Thursday, February 22, 2018
The NYTimes Editorial On Why Mental Health Can't Stop Mass Shooters -What's Wrong With It?
There was a New York Times editorial titled "The Mental Health System Can't Stop Mass Shooters" dated February 20, 2018. It was written by Amy Barnhorst, MD, a psychiatrist and vice chairwoman of community psychiatry for University of California, Davis. Since it popped up it is being posted to Twitter by more and more psychiatrists. It does contain a lot of accuracy and realism about the issue of assessing people acutely and whether or not they can be legally held on the basis of their dangerous behavior. Dr. Barnhorst gives examples of people who allegedly make threats and then deny them. She discusses the legal standard for commitment and its subjective interpretation. For example, even though a statute seems to have a clear standard they are many scenarios in the grey zone, where a decision could be made to err on the safe side. That involves hospitalizing the patient against his or her will because the risk is there and their behavior cannot be predicted. If hospitalized, she anticipates the outcome when the patient appears in front of a hearing officer and gets released. That last scenario is very real and I would guess that the majority of decisions on the front end in these cases take into account what might happen in court.
If the hypothetical patient did get committed he would not be able to acquire a gun with a functional background check system. That system does not currently exist. If guns were involved in his case before hospitalization, the police may have confiscated them. Unless his legal status changes they may give him the guns back. In some cases the patient is told to ask their psychiatrist to write a letter to get their guns back. I am not aware of any psychiatrist who has done that. The FBI NICS system lists all of the conditions that would prohibit a point of purchase gun sale (assuming a check is done). That list includes: "A person adjudicated mental defective or involuntarily committed to a mental institution or incompetent to handle own affairs, including dispositions to criminal charges of found not guilty by reason of insanity or found incompetent to stand trial." Various crimes including domestic abuse can also trigger a failure of the NICS check and when that happens the gun sale is cancelled. Unfortunately not all states participate in this check system and there are numerous exceptions if they do.
I have diagrammed the various levels of arguments that apply to a psychiatrist doing a crisis evaluation on a person brought to the emergency department for making threats with firearms. At the political level there is no nuance. At this level the degree of distortion is the greatest. The usual arguments about guns not killing people is a good example, but it extends even this morning to President Trump suggesting that more mental health resources will solve the mass shooting problem, when it clearly will not. The legal arguments are slightly more informed, but still fairly crude. Like most legal arguments they threaten or reassure. For example, most psychiatric crisis statutes hold harmless anyone who reports a suicidal or aggressive person to the authorities. On the other hand, if a psychiatrist places a person on a legal hold because they are potentially dangerous - it is typically illegal for that same psychiatrist to extend the hold if the court system has not done anything by the time it expires. The civil commitment system has a way of starting to make decisions based on available resources and in many cases the statutes seem reinterpreted that way.
At the medical level, psychiatrists are left living with the legal and political arguments no matter how biased they may be and trying to come up with a plan to contain and treat the aggression. It is not an easy task given the resource allocation to psychiatry - but after doing ti for 20 years - it is fairly obvious that acute care psychiatrists know what they are doing. They are successful at stopping violence acutely and on a long term basis. Given the legal biases they cannot do it alone. There needs to be cooperation from the courts and the legal system and some patients should be treated in the legal rather than the mental health system.
Getting back to Dr. Barnhorst's article one sentence that I disagreed completely with was:
"The reason the mental health system fails to prevent mass shootings is that mental illness is rarely the cause of such violence."
She cites "angry young men who harbor violent fantasies" as basically being incurable. The problem with mental illness and gun violence is that it is dealt with at a political level rather than a medical and diagnostic one. The facts are seldom considered. There are political factions that see violence as stigmatizing the mentally ill and political factions who want to scapegoat the mentally ill and take the heat off the gun advocates. The reality is that people with severe mental illness are overrepresented in acts of violence compared with the nonmentally ill population. It is a small but significant number. In studies of mass homicides the number increases but it depends on the methodology. There are for example school shooter databases that record events as anytime a firearm is discharged in a school. That results in a very large number of weapon discharges but most where nobody is injured. There are databases that just list events but there is no analysis of whether mental illness was a factor or not. In mass shootings in half the cases the shooter is killed or suicides. Even when the shooter survives the data is affected by the subsequent hearings - so there is rarely a pure diagnostic interview available. The data analysis depends on making sure that both the events and the mental health diagnoses are as accurate as possible.
The most parsimonious assessment of this data was published by Michael Stone, MD in 2015 (1). The paper is fairly exhaustive and I am not going to discuss the obvious pluses and minuses. I do see it as a break from the usual sensational headlines and the analysis of the trends in mass homicide over time, especially associated with semiautomatic firearms - leaves no doubt that this is a large problem.
He identifies 235 mass murderers, and estimates that 46 (22%) of them were mentally ill. His definition of mentally ill as essentially being psychotic. He goes on to say that in the remaining fraction and additional 48 had paranoid personality disorder, 11 were depressed, and 2 had autism spectrum disorders. In other words another 26% of the sample had significant mental disorders that were not considered in the analysis because he did not consider them to be psychotic. Another 45 (19%) has either antisocial personality disorder or psychopathic personality disorder - both mental conditions associated with criminal activity and thought to have no known methods of treatment. Using this conservative methodology - it is apparent that mental illness in this population is not rare at all. What should not be lost is that although mass shootings are very noticeable events - they are rare and therefore any overrepresentation of mental illness in this group, is diluted by what happens across the entire population where the majority of violent activity is associated with people having no mental illness and the overall trends in violent crimes are at a 20 year low.
My proposed solutions to the problem of semiautomatic weapon access and mass shooters/murders is approached this way:
1. Increase the purchase age to 21 years. Eliminate access to military style weapons.
2. All purchases must be cleared through the NICS system. All states must participate. Currently only 12 states participate in full point of contact background checks on every gun sale.
3. The NICS system should include terroristic threats, stalking, and any gun confiscation by the police because of mental health grounds as exclusion criteria. In other words, you are eliminated from gun purchases if you have been reported for these problems. That may sound a bit stringent but I think there is precedent. You cannot make threats about air travel at an airport. If you have been charged with domestic abuse (Misdemeanor Crimes of Domestic Violence (MCDV)
the are special instructions on what it takes to keep firearms from you. I consider the safety of children in schools to be on par with these two cases (air travel and domestic violence threats).
4. At the level of law enforcement, any firearms confiscated during a threat investigation should not be returned and that person should be investigated and reported to NICS Database.
5. Uniform protocols need to be in place for terroristic threat assessment. It is no longer acceptable to wait for a person to commit an act of aggression before there is a law enforcement intervention. The person making the threat should be removed from that environment and contained pending further investigation.
6. On the mental health side - rebuilding the infrastructure to adequately deal with this problem is a start. Hospitals with large enough mental health capacity should have a unit to deal with aggression and violence. There should be specialty units that collect outcome data on the diagnoses represented and work on improving those outcomes.
7. On the law enforcement/corrections side there needs to be recognition that not all mental health problems can be treated like mental health problems. Violent people with antisocial personality disorder and psychopathy are best treated in law enforcement setting and not in psychiatric settings. In psychiatric setting they have a tendency to exploit and intimidate the other patients in those settings as well as the staff. They should be treated by psychiatrist with expertise in these conditions and been seen in correctional settings. Probation and parole contingencies may be the best approach but I am open to any references that suggest otherwise.
8. In the early years of this blog - I was an advocate for violence prevention and I still am. Violence and aggression have the most stigmatizing effects of any mental health symptoms. I think it is safe to day that most psychiatrists actively avoid practicing in setting where they may have contact with aggressive patients. It needs to be seen as a public health problem and education and prevention are a first step.
Those are my ideas this morning. I may add more to this page later. If you have a real interest in this topic Dr. Stone's paper is a compelling read. If I find others of similar quality I will post them here. Don't hesitate to send me a reference if you have one.
The bottom line is that no psychiatrist can operate in the current vacuum of realistic options and hope to contain a potential mass shooter. And yet there is a clear overepresentation of mental illness in this population. Some level of cooperation as suggested above will result in a much tighter system for addressing this issue. We do it in airports and in domestic violence situations. We can also apply more uniform and stringent expectations to schools.
George Dawson, MD, DFAPA
References:
1: Amy Barnhorst. The Mental Health System Can't Stop Mass Shooters. New York Times February 20, 2018. Full Text Link
2: Stone MH. Mass Murder, Mental Illness, and Men. Violence and Gender. Mar 2015: 51-86. Free Full Text Link
Graphics Credit:
Photo of the M4 Assault Rifle is per Shutterstock and licensed through their agreement.
Layered arguments graphic was done by me in Visio.
Saturday, February 17, 2018
Drug Marketing In The Post Psychiatric Apocalypse
I saw this drug marketing ad from Johnson and Johnson posted on Twitter today. Johnson & Johnson is marketing their sustained release version of paliperidone called Sustenna as a way to keep people with schizophrenia out of jail! I have not been able to find an updated package insert from the FDA at this point but this is from a release on the J&J web site as an indication for the drug.
"The time to first psychiatric hospitalization or arrest and/or incarceration was significantly longer for people treated with INVEGA SUSTENNA® versus these same commonly prescribed oral antipsychotics."
I have been posting here for years about the fact that health care businesses and governments have actively worked together to eliminate psychiatric and mental health resources. That is just a proven fact. I have posted that psychiatrists have been taken out of the loop so that these same politicians and business leaders can accomplish these goals. I have posted that the resulting pricing strategies divert any existing resources away from physicians and patients and into the pockets of the managed care, pharmaceutical benefit manager industry, and pharmaceutical companies leaving some patients with very little to live on. I have posted about how psychiatric beds have been rationed until they are practically non-existent and the admission and discharge criteria altered so that very little treatment occurs there. And as a final result, I have documented the widespread diversion of patients with severe psychiatric problems to jails. The largest psychiatric hospitals in the USA are county jails. I have pointed out how there is a tendency to blame psychiatrists for the mythical shortage of their own specialty and mental health services when any real shortage was planned that way by the same people who have rationed mental health services to the bone.
There are probably just a few people (usually psychiatrists and the families of patients) who know about what happens when the bar is lowered from hospital admissions to arrests and incarcerations. I have observed first hand what occurs. The risk to the patient increases exponentially. Every time there is a confrontation between the police and a mentally ill person the odds are greater that there will be misunderstanding, injury, and possibly death. I have received many of these beaten up people on my inpatient service when they were brought to the hospital and admitted because they were obviously mentally ill. The only reason they were brought to the hospital was because of the physical injury. Otherwise they were on their way to jail. Once in jail they can get no care or very little care. It is common that people with mental disorders or addictions are taken off of their usual medications. They do not receive them in jail most of the time and that can impair their ability to cooperate with law enforcement or work with an attorney to get released.
So jail has become a treatment endpoint on par with hospitalization. Somebody somewhere must have a number that shows it is much more likely that a person with a serious mental disorder ends up in jail rather than a psychiatric hospital. I could suggest a number of surrogate endpoints for the next study. Number of people dead on the street. Number of people dead because they did not get their insulin or needed medical care for heart or lung disease. The possibilities become numerous when humane treatment in a safe medical setting drops farther down the list.
There are probably just a few people (usually psychiatrists and the families of patients) who know about what happens when the bar is lowered from hospital admissions to arrests and incarcerations. I have observed first hand what occurs. The risk to the patient increases exponentially. Every time there is a confrontation between the police and a mentally ill person the odds are greater that there will be misunderstanding, injury, and possibly death. I have received many of these beaten up people on my inpatient service when they were brought to the hospital and admitted because they were obviously mentally ill. The only reason they were brought to the hospital was because of the physical injury. Otherwise they were on their way to jail. Once in jail they can get no care or very little care. It is common that people with mental disorders or addictions are taken off of their usual medications. They do not receive them in jail most of the time and that can impair their ability to cooperate with law enforcement or work with an attorney to get released.
So jail has become a treatment endpoint on par with hospitalization. Somebody somewhere must have a number that shows it is much more likely that a person with a serious mental disorder ends up in jail rather than a psychiatric hospital. I could suggest a number of surrogate endpoints for the next study. Number of people dead on the street. Number of people dead because they did not get their insulin or needed medical care for heart or lung disease. The possibilities become numerous when humane treatment in a safe medical setting drops farther down the list.
This ad and study as well as the FDA approval marks a new low water mark in psychiatric care in the USA. I think we can safely say that we are now in a post psychiatric era of care. An era where the quality measure is keeping patients out of a place that they should never have been put in the first place - the county jail. The is a palpable new low in the nonsystem of care for the mentally ill. That new low has been endorsed by a federal agency - the FDA and a pharmaceutical company. It will probably result in other pharmaceutical companies trying to get the same indication.
At this point there is no doubt that businessmen and politicians have a stranglehold on psychiatric care. It has morphed into a landscape that is unrecognizable to this psychiatrist.
God save our patients and God save us all.
George Dawson, MD, DFAPA
Supplementary: I intentionally kept this brief. I have thoroughly covered all of this on the blog. I just wanted to clearly mark this dark day.
Friday, February 16, 2018
Jeff Bezos Hear My Plea
My latest excursion into direct-to-consumer lab testing concluded about an hour ago (2:30 PM) and it was an unequivocal bust. I wanted to check three different endocrine parameters that I thought might be important for asthma control - so I went online looking for a way to do that. I am not a novice in the area. About 10 years ago I found a local health care system that offered a limited menu of direct to consumer testing. In other words, you just walk into the lab, check off what labs you want, pay them, and they do the tests. No calls to a doctors office and the endless telephone queues, no discussions with staff who treat you like you are a demanding patient, no waiting for a call back from the doctor, and no waiting for the staff person to talk with the doctor and then call you back. That is exhausting and a clear impediment to medical care. The electronic health record (EHR) "fixes" for this problem are not much better. I find myself either looking at a list of fairly simple lab tests and visits or signing off on a possible $45 fee for an email if I have not seen the doctor within a certain interval. That is equally exhausting, especially when I end up clicking on "other" and typing an essay on what I really want.
About 10 years ago, the first direct to consumer labs became available in the Twin Cites - a metro area of just over 3 million people. There was a very limited menu, but I found it useful to follow Vitamin D levels and discovered that my wife probably did not need to take Vitamin D. I occasionally checked a few other tests - maybe a total of 5 times in the 10 years. This time I needed more esoteric tests than were on the list and hoped there was another lab. I did find it but there were several problems. The first was test selection and payment. It suggested that I do it online, collect all of my tests in a cart and check out. When I did that I discovered that the company collecting my credit card information was not the lab, but some other company I had never heard of. Was it safe to give them that information? There was an online chat staff - but she just gave me an 800 number to confirm the company was who they said they were. I shut it down at that point.
The next step was calling the nearest lab about 9 miles away. I called several times and left my number. Nobody bothered to call me back. I finally decided to just drive down there. They were located in an industrial strip mall - nothing unusual for durable medical goods companies. I walked into a packed waiting room of about 20 people. There was a reception window that was never inhabited during the 90 minutes I was there. Any new customer needed to figure out that they needed to enter their name, birth date, and phone number on an electronic tablet in order to get into the queue. A phlebotomist came out every 5-10 minutes to call the next customer. The place had an industrial feel - not unlike an old hospital past its prime. It seemed like everyone else was bringing in paper work. My expectation was that it ran like the other place. Just check off the boxes, pay, and get the blood drawn. The real conversation went something like this:
Phlebotomist: "Do you have any paper work?"
Me: "No I thought from the web site that I could just tell you what I want and pay here."
Phlebotomist: "No - here you need a doctor's order or an account."
Me: "Well I am a doctor can I just give you the order?"
Phlebotomist: "Do you have a prescription pad?"
Me: "No I thought I could just check a form and pay you."
Phlebotomist: "No we can't take any payments here - you have to pay online."
Me: "OK - sorry for wasting your time."
Phlebotomist: "You're not wasting my time. I'm here until 4 o'clock."
It was a total wash. No lab test and about 2 1/2 hours wasted.
This is where a company like Amazon can really revolutionize health care. Healthcare companies are doing everything they can to monopolize lab and imaging services. They have oversold the EHR to patients like everybody else. I have argued with some of these unfortunate souls that believe the EHR is really going to help them maintain their own private healthcare information and portability. My description above indicates otherwise. I also ask them if they still have any healthcare information that they stored on a computer in the 1990s.
The news about Amazon, Berkshire Hathaway and JP Morgan news about their healthcare initiative has fueled a lot of speculation about how that will play out. My speculation is that Amazon has the current data handling infrastructure to aggregate healthcare just like they aggregate everything else. The question is what will be aggregated, how will it be aggregated, and what will the regulatory burden be on the aggregation. Consumers are now considering their personal healthcare information to be their own property. That is not how the laws are written, but it is a selling point for health care products. If Jeff Bezos is listening, the low hanging fruit in health care are high margin lab tests, imaging studies, and medications. Those are the best products to aggregate based on price comparisons and how easily they are available. On the back end, there is the question of getting the results to the attending physician and the medicolegal implications of giving abnormal results back to a patient with no commentary. In Minnesota, the first company I used here got around that by saying that any abnormal tests were run by the laboratory pathologist for comment.
As a physician and consumer, this is the revolution that is necessary. Many people are perfectly capable of getting maintenance labs or labs of interest when necessary and call their doctor about the results. They are less likely to keep coming in and seeing a doctor for the sake of routine labs and lab interpretations. They are less likely to go to traditional hospital and clinics that adhere to inconvenient hours. This approach would shift some of the cost to the consumer, but the trade off would much better cost and convenience. An example is the three endocrine tests I was ready to order cost about $230 and they have been available for decades. For the same price, I can get my entire genome analyzed. Lab margin estimates in the news are 10-20%, but I would guess that is on the low side.
All of the current major Internet companies are capable of these changes. They should also be very competent in producing a much better EHR that works for physicians. I think that health care regulation and business models are what has been holding them up. Hopefully Amazon's move will get the rest of them involved and move health care management and funding as far away from the insurance industry and pharmaceutical benefit managers as possible.
I may still end up walking into an industrial strip mall lab to get my blood tests done - but at least I would know that everything on the front end would have been handled flawlessly and my credit card will take less of a hit.
George Dawson, MD, DFAPA
Graphics Credit:
The Amazon sign was downloaded as an image from Shutterstock per their licensing agreement. I have no connection with Amazon and am not a stockholder. I have no conflict of interest to declare in this area.
Monday, February 12, 2018
Sedating Patients For Imaging Studies
An article in this week's JAMA hit me like I was still on my old inpatient job. It was about the issue of sedating patients for imaging studies. Quality brain imaging - whether it is an MRI or a CT scan depends on the patient being able to lie very still. Any movement causes artifact that can obscure critical brain areas of interest. The reasons for the agitation vary quite a bit based on the population but the agitation is not necessarily any easier to treat. The setting is often different.
As an example, agitated patients on our neurology service when I was an intern were typically agitated due to brain disease. One of the first patients I saw was elderly and extremely agitated. Delirium or psychiatric illness was suspected because of examination limitations. When I examined the patient in the emergency department (ED) - and did the otoscopic exam - there was a large amount of pus coming out of the left ear. Subsequent lumbar puncture showed that the diagnosis was pneumococcal meningitis. Like all agitated neurology patients, the chief resident came by and administered intravenous fentanyl. The junior resident and I stood by next to the CT scanner in the event the patient became excessively sedated or apneic because of the fentanyl. Without it the CT scan would have been impossible. She was subsequently admitted to the ICU and had a very complicated course, but eventually survived and left the hospital.
On the psychiatric side. things are a little bit different. The indications for brain imaging are all based on psychiatric diagnoses. The medical status of the patient may be completely unknown, based on their ability to cooperative with a review of systems and physical examination. In most inpatient psychiatry settings these days the patient has come through the emergency department but the complete diagnostic evaluation is deferred to the inpatient side. Assessment by the inpatient staff the next day may indicate that brain imaging is needed. The ability to cooperate may vary from an inability to sit still to overt aggression based on the illness. It is a common occurrence to get a request from radiology to sedate the patient before they go for a brain imaging study.
The issue from an inpatient psychiatric unit is several fold. Many of the patients are very vigorous and have no physical illnesses. The medications used on psychiatric units are not anesthetic agents and they do not work immediately. Psychiatric units are rarely staffed at a level that several physicians can accompany the patient and give them an agent that would work immediately. Even if they could - the question would be qualifications to supervise that process. At the minimum, they would need to be qualified to administer that agent and manage a cardiopulmonary arrest. Finally, there is the hospital wide issue of how much support can psychiatry count on. Can psychiatry for example request an anesthesiology consult for the purpose of imaging study sedation?
In the case report, an elderly man with a BMI of 39 and an history of stable coronary artery disease presented to the ED with dizziness. He ahd associated hypertension, hyperlipidemia, history of carotid endarterectomy, and obstructive sleep apnea (OSA). He was treated symptomatically with meclizine and ondansetron but a neurology consultant recommended an MRI scan of the brain. He was not able to tolerate the close confines of the MRI scan and was given 1 mg of lorazepam for anxiety reduction. Over a period of about 15 minutes in the MRI scanner he became incoherent and eventually unresponsive and a cardiac arrest code was called.
The article reviews the errors made in this case beginning with the administration of lorazepam. Lorazepam is commonly used on inpatient psychiatric units for detoxification, agitation, and insomnia. The exact dose in this case is a dose that I have administered many times to patients who were going for imaging studies and it is frequently not enough for that purpose. In this case the patient has OSA and risk factors such as increased age that place him at higher risk for complications. In this case the authors suggest the minimal dose and if more is needed to monitor heart rate, pulse oximetry and blood pressure in high risk patients. I would typically do that by requesting an anesthesiology consult for the purpose of sedating the patient for an MRI scan.
Associated measures of care in this situation include equipment availability. They recommend the availability of a fiberoptic bronchoscope in case the patient needs immediate intubation and the intubation is difficult. They consider it to be a priority in the case of patients who have risk factors for airway loss after sedation.
The American Association of Anesthesiologists has designated dexmedetomidine as a sedative that does not compromise the cardiorespiratory status of patients. It is a alpha-2 adrenoreceptor agonist. I did a search on psychiatric applications of dexmedetomidine and the results of that search can be found here. The package insert discusses the limited applications of ICU intubation and sedation of non-intubated patients for procedures.
Communicating the patient's OSA status was also viewed as a key error correction process. OSA is a highly prevalent condition making it more likely that patients with this condition will be sedated for MRI scans. The suggest including an OSA section in the MRI checklist.
When I think about how this procedure has been done over the course of my career - it was hardly standardized and apart from my neurology team monitoring critically ill neurology patients inside a CT scanner - little monitoring was done. About 15 years ago that landscape started to change. Suddenly anesthesiology consults were much easier to get and much more successful. That was a great relief compared to a process when additional medications were being requested and nobody was there to monitor the patient. In a few cases, I called off the scan until adequate monitoring could be established.
The precautions noted in this case report should be studied by every psychiatrist who finds themselves ordering sedation for MRI scans or other procedures. It is entirely possible that MRI technology may be available in some hospitals but not the appropriate monitoring staff.
In that case I would recommend forgoing the procedure if all of the recommended staff and equipment is not available.
George Dawson, MD, DFAPA
Reference:
1: Blay E Jr, Barnard C, Bilimoria KY. Oversedation of a Patient With Obstructive Sleep Apnea Prior to Imaging. JAMA. 2018 Feb 6;319(5):495-496. doi: 10.1001/jama.2017.22004. PubMed PMID: 29411034.
Graphics Credit:
MRI Images are from Shutterstock per their standard licensing agreement,
Sunday, February 11, 2018
The Problem of the Drinking Spouse
Any physician treating alcoholism knows this scenario very well. You have finally convinced a person that they have a problem with alcohol. They have been in treatment and either using or not using MAT (medication assisted treatment - naltrexone or acamprosate). They are at the point where they are abstinent many more days than they are drinking. This is a critical point for many people who are daily drinkers. As you work with them in trying to define critical factors for continued use they identify: "My husband/wife refuses to stop drinking. They say it is my problem. They like drinking and they refuse to stop. They have alcohol at the house."
There are many variations on that theme. Some spouses will keep all of the alcohol locked up and imbibe only when the sober spouse is sleeping. Some will not have any alcohol at all, but continue to drink in social situations accompanied or unaccompanied by the sober spouse. Some will just resent the sober spouse and the sudden restriction in the couple's social life. Many couples start drinking to increase their social activity and expand their social contacts. In many businesses, this level of socialization and the associated drinking is expected. The associated level of emotionality in the marriage can increase precipitously based on the new expectations of the sober spouse about how things should be to support their sobriety. The combination of the environmental cues from alcohol and increased emotionality greatly increase the risk for continued alcohol use and make all of these patterns untenable. Convincing the drinking spouse that their behavior does not facilitate sobriety in the marriage is a difficult task - if it is attempted at all.
Are there any large scale studies that back up those clinical observations? A certain portion of drinking spouses may respond to clear scientific evidence if they cannot respond to the advice of a counselor or physician. It turns out that there are and a lot of that work has been done by Kendler and co-authors.
The most recent paper in JAMA Psychiatry (1) looks at the issue of spousal resemblance for alcohol use disorder. In the study, subjects were obtained from a generational sample of all people born between 1960 and 1990 in Sweden who were married before December 31, 2013. They were identified as having alcohol use disorders (AUD) through several databases that looked at medical diagnoses, medication assisted treatment prescriptions (disulfiram, naltrexone, acamprosate) and convictions or suspicions of at least two alcohol related crimes. That resulted in marital pairs - 5883 where the husband first developed an AUD and 2679 where the wife first developed an AUD. They note that in marital pairs, first onset AUD was much greater in pairs where a spouse had an AUD than when they did not.
They analyzed the data by two methods. First, they looked at hazard ratios of developing an AUD relative to a control group matched by sex, birth year, year or marriage, family history of AUD, and parental educational level. Second, they looked at intraindividual hazard ratios across subsequent marriages and divorces.
In the first analysis, the hazard ratio of AUD in the wife after the husband had an initial AUD was 13.82 dropping to 2.75 over the first two years. In the case of husbands after a wife's first registration of AUD the hazard ratio was 9.21 falling more slowly to 3.09 after 3 years.
In the intraindividual comparisons - for husbands moving from a spouse with no AUD to one with an AUD resulted in a HR of 7.02. Moving from a spouse with an AUD to one without and AUD decreased the risk to a HR of 0.50 for AUD. The protective effects persisted in the same direction in second and third marriages. They produced a comprehensive tables of 20 possible combinations of spouses +/- AUDs and list the protective and predisposing combinations. In each case, whether or not the prospective spouse has an AUD predicts the the probands status.
The authors conclude that this is tentative evidence that a spouses alcohol use status has a causal effect on their spouses drinking. They suggest the likely processes and suggest that assortative mating is a factor in the large increase in drinking that can occur when a man or woman without an AUD marries a man or woman with an AUD. Assortative mating has been previously studied by Kendler (4) and is defined as mate selection that depends on similarity across traits - in this case drinking patterns and risk factors for AUD. It is an interesting concept because it suggests at least part of the mechanism of greatly increased risk in the spouses of drinkers. A non-drinking spouse with those characteristics may have more credibility as a protective effect, but those specifics are not clear at this time.
The limitations are discussed in the original paper and I won't belabor them here. Clearly the study design is an issue. It is likely that cases were missed. I have not seen it studied, by my experience with diagnoses and the American insurance system suggests that many people will do what they can to stay off of a database. I can't imagine that is not also true in Sweden. They did a comparison of the AUD prevalence of their data to Norway and found the prevalence was lower. This methdology also focuses on more severe AUD. I based that on the fact that the DSM-5 committee eliminated legal problems as a diagnostic criteria for AUD based on it not adding much to the criteria because it was associated with most of the other criteria.
An observation about the study. It could not have occurred in the United States - at least not on the same scale. In the US, treatment for alcohol or substance use problems comes under the the auspices of §CFR 42, limiting access to information for research purposes. Advocates for these restrictions will of course say they are necessary and that people can still release information like they can for any other medical condition - but like most of these regulations there is general confusion and intimidation of clinicians to the point that the extra hurdles necessary to do research are seldom breached. In the US, in the case of non-public programs like Medicare or Medicaid, all of the data is aggregated by health care system. In Scandinavian countries all patients are on a single national database. In the Swedish study, the researchers assigned unique serial numbers to all of the subjects and the ethics committee approval waived consent because of this procedure.
This study gets back to a philosophy of life and the issue of sobriety or at least self-correcting abstinence. Couples do have conversations about drinking. They do make conscious decisions about drinking and substance use. They observe one another when they have become too intoxicated and had significant embarrassment or hangover effects. If there are no baseline agreements about the use of intoxicants early in the marriage there should be a discussion about self correcting abstinence. When do we agree to stop whatever we are doing as a couple and reassess our use of intoxicants. Things do not have to get to the level of an actual alcohol or substance use disorder.
Finally, what about the approach to the couple when there is a clearly defined alcohol or substance use problem? The couple's dynamic does need to be identified and addressed. For any physician or counselor approaching the problem is fraught with difficulty. Spouses tend to be defensive, resentful, and in some cases openly hostile to the idea that they need to stop drinking. The drinking spouse may see the physician or counselor as affiliated with the nondrinking spouse and that can amplify the resentment and negative emotion. There are programs with a more neutral response that treats the drinking spouse in an entirely different context and provides the necessary education. Al-Anon is the prototypical self help program for spouses that attempts to address anger, resentment, and provide a focus on positive strategies. I am still waiting to see an explicit manual, pamphlet, or book that is focused on why the drinking spouse needs to stop drinking. If I missed that please send me a link to that resource.
Before you send a comment on the couple where one person is sober and the other person drinks, I can assure you that I am aware that the situation exists. I typically see it where the spouses are independent and often have separate social and recreational outlets. In many cases, one of the spouses works excessively and alcohol use is incorporated into work activities or becomes a ritual on the way home. The situation I hope to address here is one where both spouses are drinking - usually too much and one of them wants to quit.
I have not seen a lot written about the problem or the solution.
George Dawson, MD, DFAPA
References:
1: Kendler KS, Lönn SL, Salvatore J, Sundquist J, Sundquist K. The Origin of Spousal Resemblance for Alcohol Use Disorder. JAMA Psychiatry. 2018 Feb 7. doi:
10.1001/jamapsychiatry.2017.4457. [Epub ahead of print] PubMed PMID: 29417130
Full text available on line. Please read it.
2: Kendler KS, Lönn SL, Salvatore J, Sundquist J, Sundquist K. Effect of Marriageon Risk for Onset of Alcohol Use Disorder: A Longitudinal and Co-Relative Analysis in a Swedish National Sample. Am J Psychiatry. 2016 Sep 1;173(9):911-8. doi: 10.1176/appi.ajp.2016.15111373. Epub 2016 May 16. PubMed PMID: 27180900.
2: Kendler KS, Lönn SL, Salvatore J, Sundquist J, Sundquist K. Effect of Marriageon Risk for Onset of Alcohol Use Disorder: A Longitudinal and Co-Relative Analysis in a Swedish National Sample. Am J Psychiatry. 2016 Sep 1;173(9):911-8. doi: 10.1176/appi.ajp.2016.15111373. Epub 2016 May 16. PubMed PMID: 27180900.
Graphics Credit:
Photo at the top is from Shutterstock per their licensing agreement.
Saturday, February 10, 2018
New Twist On An Old Method To Kill The Flu Virus
Right after posting the previous article on the latest confirmation that influenza virus is airborne, I came across and article in Nature that had me thinking back to my childhood. I remember walking into an insurance office on Main Street in our small town. There was something strange about the environment. Up next to the ceiling were ultraviolet lights. The lights were shielded so that they only reflected up toward the ceiling. I asked my parents what they were and got the answer: "They are there to kill germs." My head was spinning from that answer: "There are germs in the air? They are up next to the ceiling? What kills the germs that are down here next to me?" Yes - I was a neurotic little kid.
Over time I learned a little about the nature of ultraviolet light, especially that it could cause eye damage if you looked right at it. As I got into the 1970s, the hippie era, and psychedelia that because less important. There were UV lights everywhere - blacklight posters and the detergent residues in clothing phosphorescing white light after it has been activated by UV light. In some environments everyone was bathed in UV light.
Today most Americans are aware of UV light because of sunscreen and eyeglass applications. Long and medium wavelength (UVA and UVB) and not absorbed by the ozone layer. It is recommended that glasses block 100% of the UVA and UVB for maximum eye protection. That can also be designated as UV400 because they block all UV light from 280-400 nm. The part of the UV spectrum is also important in sunscreens. UVA penetrates the skin to a deeper level and is responsible for damaging keratinocytes, cataracts and causing premature aging. UVB is responsible for burning and carcinogenesis. UVA and UVB are considered both carcinogenic and carcinogenic. Even those UV light has been known to be germicidal for over 80 years that human toxicity has limited the application.
UVC (100-280 nm) is blocked by the ozone layer and therefore is not a consideration in either eye or skin protection. It is considered to be the part of the spectrum that is potentially germicidal and that is where the latest application begins. In this report the authors used filtered 222-nm light sources in an experiment to see if they could inactivate aerosolized H1N1 influenza virus. They were able to accurately measure the light dose and estimate virus inactivation using an epithelial cell model that measured infected cells by fluorescence. The authors aerosolized the virus into a UV irradiation chamber. The chamber had a total volume of 4.2 liters and had a characteristic particle distribution of 87% < 0.3 - 0.5 μm, 11% 0.5 - 0.7 μm, and 2% > 0.7 μm. Those are characteristic particle distributions of airborne droplets that occur with breathing, talking, and coughing.
An air flow of 12.5 L/min through the chamber was noted and they calculated that this meant a single droplet passed through the chamber in about 20 seconds. I think that is significant because it in unlikely in a typical building that a person would be standing in an air current moving that quickly. In other words, if the aerosolized virus can be inactivated in an airstream moving that quickly - it might have practical applications in most environments. The authors were able to construct a dose response curve showing that at a dose of 2 mJ/cm2 viral survival is negligible.
I found this to be extremely impressive work because it clearly shows that airborne influenza virus can be inactivated using a far-UV source that is much safer to humans than previous germicidal UV sources. Furthermore the sampling and intervention characteristics seem to be very realistic in terms of what might be encountered in public facilities. The real question seem to be whether any commercially available air cleaner/purifiers come close to matching the characteristic of this experiment. A preliminary search of these devices shows that the airflow characteristics are typically not listed, very few use far-UVC light sources (most use germicidal 254-nm sources shielded in the device), and none are certified in terms of how much virus they kill. They typically suggest that germicidal UV light is all that is needed for air purification. There is also the question of whether using a device in your office at work confers any degree of protection once you leave that office and start walking down the hallways. My speculation is that it would not, but the amount of virus generated in your office may be a significant variable.
The authors themselves suggest that if their results are confirmed far-UVC represent a significant opportunity to limit the transmission of airborne disease and that it could be widely used in medical offices and buildings as well as public areas where disease transmission is common like airports and airplanes.
I am hoping that this areas of research yields rapid results and broad implementation.
George Dawson, MD, DFAPA
Reference:
1: David Welch, Manuela Buonanno, Veljko Grilj, Igor Shuryak, Connor Crickmore, Alan W. Bigelow, Gerhard Randers-Pehrson, Gary W. Johnson, David J. Brenner. Far-UVC light: A new tool to control the spread of airborne-mediated microbial diseases. Scientific Reportsvolume 8, Article number: 2752(2018). doi:10.1038/s41598-018-21058-w
Graphics Credit:
Table 1, Figure 1, and Figure 2 are all used from reference 1 per the Creative Commons Attribution 4.0 International License.
Table 1, Figure 1, and Figure 2 are all used from reference 1 per the Creative Commons Attribution 4.0 International License.
Friday, February 9, 2018
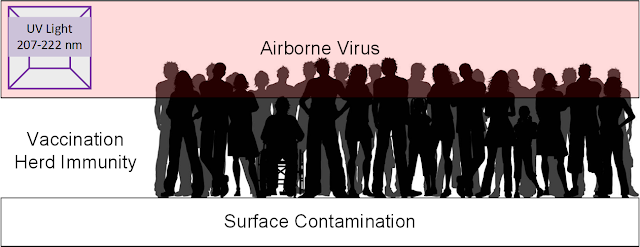
Viruses Are In The Air - Protection From Airborne Viruses
Today was a good day. I got up this morning and there on the morning news was a headline that I had been waiting to hear for at least 20 years. There on CBS This Morning, Gail King was saying: "The flu can spread just by breathing so that is kind of scary." That is kind of scary. It is even scarier if you know that fact and listen to 20 years of how hand washing will prevent the flu. Hand washing is good only for surface contamination. It does nothing for airborne viruses. There is no known protection from airborne viruses other than biohazard environments.
I did not come by the knowledge easily. Before medical school, I was a research assistance in a plant tissue culture lab. Our job was to try to clone Loblolly Pine (Pinus taeda) and Douglas Fir (Pseudotsuga menziesii) trees from elite seed. That required a sterile environment for tissue and media manipulations. I spent much of the day working in a laminar flow hood bathed in sterile air. We were not concerned at all about viruses at the time, but there were always experiments lost due to yeast and fungal contamination of the culture medium. From there it was off to medical school and observations about just how contagious airborne viruses could be. On some rotations the entire team was ill with respiratory infections. I notice there is some movement today on telling physicians to stay home if they are sick. If all of the people who were sick on one of these teams stayed home - there would be nobody there to take care of patients. I did work with one attending physician who wore a surgical mask in a medicine clinic as a barrier to viruses. Today we know that these masks are ineffective in blocking viruses.
The real eye opener came in practice. For over 20 years I worked in an inpatient environment that was designed in the 1960s. According to the HVAC experts I have consulted with, the environments in those days were designed to preserve heat. They were not designed to provide fresh air in a manner that would minimize the risk of airborne virus infections. All of the rooms in that environment had individual radiators equipped with fans. The room air was recirculated. At the top of each room was a 12" x 12" square vent that moved the air down the length of the building to a few air shafts that traveled up and down between floors. I was reassured that there was adequate air flow and that it was measured. I was provided with some diagrams that did not really show any solid data.
In that environment, airborne viral infections ran rampant. They were acute care psychiatric units - so many of the patients directly admitted had influenza. It was just a matter of time before it was picked up by the staff and then transmitted from person to person. Getting one or more of these infections predictably was quite depressing. As anyone knows - a severe case of the flu disrupts your entire life. The polypharmacy that the staff was subjected to was also impressive. Long complicated courses of antibiotics for secondary infections after the flu had passed. Exposure to prednisone and methylprednisolone for post-viral bronchitis and asthma exacerbations. All of the infected staff were schooled in proper handwashing techniques by Infection Control. During flu season we were basically adrift in tight confines - breathing contaminated air. It is well documented by studies in hospital and other building environments that there are a significant amount of viral and other pathogens in the air that can be collected by a number of means (2).
The other enlightening experience involved my participation in two Avian Influenza task forces. Practically all of the work that I saw being done seemed to ignore the issue of airborne spread. That was probably at least in part due to the fact that the hospital capacity of negative air pressure rooms would be immediately overwhelmed. At that point, I heard one expert say: "You need to have an N95 respirator mask on as soon as you walk through the door of the hospital." The efficacy of those masks in preventing flu transmission is limited but probably offers some moral support when you are walking into an environment that is full of highly lethal influenza virus. Most of the planning done on the task forces seemed to be designed to prevent a large surge of patients going to the emergency department, providing psychological support to the overwhelmed, and hoping the military really did have that palette full of Tamiflu that they keep showing us in the PowerPoint presentations.
One of the questions I frequently get is - what about the vaccine? Designing an effective flu vaccine is part science and part speculation. It involves anticipating the viral strains of the next epidemic and that is difficult to know with certainty. This is the first year that I can recall public health officials coming out with the actual numbers. Most Americans have heard that this years vaccine is about 30% effective and that the most effective vaccines are 50-60% effective. The argument is that the vaccine improves herd immunity and decreases the spread of the virus. Exactly how much of that is cancelled out by broad exposure to an airborne virus is unknown, but I do think that is sufficient reason to always get the vaccination. I was my own experiment for about 30 years. I reacted to an anti-rabies duck embryo vaccine in my 20s and did not get the vaccine for the subsequent years. I finally saw an allergist/immunologist about 7 years ago and have been getting the vaccine since. Since then there has been no detectable change in the number or intensity of flu-like illnesses that I have developed. During the time unvaccinated, I had the experience of developing an acute fever after being exposed to a colleague with the flu, taking Tamiflu (oseltamivir) and having the symptoms resolve within 24 hours. There is a chance that a universal flu vaccine can be designed and I hope that is true. In the meantime we are left dealing a number of airborne viruses and altering the environment seems like the best approach.
Flashing forward to this morning. Part of the story focused on Donald K. Milton and the work he did in designing a machine to sample flu viruses in a natural setting. Other sampling techniques have typically involved subjects breathing according to protocol into a device. The large reverse megaphone type of device that this group is using allows air flow past the face at a regular rate. It allows research subjects to breath normally and sample their expired air for influenza virus. The sample in this case was a group of healthy 19-21 year old college students with a high asthma prevalence (21%) and a low influenza vaccination rate. Nasopharyngeal (NP) sampling and RNA detection was used to diagnose influenza and RNA copies.
The subjects were asked to breathe, talk, cough, and sneeze into the sampling device with no constraints on that activity. They were asked to recite the alphabet at 5, 15, and 25 minutes. Coarse droplets (> 5 μm ) and fine droplets (≤ 5 μm and >0.05 μm) were collected separately. Influenza virus was recovered from 89% (N=150) of the NP swabs and 39% (N=52) of the fine aerosol sample. This is positive proof that just breathing (tidal volume breathing) results in dispersing infectious viral particles into the air. The influenza cases did not sneeze during the collection period. Viral shedding was greater for men. Women coughed more frequently but shed significantly less virus per cough. Increased BMI produced increased viral shedding in the fine aerosol and the speculation was that increased BMI causes a tendency for small airway collapse and that may lead to increased shear forces that produce the fine aerosol. Since sneezing was not observed - it was not considered necessary to produce the fine or coarse aerosol. Coughing was present and was a significant predictor of both coarse and fine aerosols.
This is a critical paper that I hope that all public health officials, administrators and architects will take note of. It takes more than handwashing and coughing into your sleeve to protect people against influenza virus. It takes recognition that this is an airborne virus and it is aerosolized by breathing. Physicians are on the front lines when it comes to virus exposure and we need better barrier methods to prevent exposure. During flu season I sit in a 8 x 10 foot office and talk with people who sit about 4-5 feet away from me. I talk with most of them for 20-30 minutes or about the length of time of the experiment. The symptoms listed in the severity scale below are incorporated into my review of systems and there are some days when 100% of the people I see have a respiratory infection. If they all have influenza, 30% will leave aerosolized virus in my office just from talking with me. Is there a better way to do things to minimize exposure?
I think it starts with building design. Rooms that are all individually vented to the outdoors on both the intake and exhaust side. Heat exchangers exist today and can be used for this purpose. Starting with influenza as the model and optimizing air flow and humidity to decrease infection rates is a start. Interviewing people across barriers or using television cameras is another possibility especially if vulnerable populations need to be protected from consultants who may be carriers. The tremendous lack of psychiatric infrastructure compounds the problem. Although the building that I refer to was ultimately replaced and torn down - psychiatric services are typically housed in the oldest and most run down buildings. Today jails have replaced psychiatric hospitals and the jail infrastructure is no better. It is common to see patients who are acutely ill with influenza in these settings. Psychiatric beds need to be in an environment that reduces the transmission of infectious diseases including airborne viruses.
The work does not stop at that level. The ways hospitals and buildings are cleaned needs to be thoroughly investigated. Carpet and floor cleaning equipment clearly leads to the dispersion of particles in the carpeting or on the floor. I am not aware of any initiative to make sure that cleaning the surfaces in buildings does not leave the air contaminated.
My advice is to spread the word and this reference to anyone who is unsure about airborne viruses. I am hopeful that at some point over the next 10-20 years the environmental aspects of the problem will be addressed. That will change the nature of influenza transmission as well as a host of other viruses that get sampled in the HVAC systems of old buildings - probably long after the occupants have been infected by them.
George Dawson, MD, DFAPA
References:
1: Yan J, Grantham M, Pantelic J, Bueno de Mesquita PJ, Albert B, Liu F, Ehrman S, Milton DK; EMIT Consortium. Infectious virus in exhaled breath of symptomatic seasonal influenza cases from a college community. Proc Natl Acad Sci U S A. 2018 Jan 30;115(5):1081-1086. doi: 10.1073/pnas.1716561115. Epub 2018 Jan 18. PubMed PMID: 29348203; PubMed Central PMCID: PMC5798362
2: Airborne Virus Monitoring: unedited search
Supplementary:
Image at the top uses a crowd infographic from Shutterstock per their licensing agreement.
Supplementary 2:
This is the approach the authors used to scoring the flu symptoms severity in their paper (my interpretation) (click to enlarge):
Subscribe to:
Posts (Atom)