After some deliberation I went into my local Walgreens for
an RSV immunization. I have multiple
unpredictable allergies and have had both anaphylaxis and significant local
reactions to vaccinations in the past. Like 20% of the population, I have
eczema and there is some research on flareups of this skin disease with
vaccinations. And like many people with
eczema, I also have asthma and had a severe flare-up of asthma when I got a
viral infection on a flight back from Alaska about 5 years ago. My primary care
physician recommended it last week so I scheduled it.
As I was sitting there waiting for them to prepare the
shot, I was able to observe patients coming and going to pick up their
prescriptions. This is a busy Walgreens and there are people going past the
drive-up window as fast as they are showing up in line. Most people at there in the early afternoon
are retirees. There was an informal
retirement poll of the old guys in line and it was unanimous – we were all
quite happy to be retired. The people gathered were upbeat. I recalled being at
a 24-hour pharmacy in 2002. My late
father-in-law was visiting and forgot all his cardiac medications. I went over at midnight to pick them up and
it was an ugly scene. There were about
60 people there and the pharmacist was not filling the prescriptions fast
enough. From where I was seated – I could see him working furiously. The crowd was so agitated about this it
seemed like they were ready to riot. If that wasn’t enough a rather cranky lady
sitting next to me started to goad them and call them names. Luckily, I got the medicine and got out of
there as soon as possible.
The atmosphere today
was much better – but like most scenes in American health care it was far from
perfect. There were no simple
transactions. In the transactions I witnessed, very few people walked away with
the prescription medication ordered by their doctors. The most common problem
as a lack of prior authorization. People were advised that their doctor had to
get the prior authorization. Several were advised that they needed a new prior
authorization. I remember all the messaging that people hear when they need a
prescription refill. Call your doctor’s
office. Don’t call your doctor’s
office. Call the pharmacy. Don’t call the pharmacy. Today 75% of that messaging was
incorrect. And it wasn’t like the
medications were an option.
Antihypertensives, diabetes medications, prostatic hypertrophy
medications – every medication name I heard had me hoping these impasses would
be resolved as soon as possible for the patient’s sake. The related quality
issue is that most of these medications were maintenance medications and yet
they required reauthorization – in some cases just because of an insurance
change. I didn’t see anyone get hit with
the Medicare
Donut Hole. I have been twice in the past 3 months with a copay for
apixaban ballooning up to $400 or roughly 7 times the usual amount just because
of the way the rules are written to favor pharmaceutical companies and pharmacy
benefit managers (PBMs). I am sure it would have happened if I had been there
longer.
But 20 minutes was up and I did not have an anaphylactic
reaction. Another immunization I can take.
I jumped in my car, turned the radio on, and thought about what I had
just witnessed. I am certainly no
stranger to it. As a physician I have been harassed by PBMs. They put me on hold for hours only to
eventually connect me with a clerk with no medical training or credentials that
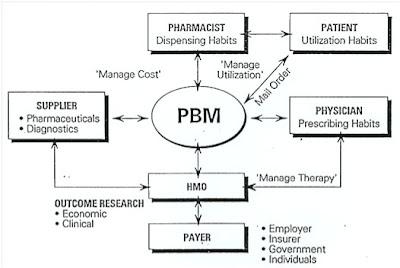
would either approve or reject my recommended prescription. PBMs are not some quality improvement project
– they are patient and physician harassment to see who blinks first and loses
the time and money. They are
multibillion dollar companies that add to the cost of medications rather than
reducing the cost.
Overall prescription drug pricing in the United States is
much higher than in comparable countries both on an overall basis and a brand
name basis. A study (1) that looked at
2018 data showed that all drug pricing ranged average 258% higher than
comparable drugs purchased in Mexico, Canada, France, Germany, Italy, Japan and
the UK. Comparable brand name
medications averaged 344% higher. All of
that translates to much larger copays for Americans and often an inability to
purchase the medication. I saw that happening a lot today.
Advocacy from the physician side has been weak. After
decades of no action on the prior authorization issue some professional
organizations are now saying that it needs to be controlled. The problem with
that position is that it is so ratchetted down on patients and physicians that
any controls in the right direction will be trivial. The only solution is to eliminate prior
authorization completely. If pharmaceutical companies want to deny payment for
prescription medications – they can do it directly without using the physician
and pharmacist for cover. Beyond that the appeal can go through a state
administrative authority independent of the pharmacy business.
I have written extensively in the past about the sheer
amount of resources that are wasted on prior authorization and the associated
pharmacy rationing strategies. I have
written about how pharmacists take a significant hit and their professionalism
is adversely affected by poor PBM reimbursement and conflict of interest –
especially when the PBM owns their own chain of pharmacies. Today as I was
waiting for clearance after an immunization it was all about the human cost.
That never seems to get better, although the Obama and
Biden administrations have provided some significant
relief to Medicare recipients. Everyone involved would be happier if this
system was just gone.
George Dawson, MD, DFAPA
Supplementary 1: Additional inefficiencies - a couple of days after writing this post my wife got a text message that one of her prescriptions was ready and she could "pick it up after Sunday." She asked me to pick it up on Monday because I was driving by the pharmacy. I pulled up to the window and asked for the prescription and was told - "it is ready but you are one day early. You can pick it up tomorrow." Not the first time that has happened. The pick up rule seems to vary by PBM, insurance, and pharmacy but the automatic messaging obviously does not take it into account. Just another reason for going to the pharmacy and leaving without the prescription.
References:
1: Mulcahy AW,
Whaley C, Tebeka MG, Schwam D, Edenfield N, Becerra-Ornelas AU. International Prescription Drug Price Comparisons
Current Empirical Estimates and Comparisons with Previous Studies. Rand Corporation Research Report. 2021.
2: Yetter DM. Reprieve for Kentucky’s independent pharmacies is saving Medicaid millions. Kentucky Lantern. October 5, 2023. https://kentuckylantern.com/2023/10/05/reprieve-for-kentuckys-independent-pharmacies-is-saving-medicaid-millions/
This is the story of how Kentucky eliminated PBMs in their state and saved $283M in three years.
Graphic credit:
Me - my wife reshot the photo.