A study on antipsychotic medication reduction and
discontinuation came out yesterday with fanfare. The fanfare was basically because the principal
investigator is a self-proclaimed critical psychiatrist with many criticisms
of psychiatric medication and the results of her trial contradicted the primary
hypothesis of the study and that was:
“Our hypothesis was that antipsychotic reduction would improve
social functioning with only a small increase in relapse rate.”
Relapse rate in this case was defined as rehospitalization
and the authors subsequently state that they thought a 10% rate of relapse
would be “acceptable.” The irony of this
situation (ideology versus real world treatment) was not lost on anyone.
Several people seemed to congratulate the authors on publishing results inconsistent with their ideology although the study was so embedded in the UK
research infrastructure – I doubt that not publishing it would have been an
option.
As a clinical trialist myself – the research seems to
present several problems and creates several questions that could suggest that
it was designed to optimize the likelihood that antipsychotic medication could
be reduced and possibly discontinued. Before I get into those scenarios let me briefly summarize the results. The paper
is open access and can be downloaded as well as another
paper that describes the research protocol.
In the study there were two arms an antipsychotic maintenance
arm (N=127) and a reduction arm (N= 126). Diagnoses were taken from clinical
information and the clinical staff had treatment responsibility for the patients. In those patients who were randomized to dose
reduction, a tapering protocol was suggested to the clinical staff and if it went well at some point the option for a more rapid taper or discontinuation was offered. The
research staff monitored the protocol. Baseline and outcome measure included a
number of checklists to assess side effects, sexual side effects, positive and
negative symptoms, quality of life, and social outcomes at the reassessment points. Raters were blinded but the measures are essentially self report. The ultimate result was
that the risk of adverse outcomes was worse in the reduction arm with no
associated improvement in social functioning.
He are some potential issues that I noticed based on my experience in clinical trial design and on research review boards.
1. Recruitment
– described in the following:
“Participants were recruited from 19 National Health
Service Trust mental health organisations across England. Potential participants
were identified initially by clinical staff or recruited through advertisements
placed in clinical settings and social media; those patients who expressed an
interest in participating were sent further information”.
Not enough information. What did the advertisements say?
Were subjects aware of who was running this trial and what the goal of the
research was? Were the patients asked why they were interested in participating
in this trial? Were they asked what they think about taking a medication? Did the subjects have any
exposure to the considerable press that the critical psychiatry group and the principal
investigator generate? Descriptions in
the lay press have been demonstrated to have significant effects on perceived
side effects – even to the point of creating a nocebo effect (6) – is there any
reason to think that a group emphasizing side effects and minimizing any therapeutic
effects might have a similar impact? If that is the case – how would it affect
this trial?
2. Inclusion/Exclusion
criteria –
“Exclusion criteria included being considered by a
clinician to pose a serious risk of harm to self or others were the individual
to reduce their antipsychotic medication, being mandated to take antipsychotic
medication under a section of the Mental Health Act, having been admitted to
hospital or treated by a crisis service for a mental disorder within the last
month, lacking capacity to consent, having insufficient spoken English,
pregnancy, breastfeeding, and being involved in another trial of an
investigational medical product; eligibility was assessed by researchers and
confirmed by the Principal Investigator for the site.”
Practically all the exclusion criteria result in a
population that may be more likely to discontinue antipsychotic medications
with less difficulty. Consistent with this is the antipsychotic doses of both
the reduction and maintenance arm of 300 mg chlorpromazine
equivalents (on average). According
to the Maudsley Prescribing Guidelines (4) 300 mg chlorpromazine is considered the
minimally effective dose of medication for relapsing schizophrenia. Whether
this was a representative sample of the 4109 patients put forward for research
by clinicians a comparison of the demographics and medication doses would have
been of interest.
Selection bias may also be evident in the Consort diagram
(page 4). After subjects consented to be
contacted by the research team (N= 958) – a total of 562 declined participation.
Was that because they did not want to take the chance of randomization to a
medication reduction?
3. Diagnoses –
the diagnosis required was schizophrenia or non-affective psychoses with recurrent
episodes. The diagnoses were taken from clinical records. Considerable heterogeneity is introduced with
the non-specific category of psychoses with an unpredictable course for which
the concept of maintenance medication was not intended.
4. The Dose Reduction
-
The description of the dose reductions in the paper is
confusing. It starts out describing
individualized reductions every 2 months based on starting doses but at some
point states the patient is allowed to discontinue the medication if the dose
reduction has been going well or reduce at a rate of the equivalent of 2 mg haloperidol/day.
2 mg/day of haloperidol is not a slow
reduction and it is a departure from reduction every 2 months. Some of the
authors here have written about antipsychotic withdrawal reactions – how is the
more rapid dose reduction or optional abrupt discontinuation justified?
4. Safety
Monitoring/Informed Consent:
The more clinical trials I read (and I have read thousands)
– the more I want to see the consent form that each patient signs. Some of the
authors here continuously talk about medication side effects. In fact – the principle investigator (PI) has
stated that in her opinion that modern psychiatric medications work in a "drug
centered" rather than a disease centered model by producing side effects like sedation,
cognitive impairment, dysphoria, and loss of libido (5). In that model, symptoms of mental illness are
muted by side effects rather than effectively treated. The model essentially
denies the possibility of effective treatment without medication side effects. Of course, there are medication side effects
but consent forms also must contain a discussion of the risks of the
intervention. How are they listed when the investigators do not believe they
can be directly addressed? Were the
subjects told about the risk from medication discontinuation of recurrent
psychosis, suicidal thinking, and death?
That seems especially relevant in a study where the intervention arm had
twice as many deaths as the maintenance arm (see Table 4).
Along those same lines – the protocol paper for the study
(2) states that a Data Safety and Monitoring Board (DSMB) assessed the ongoing
safety of the protocol and made recommendation to a Programme Steering
Committee providing independent oversight – even to the point of stopping the
protocol if there was a substantial increase in adverse events related to the
intervention. Was there a threshold? In this case why was that threshold not
met? In the trials I have been involved
with the PI and the physician responsible for monitoring safety (typically me)
had to clearly delineate a safety plan if any of the research subjects
developed medical or psychiatric complications from the intervention. In this case that responsibility seems to
have been delegated to the clinicians originally treating the patient.
In the reported causes of death of the trial participants –
how is the death of a research subject in the reduction arm attributed to
antipsychotic medication when they have been on a low dose, were being followed
clinically in an outpatient clinic, and their dose was presumably being
reduced? One patient in each arm died of
an “accidental overdose”. What medication was implicated in the accidental
overdoses?
This protocol is also a case of shifting risk for the
research to the clinicians. Here the
research staff designs an intervention that likely will lead to worsening clinic
status and the subjects are followed in a treatment as usual manner. Were any
additional safeguards in place for that eventuality? For example – were the subjects informed that
they could contact the principal investigator or research coordinator if things
were not going well?
These all seem like significant safety questions to me.
5. Social Functioning Scale (SFS) to measure the primary outcome -
The measured results with this scale are in the top line of Table 2 at 6, 12, and 24 months. The scale has 79 items that are assigned to assess social functioning. Is there a problem with taking a cross sectional sample of people stabilized on medications and hypothesizing they will function better being tapered off antipsychotic medication? There is an obvious problem and that is there is no accounting for the improvement in social functioning due to the medication in the first place. In other words - what would the subjects have scored leading up to and during the episode of acute or recurrent psychosis - the reason they are taking the medication in the first place. What would the trajectory of these scores be over time? Stabilization of psychosis involves a lot more than treating hallucinations, delusions, and thought disorder symptoms. With stabilization there is an improvement in social behavior. The design of the trial suggests that the problem began with medications rather than a significant psychiatric disorder.
There is a concept in clinical psychiatry and that is trying to get the patient as close as possible to their baseline level of functioning. That requires a knowledge of what they were like before the onset of illness and restoring as much functional and social capacity as possible. That also typically means minimal to no medication side effects if possible.
6. What is supported
reduction of antipsychotic medication?
Is there a protocol that I missed? I could not find what this means anywhere in
either the protocol or final paper or in the supplementaries. If I was tapering an antipsychotic medication
I would meet more frequently with the patient, inform them of what we
need to watch for, have additional caregiver and family involvement, and encourage
them to call me at specific signs of early problems due to the dosage
reduction. In a research protocol, research staff would call and check on how the
subject was doing. I would call all of that treatment as usual (TAU) when it
comes to antipsychotic medication reduction. Is supported reduction more than
that? Even TAU has been implicated as a
potential placebo enhancing effect. Did it have that effect on the intervention
in this case?
7. The overstated
conclusion:
“Our findings provide information for people with schizophrenia
and related conditions about the probable medium-term impact of reducing the
dose of their antipsychotic medication, and they highlight the need for collaborative
decision making based on the sharing and careful consideration of all the
evidence.”
Actually, it doesn’t.
This is what clinical psychiatrists do and more specifically it is what
I did for 35 years of practice. I can still recall community psychiatry
seminars with Len Stein, talking about dosage reductions of antipsychotic
medications and the implication of a WHO international study looking at that
problem in schizophrenia. That seminar
was in 1986. Collaborative decision making seems to be the latest term for informed consent and therapeutic alliance. Informed consent means that the patient is given enough information and discussion so that they can make a decision about the direction of their care including any medications, tests, or other interventions used. The therapeutic alliance is the affiliative relationship between the patient and physician aligned to address the patient's problems and diagnoses. It is by longstanding definition a collaboration.
What the authors did encounter but did not discuss was the
tendency of people on antipsychotics to just discontinue them (several in the maintenance
group did this), how much withdrawal was encountered, and why there were no
group categorical differences in side effects with the taper. According to the Glasgow Antipsychotic Side-effect Scale (GASS) guidelines all subjects remained in the moderate side effect range. And if medications work through side effects as the critical psychiatrists say why did the subjects in the dose reduction group worsen?
Those are a few of the problems that jumped out at me as I
read this paper and the associated backgrounder. As can be seen from the above
discussion many of these design factors potentially optimize the intervention
group in the direction of proving the authors’ hypothesis. It also limits generalizability to other clinical settings. That makes the
result of the trial even more significant.
It also raises some issues that seem more prominent in recent years as pharmaceutical
conflict of interest seems to ring hollow.
Is there an ideological conflict of interest and how is it determined? How does it affect research design, results, and the discussion of research findings?
George Dawson, MD, DFAPA
References:
1: Moncrieff J,
Crellin N, Stansfeld J, Cooper R, Marston L, Freemantle N, Lewis G, Hunter R, Johnson
S, Barnes T, Morant N, Pinfold V, Smith R, Kent L, Darton K, Long M, Horowitz M, Horne R, Vickerstaff V, Jha
M, Priebe S. Antipsychotic dose
reduction and discontinuation versus maintenance treatment in people with
schizophrenia and other recurrent psychotic disorders in England (the RADAR
trial): an open, parallel-group, randomised controlled trial. Lancet Psychiatry
September 28, 2023DOI:https://doi.org/10.1016/S2215-0366(23)00258-4.
2: Moncrieff J,
Lewis G, Freemantle N, Johnson S, Barnes TR, Morant N, Pinfold V, Hunter R,
Kent LJ, Smith R, Darton K. Randomised controlled trial of gradual
antipsychotic reduction and discontinuation in people with schizophrenia and
related disorders: the RADAR trial (Research into Antipsychotic Discontinuation
and Reduction). BMJ open. 2019 Nov 1;9(11):e030912.
3: Danivas V,
Venkatasubramanian G. Current perspectives on chlorpromazine equivalents:
Comparing apples and oranges! Indian J Psychiatry. 2013 Apr;55(2):207-8. doi:
10.4103/0019-5545.111475. PMID: 23825865; PMCID: PMC3696254.
4: Taylor D, Paton
C. The Maudsley prescribing guidelines. CRC press; 2009 Oct 30.
5: Middleton H,
Moncrieff J. Critical psychiatry: a
brief overview. BJPsych Advances (2019), vol 25, 45-54.
6: Colloca L, Barsky
AJ. Placebo and Nocebo Effects. N Engl J Med. 2020 Feb 6;382(6):554-561. doi:
10.1056/NEJMra1907805. PMID: 32023375.
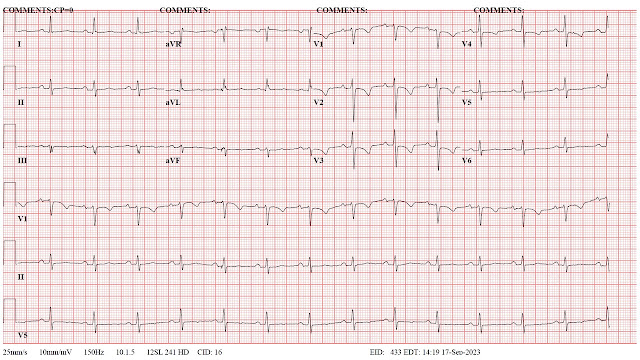
Photo Credit:
Many thanks to my colleague Eduardo A. Colon, MD for the photograph at the top of this blog.