It has been a week since I gave a presentation to the Philolectian
Society in Anoka, Minnesota. The Philolectians
are primarily retired educators and their colleagues who decided they wanted to
promote education in their county. They do this by topical discussions on a
monthly basis and fund raising for scholarships that they award to high school
students. They were founded 134 years ago. I gave them a presentation on substance
use disorders about 5 years ago – but my current presentation was entitled “Everything
You Wanted To Know About Psychiatry In 30 Minutes of Less.” It was the mile high view – but that is the
one that is typically lacking in American culture.
The venue was a sports bar conference room in an old building.
There was no projection equipment and it had spotty WiFi coverage so I decided
I should test it out ahead of time. I opted to use a Chromecast device to the
television HDMI port – but did not realize at the time that it does require
WiFi in order to work. Connection to my
home TVs was not a problem but there is continuous WiFi as the background. Failing the Chromecast, I was given an LED projector
that also required WiFi. I ended up printing out hand outs for the attendees. The
12 slides follow and total time was about 45 minutes – 30 minutes of
presentation and a 15 minute Q & A.
My presentation style is to focus on slide design. For that reason I avoid the standard templates
and try to cover as much of the slide with graphics as possible when they are
used. My second overall principle is to
free associate to the slides and never read them. They are there to keep me on
track. What I actually end up saying
varies considerably from lecture to lecture – modifiable by various factors
including what the group has indicated what they want to hear, what I have been
thinking about that day, and what I have been reding that week. The process is like
Frank Zappa described his guitar playing. Every live performance is unique – no
set of notes is identical. I can’t claim
mastering lectures like he mastered the guitar but there is some creative
process involved in lecturing.
The title slide uses a background of abstract art taken off
of one of my paintings at home. The artist is Stephen Capiz. It represents a very small area of a larger abstract
painting with the tile information superimposed. The title was chosen to keep the
atmosphere casual. I wanted people to be comfortable that this was not a
presentation to mental health professionals but to a general audience.
Slide number 2 is a critical three - fold message that is
frequently missed or distorted.
Psychiatric disorders have been observed and discussed since ancient
times. That means they are easily
recognizable to people with no training. It means that they are real and can’t
be explained away. You must be
incredibly naïve or sheltered to not have that experience. Psychiatrists only exist because they were the
doctors interested in treating these disorders. That is as true today as it was
in the 18th and 19th century. The only difference is that modern
psychiatrists have uniform training. And finally as you would expect, the
diagnostic system has undergone successive refinement over the centuries. The DSM is used as an example here but the
ICD could be used as well. (with all slides click on them to expand and get a better quality graphic - this is apparently an artifact of the blogger format).
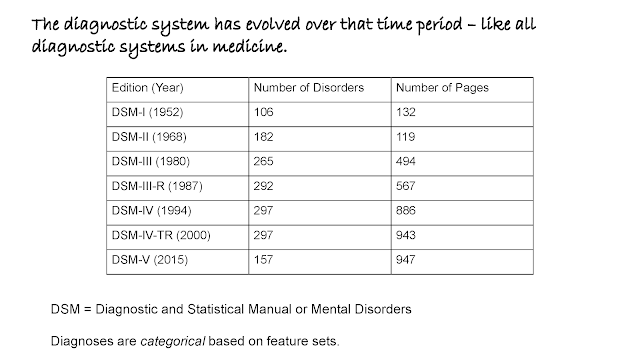
Slide 3 provides a
little more detail on the evolution of the DSM systems. Counting the total
diagnoses is always a point for rhetorical digressions. I finally figured out how to do it and listed my specific technique in this post. To a
professional audience, I might include studies on how many of the diagnoses are
actually used. This audience did not
find any of this controversial.
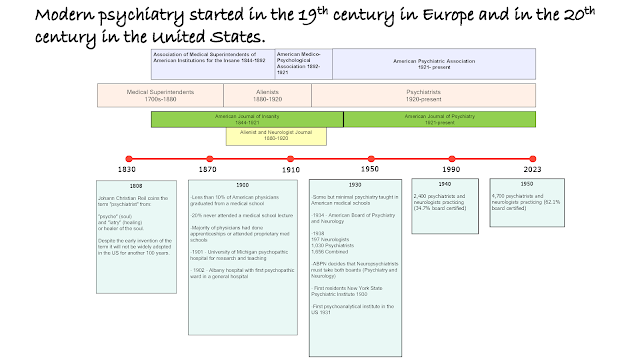
Slide 4 is a great timeline of how psychiatry developed from
a discipline that Kendler refers to as protopsychiatry to the modern era starting
in about 1920 in the US and about 40 years earlier in Europe. The audience was extremely
interested in the low percentage of physicians attending medical schools in
1900 and that lectures could be attended by purchasing tickets. The transition
from asylum doctors with no particular training to psychiatrists was also a
focal point.
Slide 5 was necessary because there is still a lot of emphasis
on Freud. I remembered that Freud was an important figure to my college English professors and that some of the teachers in the audience were about that age. I emphasized that Freud was an important figure in psychoanalysis,
but that there were many European psychiatrists that provided knowledge, literature, and
training to their American counterparts and that many were self-taught and
active across the fields of psychiatry, neurology, neuropathology, and
neuropsychiatry.
Slide 6 is a very brief outline of the basic educational milestones
of the various mental health disciplines.
Minnesota has a confusing array of designations including unlicensed
mental health practitioners so I kept it simple. In the previous slide on the psychiatry
timeline I did mention how in the early 20th century most
practitioners considered themselves neuropsychiatrists and practiced both
neurology and psychiatry. When the American board of Psychiatry and Neurology
informed practitioners that they would need to take board exams in both
psychiatry and neurology the era of separate specialties was begun.
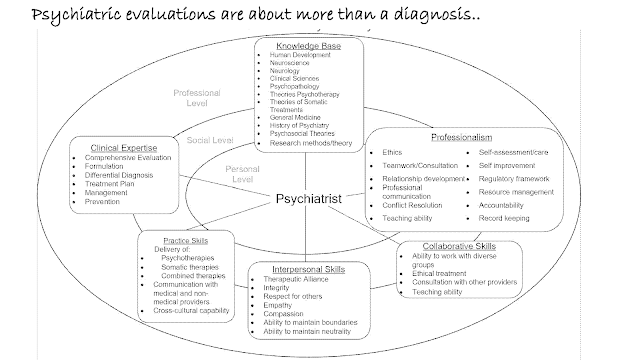
Slide 7 is one of my favorite graphics. It is produced from the current educational
requirements for residency training and Melissa Farmer, PhD greatly assisted me
with the graphic design. My overall emphasis was to point out how these training requirements
should result in a physician who is not only an expert in diagnosis, but also
interviewing, maintaining relationships over time, and capable of therapeutic
discussions.
Slide 8 attempts to capture the pattern matching aspects of
psychiatric practice and why training and experience are necessary. It illustrates how previous exposure to various
diagnostic and therapeutic elements can lead to problem recognition and
resolution.
Slide 11 is an explanation of the current workforce and how
the practice environment has deteriorated over the past 40 years. I emphasized
rationing as the main problem and several audience members were aware of the
shortage of psychiatric beds and state hospital closures. The city of Anoka has one of the few remaining
state hospitals – Anoka Metro Regional Treatment Center. In the future if I am projecting - this slide would be split to 2 separate slides.
The presentation went very well. There was additional interest in the medical and psychiatric effects of the pandemic. Several audience members were interested in my opinions about the Department of Human Services in Minnesota and how they factor into the current rationed system of care. I am currently expanding some of the graphics in case there is any additional interest and as an outline for some of my other writing.
George Dawson, MD, DFAPA