I had this idea about how to present the complexity of the psychiatric diagnostic and treatment process. After putting up a couple of diagrams for comment, I went ahead with a PowerPoint. For about 15 years I taught a course in how not to mistake a medical diagnosis for a psychiatric diagnosis. My audience at the time was 3rd and 4th year medical students. The lecture included a discussion of the research at the time in pattern matching and pattern completion, heuristics and common biases, Bayesian considerations, and inductive reasoning. It was generally well received but really cannot be appreciated until you are a senior clinician. Over the time since I taught that course there also seems to be a distinct bias toward considering DSM criteria to be the basis for psychiatric diagnosis and decision making – and that is clearly a mistake.
The very first time I really became aware of the importance
of pattern matching occurred when I was a fourth-year medical student. I was on an Infectious Disease rotation and my job was to get the consults for the day, go out and see the
patients we would be rounding on, do my basic compulsive medical student work
up and present the findings and my ideas about the case to the attending
physicians. ID docs are very bright people and like most impressive rotations I
contemplated becoming an ID specialist for a while. My patient that day had spontaneous bacterial
peritonitis and the question for us was: “Do you agree with the diagnosis and
current antibiotic treatment?” I met
with the patient, took a complete history, did a physical exam, reviewed the
hospital course and labs, and had time for a little research. At the time I was
carrying a copy of Phantom Notes for Medicine – basically an outline of
the major medicine text of the day. I looked up the differential
diagnosis. I was also carrying a copy of
Sanford’s guide to antibacterial therapy – the 1982 version and looked
up the recommended antibiotics for peritonitis.
I was all set for rounds at that point.
Both of our ID attendings were very serious physicians.
There was not a lot of banter or joking.
I anticipated presenting all of the dry facts and either getting a brief
agreement, some questioning until I could no longer answer, or a long discussion
of the diagnosis and treatment. In this
case the attending came into the patient’s room. He was 15 feet away from the
patient and he said: “What am I seeing from right here that is a potential
problem?” Our team consisting of the ID
fellow, two Internal Medicine residents, and myself – stopped in our
tracks. Nobody had an answer. Weren’t we here for peritonitis? How can you diagnose that from across the
room?
“What is wrong with the patient’s shin?” Dr. R stated
looking as serious as usual. Sure enough
there was a light pink confluent rash covering about 10 square inches of the
patient’s left shin area. Dr. R happened to be an expert in streptococcal
infections. He rattled off the type of strep he expected and suggested that we
get a culture and send it to his lab for confirmation. I completed my
presentation. The primary diagnosis and
treatment by the medicine team did not change, but now there was a new
diagnosis and treatment that depended on Dr. R’s ability to recognize the
pattern of this rash and make a rapid diagnosis – even though he was not
expecting it. But beyond that – we all
saw the rash (although we had to be prompted to see it). Dr. R not only saw
it, he processed it as a unique rash, and then a rash most likely caused by a
specific kind of streptococcal bacteria. And over the next several days he was
proven correct by the culture result.
Pattern matching and pattern completion are critical skills
acquired by clinicians over the course of their training and careers that
allows for not only more rapid diagnosis and treatment but also more accuracy
in classifying ambiguous cases. Some of the examples I used in my course
included ophthalmologists compared with primary care physicians diagnosing
diabetic retinopathy and dermatologists compared with primary care physicians
across a series of rashes. In both cases
the specialists had a higher degree of accuracy and were better at diagnosing ambiguous cases.
Cognitive neuroscience encompasses a broad range of
perceptual studies starting with the early studies of visual processing by
Hubel and Wiesel to more recent studies that look at the encoding that occurs
in perceptual systems and what level of processing occurs at the level of
primary sensory and association cortices, what the higher-level cortical structures
may be, and whether or not top down processing influences perception. According
to Superior Pattern Processing (SPP) theory (3), both perceived and mentally
constructed patterns are processed by encoding and integration and at
that point can be used for decision making or transferring approximations to
other individuals. In my example, Dr. R
not only sees the pattern of the rash, but it is integrated into a feature set
that has a time, visuospatial, social, and emotional context that makes it more
likely that he will make a correct diagnosis. Experimental data suggests that
he is not seeing the rash like any other person in the room – largely as a function
of top-down control of his perceptual process. The actual transfer of this pattern to his
junior colleagues is limited because they see the rash as being a universal
truth – that is they just “missed it” and therefore need to memorize what this
rash looks like and not let it happen again.
They are also unaware of the processes involved in pattern matching or
processing or they might have asked him about it. For example, a logical question would have
been: “What features of this rash do you notice that are suggestive of strep or
a specific kind of strep?”
The question of what represents a pattern is critical to
the idea of pattern recognition and processing.
There is a natural tendency to associate the term with visual or
auditory stimuli, but without too much imagining patterns can clearly exist in
any sensory modality and often involves the integration of multiple sensory
inputs. Cortical organization generally
reflects primary sensory input to the cortex with adjacent sensory association
areas and further information flow to heteromodal areas in the frontal and
temporal cortex where additional integration occurs. Patterns can be sensed,
encoded, recognized encoded and processed across theses systems. The resulting integration yields a very
complex array of patterns that are not intuitive. For example, Mattson suggests that pattern processing
in the human brain forms the basis of human intellect including problem
solving, language and abstract thought and that it includes fabricated
patterns. Those fabricated patterns
allow vicarious problems solving without having to conduct real world
experiments. The recent cognitive
neuroscience of pattern processing is a significant advance compared with the
old diagnostic paradigms I taught 20 years ago.
Those old experiments were basically a comparison of a non-expert to an
expert diagnostician focused on a relatively basic clinical problem like a
pathology slide, x-ray, ECG, or physical finding and the results were not a
surprise – the experts typically prevailed in both accuracy and speed. The sheer amount of information in a clinical
encounter looks at what is essentially an infinite array of patterns, including patterns
that are generally not even mentioned as being clinically relevant.
In considering what kind of patterns that need to be
recognized and processed by a psychiatrist – the patterns that exist in clinical
practice are a starting point. These
patterns and the associated phenomenology have been grossly oversimplified by
an overemphasis on nosology. I talk with far too many people who see
psychiatric diagnoses as phrases on a page in the DSM. I cringe when I hear: “The
patient does or does not meet criteria for (DSM diagnosis x)”. Kendler was correct when he referred to the
DSM approach as an indexing system. It
gets people into the same ballpark, but it is not be very useful for predicting
response to treatment or that specific person’s response to being ill. It is also based on a fraction of the information
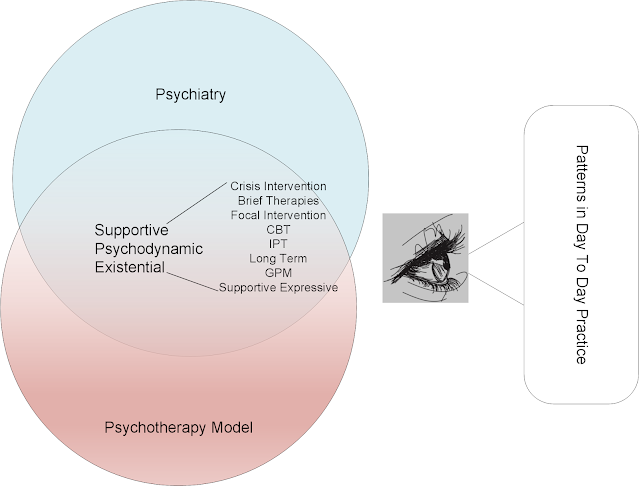
collected in a psychiatric evaluation. When I consider the feature sets that
psychiatrists are considering in evaluations it may look something the graphic below. Of course, these features sets are simplified
for the purpose of making a useful graphic. They will vary with the individual,
their experience, social context, and culture. They will also be blended across
space and have their own individual levels of integration and patterning. Let me provide a couple of examples to
illustrate these points.
Consider the above diagram as representing the possible features that must be recognized in order to assess a patient presenting to a psychiatrist and formulating and optimal diagnostic and treatment plan. My overriding concern in the first few minutes of the evaluation is whether this person really has a psychiatric disorder or a misdiagnosed medical problem and as a corollary - are they medically stable? That sounds like a basic consideration but prioritizing it is not listed anywhere in the DSM or any medical text that I know about. It does involve rapid recognition of patterns of acute medical illness particularly the most likely patterns to be misdiagnosed as psychiatric disorders and what I am seeing in real time. It also involves pattern recognition of the thousands of psychiatric presentations that I have see that were really medical disorders. Real life examples have included an almost immediate recognition that the patient had a stroke (many cases), seizures (many cases), meningitis, encephalitis, cerebral edema, serotonin syndrome, and neuroleptic malignant syndrome. These rapid diagnoses were all predicated on experience-based pattern recognition rather than written criteria and these diagnoses had nothing to do with the DSM at the time.
A more cross-cutting feature in the diagram would be transference issues and defenses that can arise as soon as the initial evaluation or be indirectly evident by the patients historical description of their relationships with important people in their life. These patterns will involve several layers in the above diagram and most importantly may suggest a psychotherapeutic intervention that can be implemented as early as the original assessment. A similar process occurs if the patient is describing features of a major medication responsive illness. In that situation, features from multiple layers result in a pattern that may be recognizable to the psychiatrist in terms of specific medical treatments or the urgency of those treatments.
And finally - what might the graphical representations of these pattern matching processes be? Here are a few examples. In the case of psychotherapeutic examples, it will depend on the exposure to specific therapies in training and practice. Each therapy has a specific pattern or series of patterns that the therapy depends up as well as patterns more specific to the conduct of therapy. These graphics contain critical books from my library shelves with those elements. In the case of the diagnostic and treatment process - the school of therapy and potential application are important patterns to recognize in the initial assessment.
I will resist making this first post of the New Year too
long and wrap it up at this point with a diagram that I think pulls it all
together (see below). Each layer of this diagram consists of patterns and all of the
associated pattern processing that leads to psychiatric diagnosis, formulation
and treatment. A few of the key features include the fact that diagnosis
and treatment are interchangeable processes. There will be times even
during the initial information gathering that a verbal treatment intervention
needs to occur and the entire interview occurs in the context of empathy and
what Ghaemi, et al (4) have described as an existential psychotherapy based encounter
– even if the administrative focus is on pharmacology. A second feature is
that the information exchange is necessarily large if the psychiatrist and the
patient are capable of it. There has been no research that I am aware of on the
optimal amount of information that is required, but there are many
limitations. The advent of the electronic
health record for example has led to the universal use of templates that are
very restrictive in terms of information, typically dichotomous responses. A
third implicit feature is the concept of patterns, what they imply for
diagnosis and decision making and how there is almost a complete lack of
discussion about this process in an era where diagnoses seem to have collapsed
to a brief list of bullet points. Cognitive
neuroscience is a critical area of research focused these processes that I first
became aware of when reading Kandel’s book “The Age of Insight” (5). It is an area that does not typically get a
lot of attention from psychiatrists, but it is a logical extension of the work
done by behavioral neurologists from 20 years ago. If we really want to focus on how psychiatrists
think about diagnosis and treatment – we need to study this field, especially
as the experiments get more complex.
I will wrap up this post at this point with the hope that
2021 is a much better year and that mankind is able to put this pandemic virus
behind us by the summer and approach future pandemics with more science and
wisdom.
Happy New Year!
George Dawson, MD, DFAPA
References:
1: Constantine-Paton
M. Pioneers of cortical plasticity: six classic papers by Wiesel and Hubel. J
Neurophysiol. 2008 Jun;99(6):2741-4. doi: 10.1152/jn.00061.2008. Epub 2008 Jan
23. PMID: 18216235.
2: Poirier CC, De Volder AG, Tranduy D, Scheiber C. Neural
changes in the ventral and dorsal visual streams during pattern recognition
learning. Neurobiol Learn Mem. 2006 Jan;85(1):36-43. doi:
10.1016/j.nlm.2005.08.006. Epub 2005 Sep 22. PMID: 16183306.
3: Mattson MP.
Superior pattern processing is the essence of the evolved human brain. Front
Neurosci. 2014 Aug 22;8:265. doi: 10.3389/fnins.2014.00265. PMID: 25202234;
PMCID: PMC4141622.
4: Ghaemi SN, Glick ID, Ellison JM. A Commentary on
Existential Psychopharmacologic Clinical Practice: Advocating a Humanistic
Approach to the "Med Check". J Clin Psychiatry. 2018 Apr
24;79(4):18ac12177. doi: 10.4088/JCP.18ac12177. PMID: 29701934.
5: Kandel ER. The Age of Insight. Random House, New York,
2012.
Graphics:
All generated by me for a PowerPoint presentation by the same name. The photo at the top are two pamphlets that I carried as a med student along with a copy of Phantom Notes. I was carrying them when I was in the room with Dr. R as he made the diagnosis described above. I would not trade my medical school experience for anything.