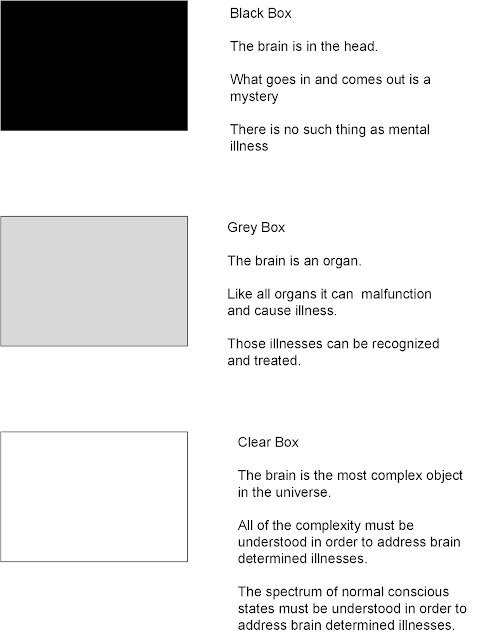
In order to bring some clarity into the discussion of why neuroscience is important for psychiatrists, I thought I would get back to the basics. I have three models in the above graphic that I think represent the basic conceptualizations of the brain in my lifetime. They are very basic models, but I think reasonable jumping off points for further discussion. They also serve to make my point about the importance of neuroscience. I realize that there is a natural human tendency to be argumentative. When I mention neuroscience or even science it seems that many psychiatrists and interestingly their detractors both get irritated. I can understand why the detractors are irritated since many of them are at the level of Black Box thinking in the above diagram. I will elaborate further, but many of them seem to consider the brain an amalgam of various qualities that either defy understanding or are unnecessary to understand because the brain may be involved at the very periphery of human behavior if at all. But I don't understand any attitude on the part of brain professionals like psychiatrists that doubt the importance of neuroscience. With that let me proceed with the three levels of thought about the brain in the above diagram.
The Black Box embodies what people have thought about the brain since the beginning of time. The brain is a mystery on the one hand and immutable on the other. The reality of that situation could not be denied for long. It was obvious that people with clear brain damage who survived the initial insult could have a number of changes in cognition, personality, and social behavior. The black box view eventually gave way to mind-body dualism that held there were a number of mental phenomenon that could not be explained by physical properties alone. That is really the last refuge of the Black Box and that is that the conscious human state has not been explained in terms of how it arises from the neural correlates of consciousness. It is an active area of research in the Clear Box area today. It is always interesting in terms of who adheres to Black Box thinking these days. I can't think of any legitimate science that occurs using this model. Pre-modern and modern neuroscience if anything has clearly dispelled black box and most mind-body duality. Some philosophers and antipsychiatrists are at this level.
In the Grey Box Box things got clearer. The transition from Black to Grey to Clear is not a well defined boundary. The best example that I can think of is German neuropsychiatry at the beginning of the 20th century. Much of that movement was focused in asylums. There is a famous picture of giants in the field like Kraepelin. Alzheimer, Nissl, Binswanger and others who were active at the time. These psychiatrists made good phenomenological observations but they were also focused on gross neuroanatomy. In the case of some illnesses like Alzheimer disease some observations could be made at autopsy. In the case of schizophrenia and bipolar disorder, gross anatomical changes were not evident. Although that is a negative finding. it is a finding that propelled a century of more sophisticated neuroanatomy, neurophysiology and the beginnings of a much more sophisticated molecular biological approach to functional mental illnesses or illnesses with no gross anatomical or physiological markers.
While neuroscience was moving forward at a slow pace, there was some slight progress on the fronts of diagnosis and treatment. The DSM is always a controversial document, largely because there is never any shortage of self-proclaimed experts in psychiatry. Psychiatrists know the limitations, what can be tested for, what physical illnesses are important to rule out, and what states can be cause by drug or alcohol intoxication, chronic use and withdrawal. These medical and intoxicant induced states are all clear medical illnesses by any definition as well as the associated syndromes. There is a disclaimer in the DSM about who should be using it. Training is required to conduct the appropriate evaluations and make the appropriate diagnosis. Further training is required to assure that patients can be safely treated. Associated medical conditions need to be recognized and diagnosed. All of this came about as a result of a medical focus that was reemphasized with the advent of the DSM. Prior to that there was an overemphasis on psychoanalysis and psychodynamic psychotherapy. A darker Grey Box consisted of a brain full of psychoanalytic constructs and the diagnosis and treatment was overly dependent on this model.
DSM technology was a required step in refocusing psychiatry on medicine and the brain as an organ. But that occurred 40 years ago. During that time, psychiatrists diagnoses and treat people based on clinical experience and general patterns that they recognize in the course of their training and practice. In some cases the DSM has very clear criteria that are very helpful - like the definition of a manic episode. In other cases - like the difference between anxiety and depression there are problems. The same patients can endorse predominately anxious symptoms one week and predominately depressive symptoms the next. The severity of the illness can typically lead to a clearer diagnosis and that is most likely due to the fact that the boundary between a clinical case and normal is arbitrarily defined as impairment in functioning. More impairment should lead to clearer diagnosis. Better markers to classify illness and hopefully predict treatment response are needed. The search for these markers is an active area of investigation. Psychiatry will remain in the Grey Box without these markers and more clear-cut treatments that address the underlying biological changes.
A lot of pharmacological research was done during the DSM era. There was a lot of discussion about neurotransmitter and receptor pharmacology and the implications for scientific treatment. Like all science, receptor pharmacology and post synaptic cell signalling mechanisms do not stand still. There are many theories of receptor and drug pharmacology that have stood the test of time. With a focus on the pathological nobody could hope that drugs that were often accidentally discovered would lead to highly effective treatments or a more comprehensive theory of mental illness or normal brain function. Clinical trials of psychiatric drugs and studies of pharmacology and physiology are are also limited by research subject heterogeneity. That is a problem with research on any complex polygenic illness. In the case of pure mental illness where any medical cause has been ruled out, the DSM criteria alone are a poor filter for selecting homogeneous populations for research.
Drug and psychotherapy research in the Grey Box have both suffered from treatments being applied to heterogeneous populations. There is no researcher that I know who thinks that any two people with a DSM diagnosis are similar to the point that drug or medication response would be high or necessarily reproducible. Apart from the diagnostic problem, the DSM suggests homogeneity in a context where any seasoned clinician knows differently.
The Clear Box is the goal here. The knowledge needed to get to this box is much more comprehensive. It recognizes brain complexity and the importance of the conscious state rather than just a collection of DSM descriptors. Despite the fact that many of the basic mechanisms were elucidated over 40 years ago neuroscience has detractors just like psychiatry. A common strategy of neuroscience detractors is to take either a research finding or a media quote and "debunk" it with fanfare in the popular media. Ulterior motives are often suggested for connecting neuroscience primarily with psychiatric disorders. Many of these detractors depend on their own characterization of the original research and the cultural phenomenon of piling on with negative criticism to score what appears to be a victory with the vocal and like minded. They use the same strategy in claiming that mental illness or addictions are "not diseases" like "real" diseases - despite the fact that the general population considers them to be equivalent. I find nothing compelling about critiques of ongoing science and medicine by the unqualified. The main problem is that the people truly qualified to produce the criticism are ignored in favor of what amounts to unscientific criticism. There is a secondary problem with the proliferation of journals, especially opinion pieces rather than scientific papers.
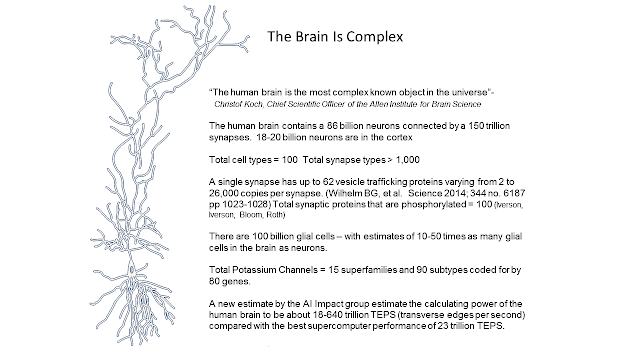
Another interesting thought that I had about the Clear Box is that many people have no difficulty at all in recognizing that machine intelligence is improving and that at some point it might exceed human intelligence. They don't seem to have any problem in figuring out whether a computer may have negotiated the Turing Test and seem indistinguishable from another human being. Many people seem to have difficulty recognizing the computational capacity of the human brain and the result of that complexity. Despite some philosophical arguments - that is a possible reason for not seeing the Clear Box as the preferred state of brain knowledge.
I have tried to point out many times that one key element of the mischaracterization of neuroscience in psychiatry is a basic lack of understanding of science. Science is a process and a dialogue. Medical science is more of a process and a dialogue than physical science - the processes involved are more complicated and the experiments involve proportionally fewer relevant variables. There are no differential equations based on a few variables that explain how the brain works. Entire blocks of research can end up partially true or a dead end. That does not mean there is some grand conspiracy - that just means it is time to move on to a new paradigm.
George Dawson, MD, DFAPA
Quotation Credit:
"The brain is the most complex object in the known universe" is a quote from Christof Koch, Chief Scientific Officer of the Allen Institute for Brain Science and well-known consciousness researcher.
Tip For The Better Graphic:
The graphic at the top is rendered with Visio. Blogger makes it blurry and ill defined. Click on it for the sharp Visio version.