Every now and again I flash back to a surgical rotation that I was doing at an old county hospital. It was quite run down. We had a large surgical service comprised mostly of people with gunshot wounds, cancer patients, and people who were in long term care hospitals for mental illness who developed acute surgical problems. Most of the patients who had gunshot wounds had been shot by the police and they had police officers posted outside of their doors. On some days it seemed like there were a lot of police officers outside of every other door for quite a distance down the hallway. We did two sets of rounds - in the morning after the surgical procedures and another set of rounds at about 6 or 7 PM. The evening rounds always ended under fluorescent lights in what is probably a long abandoned nurses station. In this particular case we are rounding with a senior surgeon and a junior surgeon. The senior surgeon has just demonstrated how much he knew and how little the residents knew about the effects and importance of gastrointestinal tract hormones. After a few moments of uneasy dead air, the junior staff asks the intern: "What was Mr. X's calcium level this afternoon?" The labs were typically run at 4PM and in those days we would have started to see results at about 5 or 5:30, but we were all rounding at that time and attempting to answer questions about GI hormones. The conversations went something like this:
Staff MD: "What was Mr. X's calcium level this afternoon?"
Intern: "I don't know."
Staff MD: "What? I expect you to run this service. How can you run this service if you don't know what Mr. X's calcium level is?"
The team got quite nervous in situations like that. Training in medicine puts you directly in the line of fire or at least it used to. These days commentary and affect like I witnessed that day might lead to some type of disciplinary procedure for the staff physician. Something that could be passed down on credentialing forms and haunt a physician for the rest of his or her career. A type of pseudoaccountability arranged by the bean counters essentially to manipulate physicians. In this case, it was considered to be a learning experience and culturally appropriate.
In this case the intern in question seemed to recover. Things went well for another few days. And then he was gone. The rumor was he was asked about another lab value, gave an answer that was slightly incorrect as in no physiological difference between the answers. He was fired for making up the answer. Keep in mind that this incident occurred at a time when there were hundreds of lab values to track and the technology was at a primitive state relative to what is currently available. The computers were slow and getting results took a lot longer. Medical students, interns and residents had to write the labs down on cards using whatever shorthand they could devise. In the process some data was memorized but not all or most of it. But the difference here is that the integrity of the answer was called into question. The assumption was that you either know the answer for sure or you say you don't know. There are no near misses. The judgment is that you made something up and that is unacceptable. In the years since, I have seen quite a few colleagues fall by the wayside as a result of similar incidents or what were considered to be errors in judgment by the senior faculty.
In recent times, I think there is a tendency to lump this behavior in the category of senior faculty being abusive toward physicians in training. That certainly may be true, but it is also true that it draws a very clear line about what you need to be doing as a physician as opposed to what you may have done in your undergraduate major. You can no longer make things up like you used to do in your philosophy and English literature classes. You have to be brutally honest about what you know and what you don't know. I don't think there is a physician alive who will not tell you that knowing this is one of the most critical aspects of training as a physician. The ultimate test of whether you are patient centered is whether you will not try to protect yourself - but whether you can be brutally honest even in a situation that may put you at risk professionally. Can you acknowledge mistakes, lapses in judgment and most importantly a lack of knowledge or expertise? Patient safety depends on it. That atmosphere also has the effect that you show up for work. If you know that you are a target for any faculty who want to criticize you, you tend to want to know everything there is to know about the patients on your service. In contrast to the events where the question does not get answered I have seen residents give tutorials on ventilator settings or pressure recordings by Swan-Ganz catheters. They were motivated to some degree by knowing that teaching staff would be asking and their assessment depended on their answers.
The reason for that introduction is that it frames the backdrop for a discussion from a financial thread with a very interesting title: Will Ebola Vanquish the MBAs Who Run Our Hospitals? It is a title by a blogger and certainly eye-catching. I have followed this blogger for a number of years and agree with a lot of what she has to say about the way financial services are managed in this country. I have disagreed with her about some of her medical opinions, but this post is something that I can agree with. I was recently e-mailed about my tendency to selectively find research that supports my opinions. I consider this to be more opinion to support my opinion. Research on how businesses manage medicine is as scant as research on management in general. Business people tend to produce papers suggesting there are deficiencies and then say how they will correct those deficiencies. There is really hardly any research to support business opinion. The opinion in this case looks at a topic I frequently comment on - how can business people with no medical or scientific training manage physicians and medical facilities? In my opinion they clearly can't but let's look at what is presented in this article.
The basis for the article is essentially opinion in the press and the opinion of a medical blogger. The conflict-of-interest here that is usually glossed over is that any journalist, newspaper, or blogger wants the public reading their stuff. It will be provocative or sensational. A measured analysis is not typically seen. For example the comparison of staff infection rates between the staff at Dallas Presbyterian Hospital (DPH) and Doctors Without Borders (DWB) in Liberia seems pointed, but the obvious question is whether the infections rates vary with experience. For example did the DWB staff in the earliest stages of their involvement have infection rates as high as were portrayed in the DPH staff. Can a direct comparison be done without that information? The highlighted emergency department (ED) problems are similarly problematic. If you pull up the Internet sites for the DPH system of care they are affiliated with a number of inpatient psychiatric units. Is the wait time a reflection of a large pool of chronically mentally ill or poorly stabilised psychiatric patients being stuck in the ED? If that is true it would still be consistent with some of the authors concern about the lack of public health concern and the fact that lower socioeconomic classes come face to face with the wealthy in such settings. It is also an aspect of the mismanagement by rationing that is pervasive with systems of care managed by large businesses.
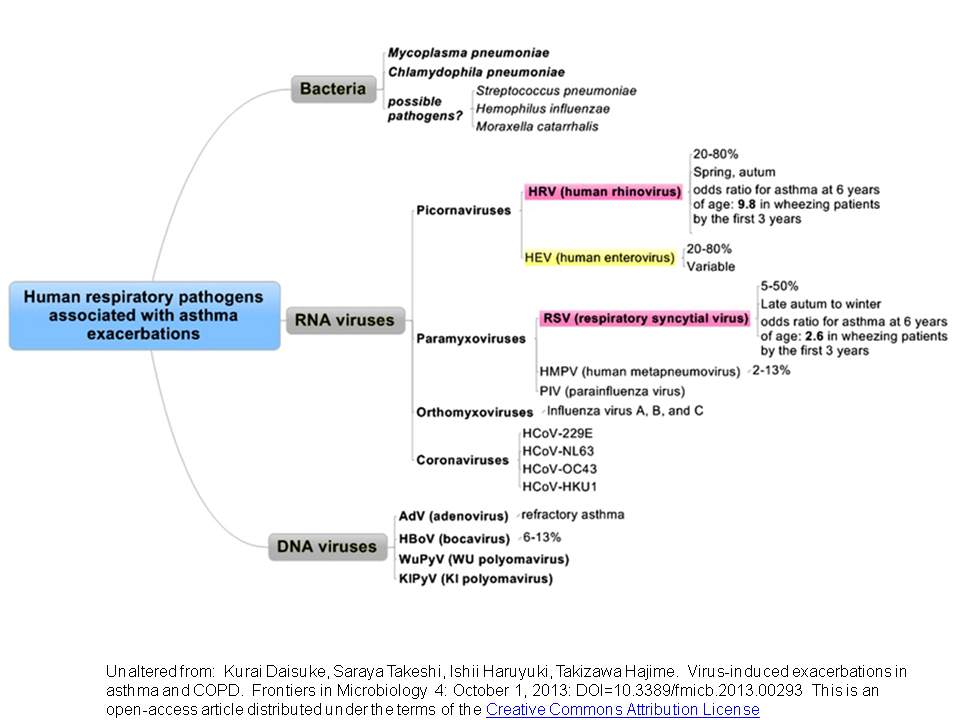
I have first hand experience with infection prevention in hospitals and attempt to stop widespread outbreaks from respiratory viruses. Keep in mind that the Ebola virus is not an airborne virus. All of the remarks in this paragraph are about airborne viruses especially Influenza virus. For a number of years I was extremely disatissfied with the epidemics of respiratory viruses that swept through the staff where I was working. Employer rules about paid time off only worsen the situation because the incentive is to work when you are sick to prevent loss of vacation days. But the most frustrating part of the problem (apart from being sick 3-5 times a year) was that the employer had no real interest in doing anything that might reduce the risk of infections. The intervention I suggested was just improving air flow in certain buildings. The standard reply that you get is "wash your hands and cough into your sleeve." Those are certainly common sense measures but as far as I could tell had no impact on the rate or severity of infections each year. Hospital administrators everywhere seem to be in denial of the fact that airborne pathogens exist and washing your hands and coughing into your sleeve will not protect you against airborne pathogens. I was also a member of two different Avian Influenza task forces. At the time there was much uncertainty about a widespread epidemic that could not be contained. We were setting up for the worst case scenario of thousands of people (both infected and not infected) coming into EDs and how to triage and treat people. After years on these task forces it became apparent to me that nobody was really interested in planning for the prevention of mass casualties from an airborne virus. There was no planning for any additional negative pressure airborne isolation rooms and no planning for any additional bed capacity in the event of a widespread epidemic. There was planning for what to do with the expected bodies. In the end it seemed that all of our hopes were pinned on a rapidly disseminated vaccine or antiviral medication. The specifics of the antiviral medication were murky. We were shown a picture of a large pallet of oseltamivir sitting in a warehouse somewhere. From a business administrator's standpoint, planning to use imaginary resources from the government is always preferable to more functional planning because it is free. My personal experience in this area from volunteer work on respiratory viruses is entirely consistent with the notion that health care businesses are not administered in a way that is consistent with public health needs in the case of infectious epidemics.
The Naked Capitalism article contains analysis from Roy Poses, MD of the Health Care Renewal Blog. He looks at inconsistencies in the media and concludes that this is another case of health care leaders being untrustworthy. That appears to be a central theme of his blog and he goes on to criticize them for being inconsistent, suppressing information from employees that may be critical to public health, and having an inflated sense of self importance. These patterns are easily observed by physician employees of health care organizations. For at least a decade after passage of The Health Insurance Portability and Accountability Act of 1996 (HIPAA) it was impossible to get necessary information from health care organizations, even in the case of needing to provide emergency care. I would routinely request information and even send a HIPAA compliant release signed by the patient and I would get a blank form the other hospital saying that my patient had to sign their form and fax it back. Hospital administrators were a big part of that process. It is common for the clinical staff to be buffeted by the next big idea from their administrator. That can range everywhere from high school style pep rallies that are supposed to improve employee morale to a new productivity system that is guaranteed to get even more work from physicians. In every case, the administrator in charge could be making 2-5 times what the average physician makes for considerable less accountability, practically no "evidence based" methodologies, and no measurable productivity. As pointed out in the article, public relations is much more of a factor in the CEO's reputation. From the article:
" On Health Care Renewal we have been connecting the dots among severe problems with cost, quality and access on one hand, and huge problems with concentration and abuse of power, enabled by leadership of health care organizations that is ill-informed, incompetent, unsympathetic or hostile to health care professionals’ values, self-interested, conflicted, dishonest, or even corrupt and governance that fails to foster transparency, accountability, ethics and honesty."
There are additional lessons from the decimation of mental health care in the United States, especially care delivered at tertiary care and community hospitals. There is perhaps no better example of low to no value service that is the direct result of non-medical management. There is no coordinated public health effort either improve the care of psychiatric disorders or specific high risk behaviors like suicide or homicide. The standard approach is rationing of both care that would result in stabilization but also bed capacity that would alleviate congestion in emergency departments. There should be no debate on cost, inpatient psychiatric care is without a doubt the low cost leader and is set to match reimbursement from a high turnover low quality model. Psychiatric services in clinics and hospitals have a lot in common with what Dr. Poses observes on the administrative side of many health care organizations.
Responding to the question of "Will Ebola Vanquish the MBAs Who Run Our Hospitals?" - my answer would be no. It is always amazing to consider how so many people in business with so little talent can end up running things and making all of the money essentially through public relations, advertising and lobbying politicians. There is no shortage of self proclaimed administrator-visionaries. The author here should know that their power is consolidated around the same strategies that have worked for the financial services industry. Managed care business strategies based on no science or input from physicians are now in the statutes of many states and in federal law. They have successfully institutionalized business strategies designed to return profits to corporations as the rules that govern healthcare. The pro-health care business lobby essentially gets what they want and the professional organizations are weak and ineffective, but continue to browbeat their members for contributions. Administrators have a lock on running health care and demanding whatever accountability they demand from health care professionals while having no similar standards for themselves.
I can't think of a worse scenario for addressing potential public health problems whether that is an infectious epidemic or the continued mental health debacle.
George Dawson, MD, DFAPA
Supplementary 1: Kaiser Family Foundation brief PowerPoint and Infographic on the current Ebola out break.
Supplementary 2: I decided to add the above table comparing the accountability of physicians with business administrators. Certainly there may be some things I have missed on the business administrator accountability so if I missed anything please let me know and I will include it. From what I have observed, health organization and hospital CEOs are typically accountable to a Board of Directors that has very little physician or medical representation. Often the Board is stacked with people who rubber stamp what the CEO wants to do. Like the web site referred to in the above post there is often an aura that the CEO and the Board have visionary-like qualities that are based on public relations and advertising rather than any academic work or actual results. I have never really seen an administrator who was a visionary or knew much about medicine - but you can certainly read their proclamations about how medicine should be reformed on a daily basis in many places on the Internet. The usual argument for all of the physician accountability is that it is a privilege to practice medicine and therefore regulation of physicians needs to reduce the privacy rights of physicians and subject them to much closer regulation than other professionals. Why wouldn't that approach apply to the people who actually determine whether a patient gets health care, medications or a specific benefit? Why wouldn't that same logic apply to the people who really run the health care system?