in the early days of this century, I spent a lot of time in
Avian Influenza Task Force meetings. I was on two separate task forces and at the
same time working on an acute care inpatient psychiatric unit. One of the
meetings took up four hours in the afternoon and I would have to go back to my
unit and make up those four hours. I made the mistake of that not saving all the
documentation from those meetings. There were hundreds of pages. The main focus
of one task force was on “surge suppression” or helping with crowd control to
prevent emergency departments from being overwhelmed by people who did not
really have the viral infection. The other meeting was more about the actual
response to the viral infection. I was always skeptical of what I heard. We
kept hearing that if there was an epicenter of infection, large pallets of Tamiflu
would be on the way. We saw presentations with pictures of those pallets under
plastic wrap. At the same time there was discussion about morgues and refrigerated trucks that have become part of the current crisis.
I was more concerned about what would happen to inpatient
psychiatry units. I kept hearing that the medical and surgical beds would be
overwhelmed. When I suggested that we increase the capacity of negative airflow
rooms and rooms vented directly to outside air, I was told that was impossible.
One expert gave the opinion that if there is an airborne virus in the
hospital: “The minute you walk into the hospital you should be wearing an N95
mask”.
That was about 2005 and I had never heard of an N95 mask
before that. I had certainly worn masks for painting, dust protection, and
various chemical and biological experiments that I did in the course of
education and research. I went out and bought a small package of N95 masks. I
fitted them per the instructions and noticed a couple of things. The fit was extremely snug due to upper and lower elastic bands (that have a much smaller
circumference than a human head or neck), the circular contour of the mask providing a suction fit to some extent, and
a flexible metal band that bends over the bridge of the nose to effectively
seal that area. When you are wearing an N95 mask your voice is muted and you
are breathing against resistance. If you wear it long enough, it becomes soaked
with exhaled droplets. I rapidly concluded that it would be nearly impossible
to conduct a psychiatric interview wearing this mask.
I never really learned at the time whether there was a plan
to shut down inpatient psychiatry and use all the beds for avian influenza
patients. Thankfully it never got to that point. Flashing forward 15 years a
real pandemic is upon us and the problems remain unsolved. Inpatient
psychiatric units and residential drug and alcohol treatment units are
considered necessary services in most states and they remain open. Very recent
information from the authorities now suggest that SARS-CoV-2, the virus causing
COVID-19 is airborne and that there are a significant number of asymptomatic
carriers.
I have been using telepsychiatry at this point for two
weeks and it seems to be going well. There are definite constraints compared with
face-to-face interviews. I have noticed more constraints since my original post
on this topic. I put a couple of questions out there on social media today to
see how my colleagues who are still actively engaged in acute care are adapting
to the changing parameters of this pandemic. Before putting those questions out,
I had the thought that telepsychiatry could be used over the short distances in
inpatient settings. As a resident I had the experience of observing
psychotherapy firsthand and being observed from adjacent rooms that also had
microphones for communication between those rooms. I was interested in seeing
whether or not anyone had implemented those solutions. I was pleased with the feedback that I have
so far.
One of the first responses was that psychiatric staff were
using surgical facemasks and face shields in some settings. In other settings, adjacent
rooms and telepsychiatry both on-site and off-site were being used for
acute-care units. The most unique solution I heard of was a consultation
liaison team using iPads to interview medical and surgical patients remotely where
possible. That reminded me that some people have joined my telepsychiatry
sessions using smart phone apps. It was generally very suboptimal if the phone
was not completely stabilized. I also
had the experience this week of getting a link sent to me from a colleague who
worked for a large healthcare system. It was an invitation to open up a video
session with him even though I am not registered in his clinic. It was very similar to a Zoom session that I
did for a podcast. All this information shows that there are technologies
available right now that are effective and actively being used. They have also
been very rapidly deployed or are in the process of being deployed. There is
some potential that this sudden change in the delivery of psychiatric services
may be a more permanent one.
I asked the question about whether or not the services were
saving personal protective equipment (PPE). The response to that question was
somewhat mixed. I am not clear on what it means but speculate that some of the staff
still need to have direct patient contact at some point during the day. Most
acute-care staff at this point have been assigned PPE. The PPE specifics seem
to vary from place to place but it is clearly rationed. If I was designing a survey of acute-care
psychiatric facilities I would like to see the specifics of how many people had
N95 masks and other kinds of protective gear.
Preadmission screening remains a question mark. There is general agreement that there is an asymptomatic carrier state for SARS-CoV-2 (1,2). Carriers may have a lower viral load and be partially symptomatic. Most people admitted to inpatient psychiatric units these days require intensive nursing care for their own safety. If there were environments where patients with COVID-19 could be safely segregated and treated that would be ideal, but I doubt those kinds of environments exist on inpatient psychiatric units. Even then the asymptomatic carriers would require the same psychosocial interventions as non-carriers. The general screening done is to ask about contact with known cases and daily temperatures. I am not aware of any screening procedures that involve trying to identify the virus and carrier state.
Preadmission screening remains a question mark. There is general agreement that there is an asymptomatic carrier state for SARS-CoV-2 (1,2). Carriers may have a lower viral load and be partially symptomatic. Most people admitted to inpatient psychiatric units these days require intensive nursing care for their own safety. If there were environments where patients with COVID-19 could be safely segregated and treated that would be ideal, but I doubt those kinds of environments exist on inpatient psychiatric units. Even then the asymptomatic carriers would require the same psychosocial interventions as non-carriers. The general screening done is to ask about contact with known cases and daily temperatures. I am not aware of any screening procedures that involve trying to identify the virus and carrier state.
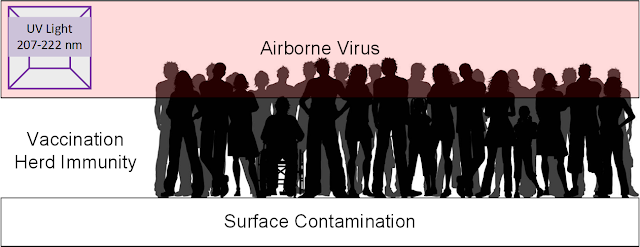
My overriding concern is that medical and psychiatric staff
everywhere have adequate protection. We have known since my days on the avian influenza
task forces that airborne viruses are difficult to contain. They can infect
through surface contamination, droplet contamination, and traveling on air
currents. Working to cancel all those routes of infection is a tall order
especially on an inpatient psychiatric unit.
The only practical way to maintain the level of
communication necessary and minimize risk of infection is through some type of electronic
communication. Some of the early methods have been listed in this post. Having
worked in these settings for a large part of my adult life I am very concerned about
the staff with daily direct patient contact including nursing, nursing assistants, and occupational
therapy. Housekeeping staff also have a vital role and are directly exposed to most contaminated surfaces. I have seen large numbers of inpatient
staff come down with seasonal respiratory viruses and I know that vulnerability
is there. They all need PPE. We need additional innovation in these settings to protect all staff
and patients.
And we have needed that innovation for a long time.
George Dawson, MD, DFAPA
References:
1: Lai CC, Liu YH, Wang CY, Wang YH, Hsueh SC, Yen MY, Ko WC, Hsueh PR. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Facts and myths. J Microbiol Immunol Infect. 2020 Mar 4. pii: S1684-1182(20)30040-2. doi: 10.1016/j.jmii.2020.02.012. [Epub ahead of print] Review. PubMed PMID: 32173241.
2: 1: Hu Z, Song C, Xu C, Jin G, Chen Y, Xu X, Ma H, Chen W, Lin Y, Zheng Y, Wang J,Hu Z, Yi Y, Shen H. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020 Mar 4. doi: 10.1007/s11427-020-1661-4. [Epub ahead of print] PubMed PMID: 32146694.
References:
1: Lai CC, Liu YH, Wang CY, Wang YH, Hsueh SC, Yen MY, Ko WC, Hsueh PR. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Facts and myths. J Microbiol Immunol Infect. 2020 Mar 4. pii: S1684-1182(20)30040-2. doi: 10.1016/j.jmii.2020.02.012. [Epub ahead of print] Review. PubMed PMID: 32173241.
2: 1: Hu Z, Song C, Xu C, Jin G, Chen Y, Xu X, Ma H, Chen W, Lin Y, Zheng Y, Wang J,Hu Z, Yi Y, Shen H. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020 Mar 4. doi: 10.1007/s11427-020-1661-4. [Epub ahead of print] PubMed PMID: 32146694.
Supplementary 1:
I am very interested in what you are doing at your facility to contain this virus while continuing to go to work every day and treat patients. I am also very interested in whether you have enough PPE. I am interested in hearing from everybody staff psychiatrists, residents, social workers, occupational therapists, nurses, nursing assistants, and housekeeping staff. Please post in the comments section below and feel free to remain anonymous.
Graphic Credit:
I am very interested in what you are doing at your facility to contain this virus while continuing to go to work every day and treat patients. I am also very interested in whether you have enough PPE. I am interested in hearing from everybody staff psychiatrists, residents, social workers, occupational therapists, nurses, nursing assistants, and housekeeping staff. Please post in the comments section below and feel free to remain anonymous.
Graphic Credit: