be used to investigate and prosecute anyone who seemed to be billing too much. They initially enforced these totally subjective rules with the FBI. At some point in the late 1990s, they allowed managed care organizations to internalize this process and control over physicians using this mechanism was handed off to managed care. Today it allows a managed care companies to look at the documentation of patient care, decide that the notes don't meet criteria for a certain bill, and retrospectively demand payment for reimbursed services based on the number of other people seen for that problem. The relationship between managed care companies and governments allows them to reimburse whatever they want for a service and demand back as much as they want. No other professionals have private industry and governments stacked against them in this manner. It is a motivating force for psychiatrists to not accept government backed insurance at a higher rate than other physicians.
Managed Care COI also means that it is practically impossible for a physician to appeal a decision by a managed care company. The appeal is to another doctor who is employed by that company. Any attempt to go outside of the company to a state insurance board is usually not productive. State insurance boards are after all generally run by political appointees who are insurance industry insiders. There are no neutral parties who are free of conflict of interest who can decide an appeal of an insurance company decision.
Practically all of the major entities represented on this chart operate in a similar manner to the managed care and insurance company conflicts of interest. They are business entities who have woven themselves deeply into the political system at all levels and they can generally do what they want to do in terms of running the US Health Care system. In most cases they treat physicians with impunity and tolerate professional groups only so far as they can co-opt some of their ideas and make it seem like they have an interest in quality care. They have also used their influence to introduce cost-effectiveness rhetoric into places where it makes no sense. That is especially true for psychiatric services where many have simply been shut down because they were not "cost-effective" enough.
Some of the other entities on the diagram are more subtle. Journalistic COI has a few sources. Certainly journalists have no interest in patient care or treatment standards. They do have an interest in selling stories and in some cases books. They have an interest in influencing people. Many of the stories I have commented on this blog over the past year were clearly rhetorical. Many were also the product of ignorance. Psychiatry is the only field in medicine, where non-experts don't hesitate to put their opinion in the New York Times and the New York Times doesn't hesitate to print it. One of the most read posts on this blog in the past year was about a Washington Post article that I critiqued for many of these reasons.
Professional Organization COI is also an interesting one. Consider the APA represents roughly 40,000 psychiatrists but only about 40% are actual members. When the American Board of Medical Specialties decided that they would introduce a new and onerous procedure to certify physicians in an ongoing manner instead of for life, the APA clearly sided with the ABMS despite widespread dissatisfaction by the membership. The conflict of interest considerations here are considerable and heavily financial. There is no scientific evidence that the proposed ABMS recertification process is a valid approach. There is certainly no evidence that a less onerous approach that would be less stressful to physicians would not achieve the goal of ongoing professional education and public safety.
The next time you read a story in the press about wealthy physicians being paid off to prescribe unnecessary medications or to perform unnecessary surgeries, pull up the COI diagram and print it out. The truth is that physicians are caught in a web of conflict of interest. Those conflicts of interest are generally set up to ration services to patients; ration or deny reimbursement to physicians; maximize the profits of middlemen (MCOs, HMOs, PBMs, Insurance companies); make politicians, think tanks, journalists and critics look good; and distribute a large chunk of the health care dollar to people who are not involved in providing the services. The impact is the greatest by far in the area of psychiatric services but at some level it affects all of medicine. The impact on physicians is also significant. All of the pressures on physicians as a result of these conflicts of interest widen dissatisfaction with the field and increase burnout. Both of those factors can potentially impact physician availability and intellectual resources necessary for optimal performance. So if your physician looks burned out - he or she may well be. It is probably directly related to doing an additional 2 or 3 hours of work every day to satisfy the requirements of all of these extraneous conflicts of interest. Of course that is all generally unreimbursed time. How would most workers react to putting in a full day and then an additional 2 - 3 hours off the clock to satisfy the requirements of some outside company? It is like working for free for another company.
That is the real cost of conflict of interest and one of the reasons that health care premiums are essentially another tax on all Americans.
Happy New Year!
George Dawson, MD, DFAPA
Institute of Medicine (US) Committee on Conflict of Interest in Medical Research, Education, and Practice; Lo B, Field MJ, editors. Conflict of Interest in Medical Research, Education, and Practice. Washington (DC): National Academies Press (US); 2009. Available from: http://www.ncbi.nlm.nih.gov/books/NBK22942/
My goal is to outline as many as possible and hopefully readers here will be able to fill in any that I might have missed. Because I am just one guy working in his spare time, it will not be an encyclopedic listing but it will be more comprehensive than you will find anywhere in the press or possibly the existing medical literature. It will also be more comprehensive than the typical political analysis that usually suggests that the only relevant conflicts of interest have to do with physicians making money or prescribing drugs in exchange for certain rewards. As you will see, these may be some of the least important conflicts of interest.
A good starting point is this diagram I made that looks at all of the important conflicts of interest that impinge on physicians. The diagram is not exhaustive. (click to enlarge)
Not all of the links are drawn and there are many smaller entities involved that have not been graphed. As you can see I have 13 major areas here that directly impact on physicians. It is important to keep in mind the main goal or interest is the practice of medicine. It flows from an ethical relationship with a physician. That relationship is defined as the physician acting toward the patient in a way that is only in the best interest of the patient in exchange for a professional fee. The modern relationship makes an important distinction in that the physician needs to be practicing scientific medicine. The American Psychiatric Association (APA) has a policy statement with some useful definitions. The APA defines the primary interest as "the highest level of evidence based practice, ethically based and scientifically valid research, and quality continuing education for the benefit of patients, the profession and society." They define secondary or personal interests such as personal, financial, or professional that: "may inhibit, distract, or unduly influence their (physicians) judgment or behavior in a manner that detracts from or subordinates the primary interest of patients and may be perceived by some as undermining public trust." Six examples of situations that may require vigilance to prevent conflict of interest issues are given and 5 of 6 can be seen as derivative of physician relationships with the pharmaceutical industry.
The Institute of Medicine (IOM) definition of conflict of interest is: "a set of circumstances that creates a risk that professional judgment or actions regarding a primary interest will be unduly influenced by a secondary interest." Note that the IOM makes no distinction about conflict of interest versus the appearance of conflict of interest. It turns out that the appearance of conflict of interest is the common standard that is used to indict the medical profession. The classic example that is typically given in the media is the influence of pharmaceutical representatives on physician prescribing behavior. The recent GSK disclosure confirms that that pharmaceutical representatives were paid based on the number of product prescriptions that the physicians they visited actually wrote. The idea is that promotional items of widely variable value (pens to pizza to golf outings to trips) and free samples led to increased prescriptions. Free samples provided to clinics was probably also a major factor and became a mainstay for many patients with limited or no mental health benefits. Typical press coverage suggests that the results of this type of conflict of interest are widespread and certain, but I would suggest that the great majority of physicians including many of those who were paid consultants by the pharmaceutical industry were not laboring under any conflict of interest.
Consider for a moment the conflicts of interest (COI) listed across the top of the diagram starting on the left with Managed Care COI. I have reviewed those conflicts of interest in great detail in previous posts. As an example consider the conflicts of interest in this post on how physician employees are managed by managed care companies. In all cases, there is a direct conflict of interest between physicians interest and the interest of the company and its managers. In every situation that I am aware of the physicians lose. That is typically viewed as a plus by the business managers running the company because it allows them to do whatever they want to do in terms of closing clinics and programs, firing physicians, firing support staff, coming up with business based performance metrics that are divorced from clinical reality, and denying care when they want to. When the conflict is framed as entitled doctors being managed for the first time in order to be fiscally responsible - apart from the obvious rhetoric the real impact on patients is lost. That has included the rationing of psychiatric services, the destruction of inpatient psychiatry services, the elimination of psychotherapy services, and the wholesale shifting of care for people with the severest forms of mental illness to deficient state operated services and correctional facilities.
Managed Care COI is almost always transacted by an army of intermediaries. There are so-called physician reviewers or utilization reviewers who look at records from a distance and second guess physicians actually treating the patient. They can say that they don't think a patient needs a particular service such as hospitalization and the patient is invariably discharged. These days many hospitals owned by managed care companies employ non-physician case managers who function the same as utilization reviewers and tell physicians when to discharge patients from the hospital. This review process represents what I consider to be the largest conflict of interest affecting the decision making process in medicine and it is the least transparent. You are not likely to hear about it until you or a family member are hospitalized and you are told that it is "time to go" based on an insurance company decision. You can see from the diagram that this COI is enmeshed with federal and state governments, think tanks, and some of the other managed care rationing tactics - Pharmaceutical Benefit Manager COI and Insurance Company COI. All of these bureaucracies can produce insurmountable obstacles to physicians trying to care for patients by denying diagnostic and treatment modalities and denying appropriate settings for care.
Staying on the Managed Care COI for a moment what do some of the other relationships imply? A full description of those relationships would require several books to explain. This all started about 30 years ago as a concerted anti-physician movement. Several political forces had an interest in making the argument that the reason for the high cost of American medicine was that physicians were greedy and they did too many procedures. The federal government set up a complex subjective billing and coding system to slow down physicians. It was a mechanism that could be used to investigate and prosecute anyone who seemed to be billing too much. They initially enforced these totally subjective rules with the FBI. At some point in the late 1990s, they allowed managed care organizations to internalize this process and control over physicians using this mechanism was handed off to managed care. Today it allows a managed care companies to look at the documentation of patient care, decide that the notes don't meet criteria for a certain bill, and retrospectively demand payment for reimbursed services based on the number of other people seen for that problem. The relationship between managed care companies and governments allows them to reimburse whatever they want for a service and demand back as much as they want. No other professionals have private industry and governments stacked against them in this manner. It is a motivating force for psychiatrists to not accept government backed insurance at a higher rate than other physicians.
Managed Care COI also means that it is practically impossible for a physician to appeal a decision by a managed care company. The appeal is to another doctor who is employed by that company. Any attempt to go outside of the company to a state insurance board is usually not productive. State insurance boards are after all generally run by political appointees who are insurance industry insiders. There are no neutral parties who are free of conflict of interest who can decide an appeal of an insurance company decision.
Practically all of the major entities represented on this chart operate in a similar manner to the managed care and insurance company conflicts of interest. They are business entities who have woven themselves deeply into the political system at all levels and they can generally do what they want to do in terms of running the US Health Care system. In most cases they treat physicians with impunity and tolerate professional groups only so far as they can co-opt some of their ideas and make it seem like they have an interest in quality care. They have also used their influence to introduce cost-effectiveness rhetoric into places where it makes no sense. That is especially true for psychiatric services where many have simply been shut down because they were not "cost-effective" enough.
Some of the other entities on the diagram are more subtle. Journalistic COI has a few sources. Certainly journalists have no interest in patient care or treatment standards. They do have an interest in selling stories and in some cases books. They have an interest in influencing people. Many of the stories I have commented on this blog over the past year were clearly rhetorical. Many were also the product of ignorance. Psychiatry is the only field in medicine, where non-experts don't hesitate to put their opinion in the New York Times and the New York Times doesn't hesitate to print it. One of the most read posts on this blog in the past year was about a Washington Post article that I critiqued for many of these reasons.
Professional Organization COI is also an interesting one. Consider the APA represents roughly 40,000 psychiatrists but only about 40% are actual members. When the American Board of Medical Specialties decided that they would introduce a new and onerous procedure to certify physicians in an ongoing manner instead of for life, the APA clearly sided with the ABMS despite widespread dissatisfaction by the membership. The conflict of interest considerations here are considerable and heavily financial. There is no scientific evidence that the proposed ABMS recertification process is a valid approach. There is certainly no evidence that a less onerous approach that would be less stressful to physicians would not achieve the goal of ongoing professional education and public safety.
The next time you read a story in the press about wealthy physicians being paid off to prescribe unnecessary medications or to perform unnecessary surgeries, pull up the COI diagram and print it out. The truth is that physicians are caught in a web of conflict of interest. Those conflicts of interest are generally set up to ration services to patients; ration or deny reimbursement to physicians; maximize the profits of middlemen (MCOs, HMOs, PBMs, Insurance companies); make politicians, think tanks, journalists and critics look good; and distribute a large chunk of the health care dollar to people who are not involved in providing the services. The impact is the greatest by far in the area of psychiatric services but at some level it affects all of medicine. The impact on physicians is also significant. All of the pressures on physicians as a result of these conflicts of interest widen dissatisfaction with the field and increase burnout. Both of those factors can potentially impact physician availability and intellectual resources necessary for optimal performance. So if your physician looks burned out - he or she may well be. It is probably directly related to doing an additional 2 or 3 hours of work every day to satisfy the requirements of all of these extraneous conflicts of interest. Of course that is all generally unreimbursed time. How would most workers react to putting in a full day and then an additional 2 - 3 hours off the clock to satisfy the requirements of some outside company? It is like working for free for another company.
That is the real cost of conflict of interest and one of the reasons that health care premiums are essentially another tax on all Americans.
Happy New Year!
George Dawson, MD, DFAPA
Institute of Medicine (US) Committee on Conflict of Interest in Medical Research, Education, and Practice; Lo B, Field MJ, editors. Conflict of Interest in Medical Research, Education, and Practice. Washington (DC): National Academies Press (US); 2009. Available from: http://www.ncbi.nlm.nih.gov/books/NBK22942/
Thursday, December 26, 2013
Pills Don't Save Lives - Psychiatrists Do
I am paraphrasing David Healy from a previous post and I am doing it here to emphasize - it's all about the side effects. Healy's comment serves as a counterpoint to a highly successful multi-decade advertising campaign by pharmaceutical companies. It began with the first National Depression Screening Day in 1991. The emphasis was on identifying and treating depression with antidepressants. There was no real discussion of antidepressant side effects or the general problem of side effects with most medications. Since then antidepressant treatment has been conceptualized as comprehensive treatment wrapped up in a pill or capsule. That bias continues today as various political forces have shifted depression screening from an annual event to primary care clinics. Some health care organizations and states consider depression screening and serial ratings of depression to be quality markers of health care services despite the fact that there are definite problems with that idea. Unless there is a highly specific screening test any screening procedure has the potential to expose more people to the side effects of treatment. There is no highly specific screening test for depression.
A second factor in considering side effects is the physician's role. Doctors are trained to identify and treat conditions with surgery or medications. Psychiatrists have additional training in psychotherapy. When you are in your training, the emphasis in on making the correct diagnosis and selecting the medication that will be the most useful. Even though medical training is long, the longest you might follow any patient might be for a couple of years. In medical practice you have the ability to see people for decades rather than months or years and how their medical treatment changes over those years. You also observe first hand the long term toxicity of many medications when you might have only been exposed to that on a theoretical basis during training. As a practicing physician you are expected to help people deal with the fact that they have side effects and the medications they are using may not be that useful. In fact, in many cases they may not be beneficial or may be causing more harm than good.
All of that experience with side effects leads clinicians to develop new practices that they were never trained to do. Very early in my career, I had the experience of treating a person who had been on an antidepressant for about 6 years. She had headaches and depression and like many people with chronic depression she was in a stressful situation that she could not remove herself from. She had chronic depression in the context of a chronic stressor that was not going away. At some point her headaches resolved and her depression improved. We decided to taper her off the antidepressant. She came in 2 weeks later and said: "I feel much better. All of the years that I was taking that medication I didn't realize it, but I felt like I had the flu. That has now cleared up." That early experience led me to modify the ways that I discuss medications with people.
I generally tell people that I don't expect anyone to "get used to" a medication. I often tell them that people may get used to feeling ill rather than develop a tolerance to medication side effects. I tell them that if they are experiencing any side effects at all to let me know about it and we will decide what to do about it at that time. I let them know the range of experiences with medications and what they might expect. As an example, I might say that "60-80% of people might take this medication and not notice that they are taking anything, but 5-10% of people might not tolerate it at all." I let them know about all of the FDA contraindications, in some cases I review it with them many times. I discuss the common side effects and usually provide them with the MedlinePlus handout on the medication. I think it is more comprehensive than most handouts and it gives the FDA black box warnings (in a red box) on the front of every handout. I talk with them about rare but potentially serious side effects like drug induced liver disease and arrhythmias and what to look for. In the case of atypical antipsychotics, I discuss movement disorders and metabolic effects. I demonstrate what the movements of tardive dyskinesia may look like. I let people know if the medications they are taking are potentially addictive. I the case of lithium, I let people know about the unique toxicities and the safest possible way they can take it. In the case of antidepressants, I let people know that they may be difficult to stop due to discontinuation symptoms.
My side effect discussions with people have taught me valuable lessons. There are people who are placebo responders and nocebo responders. The nocebo responders develop problems taking any medication, even medications that are generally well tolerated at low doses. Some of them are aware of the problem and decline any discussion of side effects. They might say they don't want the MedlinePlus handout because: "If I read about any side effects I will probably get them." They would rather be surprised. Whenever I encounter that attitude, I respect their wishes but advise them to contact me if they have any side effects. I also recall my Forensic Psychiatry lectures during residency. The instructor advised us that we "could be sued" if our side effect discussions prevented a patient from taking a useful medication and there was an adverse outcome as a result. I have realized over the years that basing your decisions on whether you could be sued is generally a bad idea because you can be sued for just about anything. I think that people need to hear about what really happens with psychiatric medications and consider myself to be a good source of information.
I have also found that there is a hearty group of people who decide on their own that they will try to tolerate side effects and not let me know about it despite our discussion. When I see them in the follow up appointment they will say: "Well you know doc, I had a pretty good headache the first three days on the medications, but I decided to keep taking it to see if it would go away and sure enough on day 4 the headache was gone." They tell me that even though I advised them to not tolerate side effects and to call me if they had any side effects. These patients are almost always men with a history of avoiding doctors and not taking care of themselves. I guess their experience confirms that some people develop a tolerance to side effects but why would you want to? I was at a large conference on the treatment of anxiety disorders and listened to a renowned psychopharmacologist talk about his technique for treating anxiety disorders with SSRI and SNRI type antidepressants. His approach was to keep titrating the medication "to the point of toxicity" and then back off to the lower dose. My experience has taught me that the best approach in non acute situations is to use the lowest possible dose. That is usually the dose recommended for anxiety disorders and titrate it to the exact point where the symptoms are in remission. I am never compelled to increase a medication by a multiple based on the pill size or a drug level based on the aggregate experience of a cohort of people in a drug trial.
I obsess about the hypothetical. Physicians in practice are aware of trends in the medications that are prescribed and psychiatry is no exception. Drug interactions have been an area of focus in psychiatry since it was first learned that fluoxetine could inhibit the hepatic metabolism of tricyclic antidepressants and that could lead to antidepressant toxicity. I treat people who are often on a mind boggling combination of medications for their chronic illnesses and psychiatric disorders. I routinely run those lists through one or more computerized drug interaction software packages. The software is inconsistent and I often have to look up the case report or study that suggest a specific interaction or problem. I have to make the decision to accept or reject what the software is telling me. The QTc interval or the interval on the electrocardiogram that corresponds with the total time of ventricular contraction and relaxation has been a major concern since the approval of ziprasidone. It has been complicated lately by the FDA concern that citalopram may prolong the QTc interval in some people to a significant extent. I screen people with electrocardiograms if it appears that their clinical status or total medication burden may lead to prolongation of the QTc interval.
In some cases a concern for the hypothetical requires some inductive reasoning. Current textbooks, literature, and standard prescribing references create the illusion at times that everything is known about a medication, it is just a matter of finding it. There are plenty of examples where that is not true or where there is a lot of uncertainty about when a medication can be safely and effectively prescribed. To illustrate, consider a hypothetical situation of patient with bipolar disorder who may benefit from taking lithium. For a time during my residency training the renal toxicity of lithium was openly debated. Nephrologists at the time certainly believed it was nephrotoxic but there were large series of patients who were described with minimal signs of renal toxicity. Clinical practice treating patients with severe bipolar disorder has lead me into situations where I have treated patients on, during and after dialysis and kidney transplantation. The estimation of glomerular filtration rate (GFR) by 24 hour urine collections was also problematic. That has been greatly improved by the practice of using calculated GFRs. I have no doubt at all that taking lithium for a period of time can lead to renal failure in a portion of patients taking it. Anyone prescribing lithium needs to be aware of this fact and take all measures necessary to minimize episodes of lithium toxicity and exposure to other nephrotoxins. In some cases like NSAIDs, the toxins are well known. In other cases like tenofovir, the interactions are not known and in fact you can scan an entire FDA approved package insert and might find no references to lithium. Making that decision may take hours or a weekend of study to figure out the best course of action.
I hope that I have made the case for psychiatric medications needing a careful analysis of side effects before they can be initiated and continued. The decision to take medications is a serious one. In 29 years of practice I have not met a single person who told me that they liked to take medications. The decision to take medications often comes down to having tried everything else and realizing that a major change is necessary to get back to where you want to be. A recent reply to my previous blog post described medications as "tools" rather than a panacea and I think that until perfectly safe and effective medications are invented that is true. Healy's point is that the advertising notion of "Take an antidepressant and get better" is false. Psychiatrists are trained to help you navigate the complicated process of recovery from depression and side effects and the potential for side effects is generally the most complicated aspect.
George Dawson, MD, DFAPA
Additional Clinical Note 1: Another blogger sent me an e-mail earlier this week asking me to send a list of psychiatrists who I thought were competent to taper people off of SSRI/SNRI type antidepressants. The intention of the e-mail was to have a ready list of people who could help people with that particular problem. I think that all psychiatric residents should be taught about medication discontinuation effects and how to resolve them, but apparently that is not the experience of some people who end up taking these medications. As an instructor in a psychopharmacology course, I can verify that the residents I taught were all aware of this problem and how to deal with it. They also had the very good back up reference of the ASCP psychopharmacology course PowerPoints and lecture materials on this problem. I realize that this blog is not widely read, but I would appreciate any posts from instructors or professors about the issue of side effect recognition and treatment in general and SSRI discontinuation symptoms in particular and the approach to teaching these topics in your program. I would also appreciate hearing your thoughts on this problem about SSRI/SNRI discontinuation symptoms and the variable experiences of people trying to get the problem diagnosed and treated.
Additional Clinical Note 2: The processes that I am describing in the above post take time. In many cases the equivalent amount of time required to do psychotherapy and longer. I do have people telling me that their physicians (all types) seem to be poised over a prescription pad. They tell me nobody has ever informed them of the risks or potential side effects of a medication. I don't think the problem has been investigated and it would be difficult to do. The idea that "medication management" in psychiatry, internal medicine or any other field is a brief uncomplicated encounter that takes little thinking on the part of a physician is largely an invention of business interests seeking to reimburse physicians at the lowest possible rate. If you are a consumer of medical services, consider my approach in the above post and ask yourself if you have had the discussions that I describe.
A second factor in considering side effects is the physician's role. Doctors are trained to identify and treat conditions with surgery or medications. Psychiatrists have additional training in psychotherapy. When you are in your training, the emphasis in on making the correct diagnosis and selecting the medication that will be the most useful. Even though medical training is long, the longest you might follow any patient might be for a couple of years. In medical practice you have the ability to see people for decades rather than months or years and how their medical treatment changes over those years. You also observe first hand the long term toxicity of many medications when you might have only been exposed to that on a theoretical basis during training. As a practicing physician you are expected to help people deal with the fact that they have side effects and the medications they are using may not be that useful. In fact, in many cases they may not be beneficial or may be causing more harm than good.
All of that experience with side effects leads clinicians to develop new practices that they were never trained to do. Very early in my career, I had the experience of treating a person who had been on an antidepressant for about 6 years. She had headaches and depression and like many people with chronic depression she was in a stressful situation that she could not remove herself from. She had chronic depression in the context of a chronic stressor that was not going away. At some point her headaches resolved and her depression improved. We decided to taper her off the antidepressant. She came in 2 weeks later and said: "I feel much better. All of the years that I was taking that medication I didn't realize it, but I felt like I had the flu. That has now cleared up." That early experience led me to modify the ways that I discuss medications with people.
I generally tell people that I don't expect anyone to "get used to" a medication. I often tell them that people may get used to feeling ill rather than develop a tolerance to medication side effects. I tell them that if they are experiencing any side effects at all to let me know about it and we will decide what to do about it at that time. I let them know the range of experiences with medications and what they might expect. As an example, I might say that "60-80% of people might take this medication and not notice that they are taking anything, but 5-10% of people might not tolerate it at all." I let them know about all of the FDA contraindications, in some cases I review it with them many times. I discuss the common side effects and usually provide them with the MedlinePlus handout on the medication. I think it is more comprehensive than most handouts and it gives the FDA black box warnings (in a red box) on the front of every handout. I talk with them about rare but potentially serious side effects like drug induced liver disease and arrhythmias and what to look for. In the case of atypical antipsychotics, I discuss movement disorders and metabolic effects. I demonstrate what the movements of tardive dyskinesia may look like. I let people know if the medications they are taking are potentially addictive. I the case of lithium, I let people know about the unique toxicities and the safest possible way they can take it. In the case of antidepressants, I let people know that they may be difficult to stop due to discontinuation symptoms.
My side effect discussions with people have taught me valuable lessons. There are people who are placebo responders and nocebo responders. The nocebo responders develop problems taking any medication, even medications that are generally well tolerated at low doses. Some of them are aware of the problem and decline any discussion of side effects. They might say they don't want the MedlinePlus handout because: "If I read about any side effects I will probably get them." They would rather be surprised. Whenever I encounter that attitude, I respect their wishes but advise them to contact me if they have any side effects. I also recall my Forensic Psychiatry lectures during residency. The instructor advised us that we "could be sued" if our side effect discussions prevented a patient from taking a useful medication and there was an adverse outcome as a result. I have realized over the years that basing your decisions on whether you could be sued is generally a bad idea because you can be sued for just about anything. I think that people need to hear about what really happens with psychiatric medications and consider myself to be a good source of information.
I have also found that there is a hearty group of people who decide on their own that they will try to tolerate side effects and not let me know about it despite our discussion. When I see them in the follow up appointment they will say: "Well you know doc, I had a pretty good headache the first three days on the medications, but I decided to keep taking it to see if it would go away and sure enough on day 4 the headache was gone." They tell me that even though I advised them to not tolerate side effects and to call me if they had any side effects. These patients are almost always men with a history of avoiding doctors and not taking care of themselves. I guess their experience confirms that some people develop a tolerance to side effects but why would you want to? I was at a large conference on the treatment of anxiety disorders and listened to a renowned psychopharmacologist talk about his technique for treating anxiety disorders with SSRI and SNRI type antidepressants. His approach was to keep titrating the medication "to the point of toxicity" and then back off to the lower dose. My experience has taught me that the best approach in non acute situations is to use the lowest possible dose. That is usually the dose recommended for anxiety disorders and titrate it to the exact point where the symptoms are in remission. I am never compelled to increase a medication by a multiple based on the pill size or a drug level based on the aggregate experience of a cohort of people in a drug trial.
I obsess about the hypothetical. Physicians in practice are aware of trends in the medications that are prescribed and psychiatry is no exception. Drug interactions have been an area of focus in psychiatry since it was first learned that fluoxetine could inhibit the hepatic metabolism of tricyclic antidepressants and that could lead to antidepressant toxicity. I treat people who are often on a mind boggling combination of medications for their chronic illnesses and psychiatric disorders. I routinely run those lists through one or more computerized drug interaction software packages. The software is inconsistent and I often have to look up the case report or study that suggest a specific interaction or problem. I have to make the decision to accept or reject what the software is telling me. The QTc interval or the interval on the electrocardiogram that corresponds with the total time of ventricular contraction and relaxation has been a major concern since the approval of ziprasidone. It has been complicated lately by the FDA concern that citalopram may prolong the QTc interval in some people to a significant extent. I screen people with electrocardiograms if it appears that their clinical status or total medication burden may lead to prolongation of the QTc interval.
In some cases a concern for the hypothetical requires some inductive reasoning. Current textbooks, literature, and standard prescribing references create the illusion at times that everything is known about a medication, it is just a matter of finding it. There are plenty of examples where that is not true or where there is a lot of uncertainty about when a medication can be safely and effectively prescribed. To illustrate, consider a hypothetical situation of patient with bipolar disorder who may benefit from taking lithium. For a time during my residency training the renal toxicity of lithium was openly debated. Nephrologists at the time certainly believed it was nephrotoxic but there were large series of patients who were described with minimal signs of renal toxicity. Clinical practice treating patients with severe bipolar disorder has lead me into situations where I have treated patients on, during and after dialysis and kidney transplantation. The estimation of glomerular filtration rate (GFR) by 24 hour urine collections was also problematic. That has been greatly improved by the practice of using calculated GFRs. I have no doubt at all that taking lithium for a period of time can lead to renal failure in a portion of patients taking it. Anyone prescribing lithium needs to be aware of this fact and take all measures necessary to minimize episodes of lithium toxicity and exposure to other nephrotoxins. In some cases like NSAIDs, the toxins are well known. In other cases like tenofovir, the interactions are not known and in fact you can scan an entire FDA approved package insert and might find no references to lithium. Making that decision may take hours or a weekend of study to figure out the best course of action.
I hope that I have made the case for psychiatric medications needing a careful analysis of side effects before they can be initiated and continued. The decision to take medications is a serious one. In 29 years of practice I have not met a single person who told me that they liked to take medications. The decision to take medications often comes down to having tried everything else and realizing that a major change is necessary to get back to where you want to be. A recent reply to my previous blog post described medications as "tools" rather than a panacea and I think that until perfectly safe and effective medications are invented that is true. Healy's point is that the advertising notion of "Take an antidepressant and get better" is false. Psychiatrists are trained to help you navigate the complicated process of recovery from depression and side effects and the potential for side effects is generally the most complicated aspect.
George Dawson, MD, DFAPA
Additional Clinical Note 1: Another blogger sent me an e-mail earlier this week asking me to send a list of psychiatrists who I thought were competent to taper people off of SSRI/SNRI type antidepressants. The intention of the e-mail was to have a ready list of people who could help people with that particular problem. I think that all psychiatric residents should be taught about medication discontinuation effects and how to resolve them, but apparently that is not the experience of some people who end up taking these medications. As an instructor in a psychopharmacology course, I can verify that the residents I taught were all aware of this problem and how to deal with it. They also had the very good back up reference of the ASCP psychopharmacology course PowerPoints and lecture materials on this problem. I realize that this blog is not widely read, but I would appreciate any posts from instructors or professors about the issue of side effect recognition and treatment in general and SSRI discontinuation symptoms in particular and the approach to teaching these topics in your program. I would also appreciate hearing your thoughts on this problem about SSRI/SNRI discontinuation symptoms and the variable experiences of people trying to get the problem diagnosed and treated.
Additional Clinical Note 2: The processes that I am describing in the above post take time. In many cases the equivalent amount of time required to do psychotherapy and longer. I do have people telling me that their physicians (all types) seem to be poised over a prescription pad. They tell me nobody has ever informed them of the risks or potential side effects of a medication. I don't think the problem has been investigated and it would be difficult to do. The idea that "medication management" in psychiatry, internal medicine or any other field is a brief uncomplicated encounter that takes little thinking on the part of a physician is largely an invention of business interests seeking to reimburse physicians at the lowest possible rate. If you are a consumer of medical services, consider my approach in the above post and ask yourself if you have had the discussions that I describe.
Saturday, December 21, 2013
GSK Eliminates Appearance of Conflict of Interest - Who Is Next?
Glaxo Smith Kline came out with a major announcement a few days ago. It will no longer pay doctors to promote its drugs and it will no longer tie the compensation of its sales force to the number of prescriptions written by doctors who have been detailed about those drugs. These are both standard practices in the pharmaceutical industry and this is the first announcement of its kind within the industry. GSK will continue to to provide "unsolicited independent educational grants" to educational institutions or medical societies. Pharmaceutical reps will be paid on the basis of technical knowledge and customer service rather than sales. GSK has been fined heavily lately about promoting off label use of its products and is currently under investigation in China.
My immediate reaction to the piece was "good riddance". For the past decade there has been no bigger issue in psychiatry than the appearance of conflict of interest with the pharmaceutical industry. Psychiatry has been targeted more than any other medical specialty by prominent politicians, the news media, and even by psychiatrists themselves. There are endless blogs and opinion pieces about how the practice of psychiatry has been defined by this appearance of conflict of interest. There are several blogs out there that have gained prominence by endlessly reviewing all of these details. It has affected the way the APA does business. It has affected the way local district branches do business. In the end the politicians are grandstanding on it, because the PPACA (Obamacare) will apparently list any physician receiving money from a pharmaceutical company. That was suggested as a motivating factor in the NY Times article. Those public lists have existed in some states like the one I have practiced in for years.
To me the arguments have always come down to advertising and ethics. From an advertising perspective would we expect people to be affected by product advertising? Of course we would. The buying habits of the American population are shaped by advertising. Selling products is more of a science than people think. The American public can easily change its buying habits and can purchase products that are unnecessary and will be discarded after a brief period of time. They can also be sold on products like junk food that are unhealthy but designed to be sold in large quantities. Advertising would not seem to be the ideal basis for marketing drugs to physicians, but with many new products physicians are now bypassed and the drug is sold directly to the consumer. If the epidemiology of a particular problem like "low-T" is known, direct-to-consumer marketing probably leads to many, many more physician visits than a physician suggesting to their patient that they probably have primary or hypogonadotropic hypogonadism. All a patient has to do is go to the web site and take a non-specific checklist quiz on the features of "low-T" and be in their doctor's office to get the levels done within a week. Things will probably go a lot smoother without a physician intermediary in the loop and I am sure that much physician behavior will be shaped by the onslaught of men coming in to be tested for "low-T". I know for a fact that psychiatrists are approached for this problem because of the overlap between the syndrome and depression.
Part of the advertising argument has always been that there are unconscious factors in play. Really? That is the basis for all advertising in general. The main difference has been that pharmaceutical representatives have been schooled on the relationship aspects of the sale. They have been taught that basically if a physician likes them or feels indebted to them for free food, trinkets like poor quality pens that never seem to write very well, a round of golf, or tickets to the Lakers game that they may be more likely to prescribe their product. Most physicians were apparently naive enough to not realize that there was a huge marketing database out there that tracked their prescription writing to see if they were writing the required number of prescriptions for that product. In the real heyday of marketing bonuses to physicians, companies would pay for travel to important meetings.
While the people focused on the advertising influence kept chipping away mostly at psychiatrists, they seemed to ignore two important developments that made detailing or selling to individual physicians much less relevant. The first was restricted formularies. I was on the Pharmacy and Therapeutics Committee (P&T) of one of the largest health plans in the state and an affiliated hospital for a total of 10 years. During that time, the predominant factor in the decision about whether to put a drug on a formulary that would make it available to prescribing physicians was the cost. There were very few instances where a drug was so unique that it was made available even if it was very expensive. In those cases a drug might be available for an incurable illness that had a negligible benefit but it was included basically for public relations. One of the other overriding themes of the P & T Committee was that all drugs in a particular class (like antidepressants) were equivalent and therefore the least expensive drug in the class could be substituted for anything else. This potentially led to a lot of unnecessary chaos when medications fell out of favor due to pricing and patients needed to be shifted en masse to the least expensive drug. It gave hospitals and health plans leverage in dealing with pharmaceutical companies, but in some cases the deals were complex. As an example, in order to get a new blockbuster drug at a good price, the health plan would need to accept the same company's generic in a different class that had been removed because it was considered too expensive. Over a decade ago, business entrepreneurs decided that there was money to be made rationing medications to health plan enrollees and now a lot of that is done by pharmaceutical benefit managers (PBMs). PBMs are currently a multibillion dollar industry.
The second important development was generic drugs. Practically all of the blockbuster psychiatric medications of the past two decades are now generic drugs. Many generic drugs are easily affordable even as direct out of pocket purchases. At that point they are no longer actively marketed by the pharmaceutical company that held the exclusive patents. They are more likely to be the preferred drugs of PBMs and health plan formularies. They are in that role because of a scientific approximation. That approximation is that all drugs in a certain class, like antidepressants that have the same purported mechanism of action are equivalent and one can be substituted for another. That is clearly false but it allows the health plan to to provide you with the least expensive medication or charge you a hefty copay for one that is not. It also seems to not consider after market information that can even affect generic drugs. The best example I can think of there is the FDA warnings on citalopram. I would guess that despite the warnings, it remains a preferred drug by most health plans. Health plans in general seem to be geared up to prescribe antidepressants at higher and higher rates. I would take it a step further and venture a guess that most health plans have not taken a look at the data in their systems on whether or not they have observed problems related to the FDA warning on citalopram.
The ethical argument goes something like this. Physicians should have the best interests of their patients in mind and an advertising based conflict-of-interest to prescribe a certain drug creates an ethical concern. On the face of it, it seems like a straightforward argument. But there are several problems with it. For example, what is the direct evidence that this occurs - if any? Is it really believable that a physician would prescribe a decidedly suboptimal medication to a patient based on schmoozing with a pharmaceutical representative? There are often other factors in play. It is common to treat people with chronic illnesses who have suboptimal response to the current therapy and who are looking for the "next biggest thing" to try. A physician who has been detailed on the "next biggest thing" is likely to prescribe it if asked. There is a similar dynamic with the issue of overprescribing in general. If a patient persists in their request for an opioid, an antibiotic, a stimulant or any other drug are they likely to get it? The recent declaration that the CDC initiative to decrease antibiotic prescribing has failed would suggest that they will. Finally there is the dynamic of "see the doctor and leave with a pill." There are any number of scenarios where medications are used in medical practice and other options are not even discussed. The psychiatric cases are highlighted but it happens as frequently in cases of mild diabetes mellitus, back pain, chronic pain of various causes, hypercholesterolemia, mild hypertension and others. Many people have described this as "the doctor was poised over his prescription pad" but the healthcare industry is set up to see people in brief medication focused visits and physician reimbursement is tied to it. There are also patient related factors and a recent Tom Hanks interview is illustrative. He was on a late night talk show discussing his recent diagnosis of diabetes mellitus and he said his physician told him that if he could get back to his high school body weight he probably would not have it. His reply was: "Well I'm going to have Type II diabetes."
The ethical arguments, especially the ones I have seen constructed by physicians also ignore the general case of conflicts of interest at the professional level. Practically every major university department allows its faculty to supplement their salaries by consulting in private industry. In many cases that is a major source of additional income. In some cases those professionals are involved in setting standards and their approach is much different than the wall that is currently being constructed between the medical profession and the pharmaceutical industry. As an example, academic and industry professionals within the engineering profession are often on committees responsible for setting standards that govern all of the products within that industry. Their approach is to include as many industry professionals as necessary rather than suggesting the academics can set the standards themselves. Considering that pharmaceutical companies employ some of the top scientists in the world it would seem that medicine has a lot to lose if it goes along with the prevailing assumption. The prevailing assumption is that physicians are powerless to stop prescribing expensive medications that are of questionable benefit for their patients based solely on advertising and no scientific merit.
I applaud the GSK decision even though the above cited factors would suggest that for most physicians it has only historical relevance. I would encourage all of Big Pharma to adopt the same policies toward physicians. But this doesn't really go far enough and it is basically a token gesture at this point. To really make a difference I would suggest that they stop giving money to politicians. GSK spent $1.9 million on candidates and $4.9 million in lobbying last year. All of that money was directed at a few politicians. It is a part of a massive industry wide contribution to politicians. What do you think buys more influence, giving free pizza and pens to doctors or giving thousands to tens of thousands of dollars to politicians?
George Dawson, MD, DFAPA
Katie Thomas. Glaxo Says It Will Stop Paying Doctors To Promote Drugs. New York Times December 16, 2013.
My immediate reaction to the piece was "good riddance". For the past decade there has been no bigger issue in psychiatry than the appearance of conflict of interest with the pharmaceutical industry. Psychiatry has been targeted more than any other medical specialty by prominent politicians, the news media, and even by psychiatrists themselves. There are endless blogs and opinion pieces about how the practice of psychiatry has been defined by this appearance of conflict of interest. There are several blogs out there that have gained prominence by endlessly reviewing all of these details. It has affected the way the APA does business. It has affected the way local district branches do business. In the end the politicians are grandstanding on it, because the PPACA (Obamacare) will apparently list any physician receiving money from a pharmaceutical company. That was suggested as a motivating factor in the NY Times article. Those public lists have existed in some states like the one I have practiced in for years.
To me the arguments have always come down to advertising and ethics. From an advertising perspective would we expect people to be affected by product advertising? Of course we would. The buying habits of the American population are shaped by advertising. Selling products is more of a science than people think. The American public can easily change its buying habits and can purchase products that are unnecessary and will be discarded after a brief period of time. They can also be sold on products like junk food that are unhealthy but designed to be sold in large quantities. Advertising would not seem to be the ideal basis for marketing drugs to physicians, but with many new products physicians are now bypassed and the drug is sold directly to the consumer. If the epidemiology of a particular problem like "low-T" is known, direct-to-consumer marketing probably leads to many, many more physician visits than a physician suggesting to their patient that they probably have primary or hypogonadotropic hypogonadism. All a patient has to do is go to the web site and take a non-specific checklist quiz on the features of "low-T" and be in their doctor's office to get the levels done within a week. Things will probably go a lot smoother without a physician intermediary in the loop and I am sure that much physician behavior will be shaped by the onslaught of men coming in to be tested for "low-T". I know for a fact that psychiatrists are approached for this problem because of the overlap between the syndrome and depression.
Part of the advertising argument has always been that there are unconscious factors in play. Really? That is the basis for all advertising in general. The main difference has been that pharmaceutical representatives have been schooled on the relationship aspects of the sale. They have been taught that basically if a physician likes them or feels indebted to them for free food, trinkets like poor quality pens that never seem to write very well, a round of golf, or tickets to the Lakers game that they may be more likely to prescribe their product. Most physicians were apparently naive enough to not realize that there was a huge marketing database out there that tracked their prescription writing to see if they were writing the required number of prescriptions for that product. In the real heyday of marketing bonuses to physicians, companies would pay for travel to important meetings.
While the people focused on the advertising influence kept chipping away mostly at psychiatrists, they seemed to ignore two important developments that made detailing or selling to individual physicians much less relevant. The first was restricted formularies. I was on the Pharmacy and Therapeutics Committee (P&T) of one of the largest health plans in the state and an affiliated hospital for a total of 10 years. During that time, the predominant factor in the decision about whether to put a drug on a formulary that would make it available to prescribing physicians was the cost. There were very few instances where a drug was so unique that it was made available even if it was very expensive. In those cases a drug might be available for an incurable illness that had a negligible benefit but it was included basically for public relations. One of the other overriding themes of the P & T Committee was that all drugs in a particular class (like antidepressants) were equivalent and therefore the least expensive drug in the class could be substituted for anything else. This potentially led to a lot of unnecessary chaos when medications fell out of favor due to pricing and patients needed to be shifted en masse to the least expensive drug. It gave hospitals and health plans leverage in dealing with pharmaceutical companies, but in some cases the deals were complex. As an example, in order to get a new blockbuster drug at a good price, the health plan would need to accept the same company's generic in a different class that had been removed because it was considered too expensive. Over a decade ago, business entrepreneurs decided that there was money to be made rationing medications to health plan enrollees and now a lot of that is done by pharmaceutical benefit managers (PBMs). PBMs are currently a multibillion dollar industry.
The second important development was generic drugs. Practically all of the blockbuster psychiatric medications of the past two decades are now generic drugs. Many generic drugs are easily affordable even as direct out of pocket purchases. At that point they are no longer actively marketed by the pharmaceutical company that held the exclusive patents. They are more likely to be the preferred drugs of PBMs and health plan formularies. They are in that role because of a scientific approximation. That approximation is that all drugs in a certain class, like antidepressants that have the same purported mechanism of action are equivalent and one can be substituted for another. That is clearly false but it allows the health plan to to provide you with the least expensive medication or charge you a hefty copay for one that is not. It also seems to not consider after market information that can even affect generic drugs. The best example I can think of there is the FDA warnings on citalopram. I would guess that despite the warnings, it remains a preferred drug by most health plans. Health plans in general seem to be geared up to prescribe antidepressants at higher and higher rates. I would take it a step further and venture a guess that most health plans have not taken a look at the data in their systems on whether or not they have observed problems related to the FDA warning on citalopram.
The ethical argument goes something like this. Physicians should have the best interests of their patients in mind and an advertising based conflict-of-interest to prescribe a certain drug creates an ethical concern. On the face of it, it seems like a straightforward argument. But there are several problems with it. For example, what is the direct evidence that this occurs - if any? Is it really believable that a physician would prescribe a decidedly suboptimal medication to a patient based on schmoozing with a pharmaceutical representative? There are often other factors in play. It is common to treat people with chronic illnesses who have suboptimal response to the current therapy and who are looking for the "next biggest thing" to try. A physician who has been detailed on the "next biggest thing" is likely to prescribe it if asked. There is a similar dynamic with the issue of overprescribing in general. If a patient persists in their request for an opioid, an antibiotic, a stimulant or any other drug are they likely to get it? The recent declaration that the CDC initiative to decrease antibiotic prescribing has failed would suggest that they will. Finally there is the dynamic of "see the doctor and leave with a pill." There are any number of scenarios where medications are used in medical practice and other options are not even discussed. The psychiatric cases are highlighted but it happens as frequently in cases of mild diabetes mellitus, back pain, chronic pain of various causes, hypercholesterolemia, mild hypertension and others. Many people have described this as "the doctor was poised over his prescription pad" but the healthcare industry is set up to see people in brief medication focused visits and physician reimbursement is tied to it. There are also patient related factors and a recent Tom Hanks interview is illustrative. He was on a late night talk show discussing his recent diagnosis of diabetes mellitus and he said his physician told him that if he could get back to his high school body weight he probably would not have it. His reply was: "Well I'm going to have Type II diabetes."
The ethical arguments, especially the ones I have seen constructed by physicians also ignore the general case of conflicts of interest at the professional level. Practically every major university department allows its faculty to supplement their salaries by consulting in private industry. In many cases that is a major source of additional income. In some cases those professionals are involved in setting standards and their approach is much different than the wall that is currently being constructed between the medical profession and the pharmaceutical industry. As an example, academic and industry professionals within the engineering profession are often on committees responsible for setting standards that govern all of the products within that industry. Their approach is to include as many industry professionals as necessary rather than suggesting the academics can set the standards themselves. Considering that pharmaceutical companies employ some of the top scientists in the world it would seem that medicine has a lot to lose if it goes along with the prevailing assumption. The prevailing assumption is that physicians are powerless to stop prescribing expensive medications that are of questionable benefit for their patients based solely on advertising and no scientific merit.
I applaud the GSK decision even though the above cited factors would suggest that for most physicians it has only historical relevance. I would encourage all of Big Pharma to adopt the same policies toward physicians. But this doesn't really go far enough and it is basically a token gesture at this point. To really make a difference I would suggest that they stop giving money to politicians. GSK spent $1.9 million on candidates and $4.9 million in lobbying last year. All of that money was directed at a few politicians. It is a part of a massive industry wide contribution to politicians. What do you think buys more influence, giving free pizza and pens to doctors or giving thousands to tens of thousands of dollars to politicians?
George Dawson, MD, DFAPA
Katie Thomas. Glaxo Says It Will Stop Paying Doctors To Promote Drugs. New York Times December 16, 2013.
Wednesday, December 18, 2013
Elimination of Homosexuality from the DSM - An Old But Important Story
I follow Michael Blumenfield's blog Psychiatry Talk and his most recent post reminds us that homosexuality was eliminated as a diagnostic category from the DSM 40 years ago. Incredibly he interviewed the President of the American Psychiatric Association at the time of this decision and has these interviews posted on his blog. Many years ago, I encountered a piece done on This American Life that documented another side to the process. In that discussion Robert Spitzer one of the main architects of the DSM was directly influenced by his attendance at a parallel meeting of gay and lesbian psychiatrists - informally self titled the GAYPA. He was apparently struck by the fact that homosexuality did not confer any disability in terms of psychiatric careers or social functioning and advocated for eliminating it from the DSM.
Dr. Freedman's interview (especially recording 2 and 3) starts to talk about the issues raised by the Committee for Concerned Psychiatry.(paragraph 4). The major issues of the day were opposing the Vietnam War and homosexuality as a disease. Dr. Freedman accepted their offer to be a petition candidate to oppose the "old boy's club" approach to APA presidency. He describes the 1972 APA Annual Meeting in Dallas where a gay APA member gave a talk wearing a disguise about how the DSM definition had harmed him. He received a standing ovation.
Dr. Freedman refers to Spitzer as the Chair of a Task Force to look into homosexuality. He prepared a document that supported dropping homosexuality as a diagnosis. At the same time the APA Board and members were strongly in favor of it. It was debated in committees on nomenclature, research and reference committees in a process similar to the recent DSM-5 process. The evidence to maintain the homosexuality was found to be unscientific, based on highly selected samples and it was rejected. The decision was front page news in both the New York Times and Washington Post. On December 16, 1999 the Washington Post selected the APA decision as one of the "stories of the century."
There was not complete consensus and two psychoanalysts insisted on a referendum at the next election and their petition was defeated by a margin of 2:1. Dr. Freedman provided this information because of criticism that the APA Board and not the membership favored the elimination of homosexuality. He points out in retrospect that there were other issues that he was focused on at the time including the theft of psychoanalytic records during the Watergate scandal and the reaction to that incident. He also raised the issue of psychiatric abuse in the Soviet Union and interview detainees who had been inappropriately placed in psychiatric hospitals. The APA contingent refused to travel to the USSR unless they would have access to patients in psychiatric hospitals and could interview them. The Soviets sandbagged the process by presenting cases of severe chronic mental illness and not allowing interviews.
The 81 Words piece is given primarily by Alix Spiegel, the granddaughter of John Spiegel a past President of the APA. At the time of this decision he was President Elect of the APA. She waxes rhetorical at times about psychiatry but I won't dwell on those details. They are minor in comparison with a well researched human interest story about the parallel stories that factored into this decision. She also discusses a parallel story within her family based on the occurrences at the time.
At the time that Dr. Spitzer decided to eliminate homosexuality as a diagnostic category he was probably early in his career in terms of designing diagnostic criteria and extending the DSM technology. He has described that process as basically reviewing literature, talking with experts and trying to type up a notecard with the criteria for that disorder. The MPR piece described his process with regard to the homosexuality question as more complex. He first met with a gay activist and wanted to understand that viewpoint. Several months later he arranged for three gay activists to present their case to the DSM nomenclature committee. A forum was organized at the 1973 APA Convention in Honolulu with an open debate between the analysts supporting homosexuality as a diagnosis, a faction of psychiatrists who did not, and Ronald Gold, the gay activist who befriended Spitzer. The event that led to the redraft that evening was Spitzer's attendance at the GAYPA party later that evening. After stating that he did not know any gay psychiatrists, he saw many notable psychiatrists at that meeting and went back to his hotel and redrafted the DSM criteria.
I have an interest in flagging these resources for future reference. Listen to the This American Life piece and the interviews by Dr. Blumenfield. This is a compelling story and clearly a decision that the APA and its membership got right. A common criticism of psychiatry is that it is unscientific or pseudoscientific and yet one of the main points in this historic decision was the rejection of psychoanalytic research that was considered unscientific. Dr. Freedman's commentary points out that the decision went through a process that seems to be very similar to the current DSM-5 process. Contrary to the flurry of criticisms of the DSM-5 before the recent release, this decision was precedent setting. It preceded most state laws regulating gay marriage by nearly 40 years. It was hailed as recently as 1999 as being a story of the century. And yet the press image of the DSM process suggested that the organization was socially inept and could not be trusted with similar decisions without close monitoring by non-medical organizations.
If anything this decision combined with precedent setting decisions on confidentiality, commenting on public figures, and banning psychiatry from participating in torture and capital punishment suggests that psychiatry should be one of the first professional organizations consulted. Anyone reading this blog gets the message that the APA is far from perfect, but at times they get it very right. This is a forty year decision that has stood the test of time and is also a good example of activism within the organization as a driving force. Activism and political tension within the organization can be as important as the science behind the position.
George Dawson, MD, DFAPA
1. This American Life. 81 Words. January 18, 2002. The NPR story of how the American Psychiatric Association decided that homosexuality was no longer a mental illness.
2. Michael Blumenfield, MD. 40th Anniversary of "Homosexuality" Being Removed from DSM.
3. DSM-II Change - The actual DSM-II change involved the category "Sexual Deviations". The introductory paragraph was 81 words long and "302. Homosexuality" was removed from the list. It begins with the sentences:
"This category is for individuals whose sexual interests are directed primarily toward objects other than people of the opposite sex, toward sexual acts not usually associated with coitus, or toward coitus performed under bizarre circumstances as in....."
Dr. Freedman's interview (especially recording 2 and 3) starts to talk about the issues raised by the Committee for Concerned Psychiatry.(paragraph 4). The major issues of the day were opposing the Vietnam War and homosexuality as a disease. Dr. Freedman accepted their offer to be a petition candidate to oppose the "old boy's club" approach to APA presidency. He describes the 1972 APA Annual Meeting in Dallas where a gay APA member gave a talk wearing a disguise about how the DSM definition had harmed him. He received a standing ovation.
Dr. Freedman refers to Spitzer as the Chair of a Task Force to look into homosexuality. He prepared a document that supported dropping homosexuality as a diagnosis. At the same time the APA Board and members were strongly in favor of it. It was debated in committees on nomenclature, research and reference committees in a process similar to the recent DSM-5 process. The evidence to maintain the homosexuality was found to be unscientific, based on highly selected samples and it was rejected. The decision was front page news in both the New York Times and Washington Post. On December 16, 1999 the Washington Post selected the APA decision as one of the "stories of the century."
There was not complete consensus and two psychoanalysts insisted on a referendum at the next election and their petition was defeated by a margin of 2:1. Dr. Freedman provided this information because of criticism that the APA Board and not the membership favored the elimination of homosexuality. He points out in retrospect that there were other issues that he was focused on at the time including the theft of psychoanalytic records during the Watergate scandal and the reaction to that incident. He also raised the issue of psychiatric abuse in the Soviet Union and interview detainees who had been inappropriately placed in psychiatric hospitals. The APA contingent refused to travel to the USSR unless they would have access to patients in psychiatric hospitals and could interview them. The Soviets sandbagged the process by presenting cases of severe chronic mental illness and not allowing interviews.
The 81 Words piece is given primarily by Alix Spiegel, the granddaughter of John Spiegel a past President of the APA. At the time of this decision he was President Elect of the APA. She waxes rhetorical at times about psychiatry but I won't dwell on those details. They are minor in comparison with a well researched human interest story about the parallel stories that factored into this decision. She also discusses a parallel story within her family based on the occurrences at the time.
At the time that Dr. Spitzer decided to eliminate homosexuality as a diagnostic category he was probably early in his career in terms of designing diagnostic criteria and extending the DSM technology. He has described that process as basically reviewing literature, talking with experts and trying to type up a notecard with the criteria for that disorder. The MPR piece described his process with regard to the homosexuality question as more complex. He first met with a gay activist and wanted to understand that viewpoint. Several months later he arranged for three gay activists to present their case to the DSM nomenclature committee. A forum was organized at the 1973 APA Convention in Honolulu with an open debate between the analysts supporting homosexuality as a diagnosis, a faction of psychiatrists who did not, and Ronald Gold, the gay activist who befriended Spitzer. The event that led to the redraft that evening was Spitzer's attendance at the GAYPA party later that evening. After stating that he did not know any gay psychiatrists, he saw many notable psychiatrists at that meeting and went back to his hotel and redrafted the DSM criteria.
I have an interest in flagging these resources for future reference. Listen to the This American Life piece and the interviews by Dr. Blumenfield. This is a compelling story and clearly a decision that the APA and its membership got right. A common criticism of psychiatry is that it is unscientific or pseudoscientific and yet one of the main points in this historic decision was the rejection of psychoanalytic research that was considered unscientific. Dr. Freedman's commentary points out that the decision went through a process that seems to be very similar to the current DSM-5 process. Contrary to the flurry of criticisms of the DSM-5 before the recent release, this decision was precedent setting. It preceded most state laws regulating gay marriage by nearly 40 years. It was hailed as recently as 1999 as being a story of the century. And yet the press image of the DSM process suggested that the organization was socially inept and could not be trusted with similar decisions without close monitoring by non-medical organizations.
If anything this decision combined with precedent setting decisions on confidentiality, commenting on public figures, and banning psychiatry from participating in torture and capital punishment suggests that psychiatry should be one of the first professional organizations consulted. Anyone reading this blog gets the message that the APA is far from perfect, but at times they get it very right. This is a forty year decision that has stood the test of time and is also a good example of activism within the organization as a driving force. Activism and political tension within the organization can be as important as the science behind the position.
George Dawson, MD, DFAPA
1. This American Life. 81 Words. January 18, 2002. The NPR story of how the American Psychiatric Association decided that homosexuality was no longer a mental illness.
2. Michael Blumenfield, MD. 40th Anniversary of "Homosexuality" Being Removed from DSM.
3. DSM-II Change - The actual DSM-II change involved the category "Sexual Deviations". The introductory paragraph was 81 words long and "302. Homosexuality" was removed from the list. It begins with the sentences:
"This category is for individuals whose sexual interests are directed primarily toward objects other than people of the opposite sex, toward sexual acts not usually associated with coitus, or toward coitus performed under bizarre circumstances as in....."
Subscribe to:
Posts (Atom)