I finished reading a paper last night about estimating the
prevalence of depression using the PHQ-9 (1). The paper had 76 authors
including one of the most well recognized epidemiologists in the world. It was
focused on the differences in estimating depression prevalence using a
structured research interview specifically the SCID (Structured Clinical
Interview for Diagnostic and Statistical Manual of Mental Disorders versus the
PHQ-9 - a nine item checklist based on the DSM criteria for major depression.
If you ever need a reference paper for how to write an epidemiology paper based
on a literature search this is probably a good one to have.
The authors did an extensive literature review in the end
found 44 (n=9,242) studies that looked at comparisons between the PHQ-9 and the
SCID. The result was that the pooled
results showed that depression prevalence estimates with the PHQ-9 (total score
≥ 10) were about 25% and for the SCID it was 12%. Modifying the criteria for the PHQ-9 to a
score of ≥ 14 and using a separate PHQ-9 diagnostic algorithm resulted in a
lower prevalence estimate but a wide margin of error. The authors conclude that structured
interviews are the best approach to prevalence estimates largely because they
are closer to clinician style interviews and through clarification, they can
limit confounding variables. Nobody ever seems to comment on the restrictive
aspects of both checklists and structured interviews. After all, DSM criteria that are embedded in
the matrix of questions and elaborations in the SCID are basically converted to
nine unidimensional questions in the PHQ-9. It should be obvious that there
would be a correlation between the two when the PHQ-9 is validated against the
SCID, but instead it is accepted as an academic exercise.
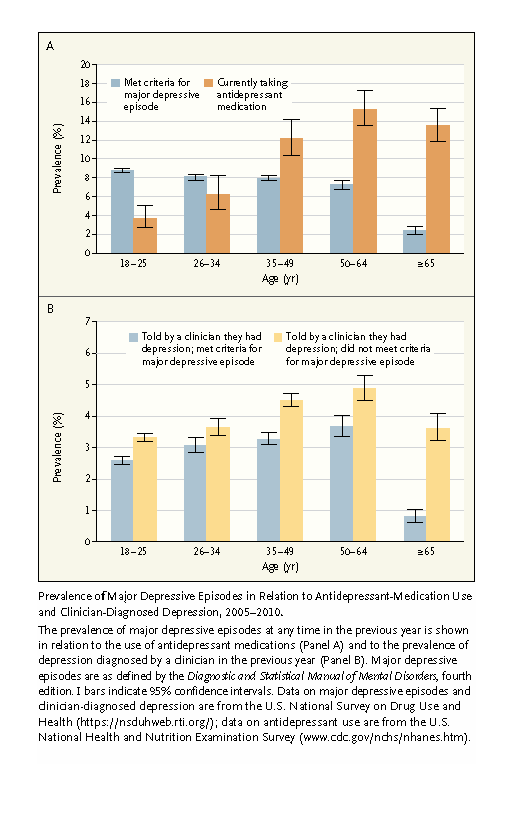
The first thing I thought about when I saw these numbers
and read the paper was “even the SCID prevalence figures are too high”. I base that on numbers available in a standard
textbook on psychiatric epidemiology (2).
Reviewing much larger sample sizes across 25 countries yields one-year
prevalence figures for depression of 2.6-10.3% (median 5.3%) lifetime
prevalence figures of 2 to 16.2% (median 8.6%). In that table the variation in
very large community samples ranging from 5000 to 42,000 subjects in the United
States seem to depend on the research methodology more than anything and
structured interviews other than the SCID were used.
The selected samples from reference 1 are detailed in table
1 and very few of them are community samples. They are relatively small
outpatient samples of identified medical patients or people seeking medical
services for themselves or another person. Many of the conditions have known
comorbidity with depression. The authors list this as a study limitation
particularly “where the presence of transdiagnostic somatic symptoms and
adjustment to illness or injury may have contributed to error variance”. They also comment on the heterogeneity of the
study settings and how that might affect the data. That is certainly my concern
for post stroke patients, multiple sclerosis patients, Parkinson’s disease
patients, epilepsy outpatients, and other neurological conditions for
depression is a common comorbidity. The implicit message from this paper is
that depression prevalence estimates from clinical samples will be higher than
estimates from epidemiological community surveys.
But there is a much larger lesson here than differences in
depression prevalence estimates based on methodology or clinical sample. For me
the heart of the matter is the difference between a psychiatric interview, a
structured clinical interview, and a checklist.
I have expressed my concerns over the years that checklists are
currently surrogates for psychiatric interviews and I can confirm this on a
weekly basis. Most the patients I see have seen primary care physicians or
nonpsychiatrists and they tell me how they are given a PHQ-9, a diagnosis based
on that rating scale, and a prescription. That model of care is promoted by
some organizations as “evidence-based medicine”. In some cases it is called
“measurement based medicine”. The state of Minnesota for example has a project
were all PHQ-9 scores are collected from any clinic treating patients with a
diagnosis of major depression. This was supposed to be some kind of quality
measure even though an analysis of all the cross-sectional data has never been
done.
When I talk with people who have taken these checklists and
asked them about depression it is common to hear the question “What do you mean
by depression? I am still not sure about what that means and the difference
between depression and anxiety.” I hear those questions from people who have
been filling out the rating scales and getting medications prescribed to them
based on those scores and yet they are uncertain about the concept of
depression. How can that happen?
The obvious way is by limiting choices. If a nine-item
checklist is given to a person and they are told to answer a specific question
as one of 4 choices, most people will check a box. In the case of the SCID – there is more
elaboration. People are asked about
whether there was a time in the last month when they felt “depressed or down
most of the day nearly every day?”. They are asked to elaborate and whether or
not it affected their interest or pleasure in activities. They are asked if it
lasted as long as two weeks. At that point there is a qualifier that says the
interviewer is not supposed to include symptoms “that are clearly due to a
physical condition, mood-incongruent delusions or hallucinations, incoherence
are marked loosening of associations, or that are clearly part of the residual
or prodromal phases of schizophrenia”. Additional questions about symptoms of
the depressive syndrome follow.
Many clinics use electronic health record (EHR) templates that include checklists about all of the major classes of psychiatric syndromes. They are a variation on the SCID but they generally result in more spontaneity and elaboration than a checklist but not as much as the structured interview. What is lost along the way? I would suggest – a lot.
The rationale for structured interviews is reliability or consistency
in responses. If any population is given
a matrix of the same questions to differentiate different conditions – no matter
how exhaustive - there will be a pattern of responses that has internal
consistency. Viewed from that perspective, the PHQ-9 is just a very abbreviated
and less specific version of the SCID – hence the difference in prevalence estimates.
Although prevalence estimates are often the focus of
criticism (too high, too low, just right) what is typically missed is that they
really have limited application to good clinical psychiatry. Psychiatrists do
not do SCID interviews on patients and the reasons may not be that apparent.
Psychiatric diagnoses depend on a lot more than a symptom checklist and the
total time to administer a SCID (2-3 hours) is prohibitive. There is also a question of efficiency. In practice the psychiatrist has to be able to focus on all relevant aspects of the identified problem not areas that are not considered to be a problem. Most importantly
– the psychiatric interview needs to recognize that the person in the conversation
has a unique conscious state that is interpreting their emotional, cognitive,
and physical experience. The psychiatrists has to understand how that is happening.
There is probably no better discussion of this crucial
aspect of the interview than that provided by Nordgaard, Sass and Parnas (3). These
authors use the term “a conversational, phenomenologically oriented
interview, performed by am experienced and reliability-trained psychiatrist.”
as the more optimal and preferred approach. After reading their work, I realized that it
is what I have been doing for the past 35 years. In a more recent article, this group has compared
American phenomenology to a simple study of signs and symptoms and suggested
their use of the term is more consciousness based:
“It refers to a faithful exploration, description, and
conceptualization of the patient’s contents and structures of subjective life
and modes of existence (eg, not only the content of the delusion but its mode
of emergence and articulation and ways of experiencing the delusion)” (4)
They suggest this requires an interview that maximizes self-description
and a knowledgeable physician with a “rich conceptual repertoire”. Since the DSM approach is intentionally atheoretical
– it speaks to the need to be trained in a variety of psychopathological
theories. Andreasen (5) has previously written
about the death of phenomenology as being an unintended consequence of the DSM approach. In my experience it is easily approached in
residency training as the need for a empathy based formulation that makes sense
to the patient. In their article (3) the
authors provide a table comparing what is elicited with a structured interview as
opposed to a phenomenologically based conversational interview. In the table below I provide my own example
for a patient with depression. I will add that in most electronic health
records these days there are templates that are essentially structured
interviews requiring brief responses and very little discussion about the process
or content of those responses. Those templates are further limited by the fact that all of the information needs to be entered by the psychiatrist doing the interview - a further inefficiency.
Structured
Interview
|
Conversational
Interview
|
She has
been depressed all of her life with very few periods of neutral mood. The
depression includes periods of extreme irritability. The depression worsens from time to time.
|
She had
had long term depression but it is clearly worsened in specific contexts.
There are situations that specifically make her anxiety worse and when this happens,
she “spirals down” into a depression and will often spend the entire weekend
in bed. A lot of these episodes are associated with a stressful job and a
specific interpersonal conflict at work.
|
She
describes a motivational deficits and anhedonia.
|
During
the episodes of worsening depression and isolation – she watches TV all
day long. She is not motivated to exercise but occasionally will push herself
to go for a jog. She was the high school state record holder in the quarter
mile. Even though it is initially difficult she feels much better afterwards
and the activity reminds her of the importance of exercise in her life and
how she used to work out in high school.
|
Decreased
concentration and memory problems
|
She has
had life long concerns about her memory and at one point considered “getting
tested” for ADHD. She got a degree in molecular biology and graduated summa
cum laude. She is currently working in a professor's lab and thinking of
applying for a PhD program. She has no problem reading and retaining information
from highly technical journals and devising lab protocols or her favorite science
fiction. She attends meetings where her mind wanders.
|
Depressing
thoughts
|
“I am a
perfectionist and am my own worst critic.” She was encouraged from an early
age to get A grades in school and had a nearly catastrophic reaction when she
got a B in high school. She still remembers
that teacher who told her that getting a B would be “good for her”. Her
parents were always critical and she realized at some level she has
internalized some of these criticisms especially when it comes to body image
and weight: “I don’t think being petite and wearing the latest fashions makes
me a better scientist”. Despite fairly constant self-criticism it never
gets to the point where she feels worthless.
|
I have
some suicidal thoughts but have never made a suicide attempt or an attempt to
hurt myself.
|
“I read
a journal article somewhere that looked at the prevalence of suicidal
thoughts and they are fairly common.” She describes intrusive thoughts about
suicide that are obsessional in nature. “I drive across this bridge every day. If I am having a bad day, I think about
cranking the wheel at the half way point and driving off. But I know I will never
do it. I am too chicken and I have too
much going for me. I want to hang
around and see what happens.”
|
The conversational interview is information rich and allows
for more extensive pattern matching. The
PHQ-9 and even the SCID describes a very limited pattern or as Kendler (6) describes
indexing of major psychiatric disorders.
That is the primary (and limited) intent of the DSM. But Kendler points out that it is really a
jumping off point for the additional study of psychopathology. I would also point out that it ignores what
is the elephant in the room for psychiatrists – human consciousness. Consciousness in psychiatry tends to be
mentioned only when it is grossly impaired rather than existing as the every day
moderator of everything.
When the additional pattern matching takes place, the only
real limit is the interviewer’s ability to recognize it and what it means. In
the ideal world that should lead to further elaboration of the patient’s
concerns, education based on the psychiatrist’s understanding of the general
problem and more specifically how it affects the unique patient, and specific
treatments that have worked before. It
can extend to a unique approach to the associated DSM disorder that would not
have been possible with a highly structured interview. One of the best examples I can think of are life
long sleep problems that become anxiety and depressive disorders as an adult –
because the development of those disorders and the sleep disorder is not
covered in detail. There are a lot of
examples.
In closing this post, prevalence estimates for psychiatric
disorders vary greatly. That is the
expected result of the screening methodology that includes the instrument used,
the population sampled, and the prevalence of the disorder being screened in
the population. Very basic screens like checklists used as a proxy for diagnoses
will have the highest prevalence estimates. More comprehensive structured
interviews will be somewhat lower. The gold standard for epidemiological
work (structured interview) is not the gold standard for clinical work
(the semi-structured phenomenologically oriented interview). It is also the reason psychiatrists need to
know psychopathology, phenomenology, and case formulations based on those
disciplines.
George Dawson, MD, DFAPA
References:
1: Levis B,
Benedetti A, Ioannidis JPA, et al. Patient Health Questionnaire-9 scores do not
accurately estimate depression prevalence: individual participant data
meta-analysis. J Clin Epidemiol. 2020;122:115‐128.e1.
doi:10.1016/j.jclinepi.2020.02.002
2: Hasin DS, Fenton
MC, Weissman MM. Epidemiology of
depression disorders. In: Tsuang MT, Tohen M, Jones PB, editors. Textbook of Psychiatric Epidemiology,
Third Edition. West Sussex: Wiley Blackwell, 2011: 289-309.
3: Nordgaard J, Sass
LA, Parnas J. The psychiatric interview: validity, structure, and
subjectivity. Eur Arch Psychiatry Clin Neurosci. 2013;263(4):353‐364.
doi:10.1007/s00406-012-0366-z
4: Parnas J,
Zanderson M. Rediscovering disordered selfhood in schizophrenia. Psychiatric
Times. Jun 08, 2020
5: Nancy C.
Andreasen, DSM and the Death of Phenomenology in America: An Example of
Unintended Consequences, Schizophrenia Bulletin, Volume 33, Issue
1, January 2007, Pages 108–112, https://doi.org/10.1093/schbul/sbl054
6: Kendler KS. DSM issues: incorporation of
biological tests, avoidance of reification, and an approach to the "box
canyon problem". Am J Psychiatry. 2014;171(12):1248‐1250.
doi:10.1176/appi.ajp.2014.14081018