Jeffrey Lieberman, MD is the current President of the American Psychiatric Association (APA). He came out today with the first in a series of three statements on the changing profession of psychiatry. He starts out with an uneven historical recap of the first 200 years of the profession. I am probably sensitized to his use of Freud as an inflection point with my recent study of the philosophy of science. Freudian psychoanalysis and Adlerian psychology were Popper's original example of fields that did not meet logical criteria as a science. They were not falsifiable and therefore were unscientific. At the same time the neuropsychiatric movement based on phenomenology and neuroanatomy associated with German asylums is not mentioned. I suppose that a historical context is appropriate when considering all of the inflection points for the profession but let's face it - the first 150 of those 200 years are irrelevant to any scientifically based psychiatry and can be disregarded. He added a few paragraphs on the advent of psychopharmacology and the DSM as additional innovations and ends with his idea that the rising cost of health care and the pace of scientific discovery will be the two forces that shape the profession of psychiatry going forward.
My first problem with this statement is that there seems to be no role for psychiatrists or their professional organization in shaping the profession. We are there to be buffeted by rising costs and scientific discovery. Like most fields of medicine innovation has been driven by the clinicians and researchers in the field. When Len Stein, MD and his collaborators noticed that patients at the Mendota State Mental Health Institute were residing there in appalling conditions, they invented community psychiatry and community support teams and moved them out. There have been a long list of innovators in psychotherapy, psychopharmacology, neuroscience and in the general methods of psychiatry.
Taking Dr. Lieberman's points individually and starting with the rising cost of healthcare - what does that mean exactly and what does it mean in terms of psychiatric services? Thirty years ago some health plans covered unlimited psychotherapy. Many psychiatric trainees underwent psychoanalysis as part of their training and it was covered by health insurance. Today they would likely get a brief evaluation or a checklist and the offer of antidepressant medication if they scored high enough on a rating scale. If they were very fortunate they might see a crisis counselor for two or three sessions. How could this change in care possibly be related to rising costs? Psychiatric care has never been cheaper. The rising costs in medicine have to do with services that have pricing power and that never involves mental health. The real challenge here is a political one. It is very apparent that political systems and their partners in the business community will do everything possible to restrict access to psychiatric services - no matter how cheap they are. In the general scope of actual payments to providers there are no services that are more cost effective than psychiatry and until very recently that was essentially guaranteed by special billing codes that reimbursed psychiatry less.
The impact of rationing of psychiatric services by managed care companies, state and federal governments go beyond the purely economic. When psychiatric services are easily rationed, evidence based services that are more expensive like Assertive Community Treatment can simply be made a non covered service. There are few functional detoxification facilities for people with severe drug and alcohol problems. Most people are sent home from an emergency department with medications to "self detox" or sent to a county run facility with no medical services. They are readmitted when that fails or when they develop complications that require intensive care such as seizures or delirium tremens. The majority have no chance to achieve sobriety from outpatient detox of significant addictions. The hospital evaluation and treatment of severe disorders that often take weeks or months to assess and treat are restricted to a few days. The actual admission and discharge decisions from hospitals and treatment centers are no longer medical decisions but they are based on arbitrary guidelines made up by business organizations. Entire hospital and clinic environments are run by administrators with no psychiatric training. There are actually situations where administrators seem to believe that they can design treatment programs that target behavioral problems when they are not clinicians. The "rising cost of health care" rhetoric is frequently used to rationalize a nationwide approach to mental illness that is totally nonfunctional. This has been the result of a series of "reforms" that basically turned the field over to the managed care industry.
Psychiatric research and the neuroscience research that applies to psychiatry is vast. When physicians are trained we are all taught to value ongoing education. At some point the education of physicians also became a political football. There are initiatives to teach physicians how to treat pain. A decade later there are initiatives to retrain physicians who are prescribing too many opioids - despite the fact that the original initiative had a goal of appropriate assessment and treatment. Specialty boards and the oversight board unilaterally decided that the public wanted board certification to be time limited. They came up with a Maintenance of Certification (MOC) procedure despite the lack of evidence that it was necessary. That allowed several states to consider tying medical licensing to these costly and unnecessary exams. The best way to educate physicians is an active collaboration at both the clinical and basic science levels like many specialty boards were doing at the time of the new idea about MOC.
These are the dimensions that shape my world as a psychiatrist every day. They have been responsible for the deterioration of the practice environment and decreased quality of care across most treatment settings. Contrary to Dr. Lieberman's points there has been no reform and there certainly is no enlightenment. Despite all of the research and expanding knowledge clinical psychiatry is in the Dark Ages as external forces suppress psychiatrists and limit creativity and innovation.
George Dawson, MD, DFAPA
Jeffrey Lieberman, MD. Change, Challenge, and Opportunity: Psychiatry in Age of Reform and Enlightenment. Psychiatric News August 29, 2013
Friday, August 30, 2013
Sunday, August 25, 2013
Adapting to a Mother with Problems
Mothers have historically held a prominent place in psychiatry. The public often thinks that mothers are blamed for problems with their children, but the research on the matter is less clear and more subtle. That is true even in the case of theorists who placed very little emphasis on individual psychopathology and more on problems within the family system. The concept of "expressed emotion" evolved to describe a critical home environment that may be associated with exacerbations of schizophrenia. Childhood adversity is the current concept that describes a number of factors that children must negotiate and that can be very problematic. The goal of looking at these factors in childhood is an important part of any psychiatric evaluation, but not to look at someone to blame. They are important indicators of the degree of resilience, their perspectives on important relationships and how their relationship with important childhood figures affected their personality development. Almost everyone can recall a critical event that happened in their childhood and they can freeze it in time based on other memory associations. I happened to hear a great example of this on the public radio show "This America Life" today.
The theme of the program today was babysitting and the piece I am interested in was the last segment called "Act Three. Yes There is a Baby" It is a recollection of how a son and daughter interacted with their single mother. It is really a story of how two kids adapted to a mother who had severe problems. It is also a story of how remote events continue to affect people over time. One of the most surprising and consistent observations I have made in my discussions with people over time is how the relationships with parents and siblings are long lasting. They don't seem to fade away over time. Strong emotions and patterns of interpersonal interaction persist for decades if not an entire lifetime. Having no contact with your parents or siblings for prolonged periods of time usually has little effect on these dimensions. This story starts out with a teenage daughter making up a family - the McCrearys who she was babysitting for in order to escape her mother's limitations on her freedom to move around in the 1940s.
This story interested me for a number of reasons, not the least of which is the way it echoed many themes that I have heard from people as well as my own personal experience. The other important point is that it is a true story. With the current constraints on the discussion of true stories by medical professionals, I think we will need to rely more and more on true stories that are openly disclosed in the media. The eliminates any possibility of professional intervention but it allows for the emphasis of important points. In this case I have linked to the transcript because the audio file is not available until later. I agree with the disclaimer on the web site that you should actually listen to the audio file to get the full impact and hear the story in the voices of the people involved.
The story begins with the son Myron telling Ira Glass about how the rules about staying out from the family home were very different for him and his sister. He enjoyed a fair amount of freedom but his mother restricted his sister to going out to church dances. When his sister Carol is contacted, she describes a situation that is much worse. She was followed by her mother's friends. Her mother began calling her a whore at an age before she knew the meaning of the word. Whenever she was employed as a babysitter, her mother needed to know the number in order to check on her. She would also remind Carol and Myron that when their father died she got a lot of advice that she she put them both in an orphanage. She did not and described it as the biggest mistake in her life.
In order to adapt to her mother's restrictive and abusive parenting style, Carol invented a family and would say that she was babysitting for this family when she was really sleeping out on the beach or staying with friends. Mr. McCreary was an FBI agent and therefore she could not give her mother their telephone number. She was also being paid for babysitting in stocks and bonds, so there was no proof of babysitting in money.
The interesting psychiatric aspects of this story are basically threefold. Early on Myron points out that the whole concept of "imaginary people" was something that he and his sister got directly from his mother. She talked about seeing a lawyer, a psychiatrist ("psycholotrist"), and a doctor. In every case the appointments with these imaginary professionals was foreboding. She told the children that she was seeing the lawyer in order to make arrangements to put them in an orphanage. The psychiatrist told her that her children were driving her crazy. The doctor told her she was going to die.
Myron tells the story of coming home one day when he was ten years of age and his mother telling him that she was arranging for him to go to an orphanage with a local priest. He decided he would go away to school at that time, even though he knew there were any number of ways he could have sabotaged it, basically because his mother had been threatening him with an orphanage "all of my life". As a part of that process his mother wanted reassurances that he thought about her "crying my eyes out" when he was at his "fancy school". He decided from that point on (at age 10) that he would never ask his mother for anything or look to her for anything again. He had that insight when he was 30 years old.
Carol lashed out at her mother when she was about 35 years old. Her mother reacted by crying and it was the first time she had ever seen her cry. When her mother stopped crying she said that she did the best that she could have and this lead Carol to the insight:
"And I thought, oh my god, she did. Her best was so bad. Her best was so empty. But she couldn't do any better.."
Accepting that truth and recognizing the importance that her mother had to her grandmother and aunt lead Carol to modify her emotional response to her mother.
The themes in this story are important in psychotherapy and form the basis for most psychodynamic therapies. Although they never made it explicit Carol and Myron both had unique strategies to adapt to their mother's problems. This is a story that has universal appeal. Everyone has landmarks in his or her personal history when an interaction with a parent or a sibling is an organizing event in the rest of their life. The number of possible decisions and behaviors based on that event and their complexity are are well illustrated in this family history. The resilience of these two children and how they overcame childhood adversity is remarkable.
George Dawson, MD, DFAPA
The theme of the program today was babysitting and the piece I am interested in was the last segment called "Act Three. Yes There is a Baby" It is a recollection of how a son and daughter interacted with their single mother. It is really a story of how two kids adapted to a mother who had severe problems. It is also a story of how remote events continue to affect people over time. One of the most surprising and consistent observations I have made in my discussions with people over time is how the relationships with parents and siblings are long lasting. They don't seem to fade away over time. Strong emotions and patterns of interpersonal interaction persist for decades if not an entire lifetime. Having no contact with your parents or siblings for prolonged periods of time usually has little effect on these dimensions. This story starts out with a teenage daughter making up a family - the McCrearys who she was babysitting for in order to escape her mother's limitations on her freedom to move around in the 1940s.
This story interested me for a number of reasons, not the least of which is the way it echoed many themes that I have heard from people as well as my own personal experience. The other important point is that it is a true story. With the current constraints on the discussion of true stories by medical professionals, I think we will need to rely more and more on true stories that are openly disclosed in the media. The eliminates any possibility of professional intervention but it allows for the emphasis of important points. In this case I have linked to the transcript because the audio file is not available until later. I agree with the disclaimer on the web site that you should actually listen to the audio file to get the full impact and hear the story in the voices of the people involved.
The story begins with the son Myron telling Ira Glass about how the rules about staying out from the family home were very different for him and his sister. He enjoyed a fair amount of freedom but his mother restricted his sister to going out to church dances. When his sister Carol is contacted, she describes a situation that is much worse. She was followed by her mother's friends. Her mother began calling her a whore at an age before she knew the meaning of the word. Whenever she was employed as a babysitter, her mother needed to know the number in order to check on her. She would also remind Carol and Myron that when their father died she got a lot of advice that she she put them both in an orphanage. She did not and described it as the biggest mistake in her life.
In order to adapt to her mother's restrictive and abusive parenting style, Carol invented a family and would say that she was babysitting for this family when she was really sleeping out on the beach or staying with friends. Mr. McCreary was an FBI agent and therefore she could not give her mother their telephone number. She was also being paid for babysitting in stocks and bonds, so there was no proof of babysitting in money.
The interesting psychiatric aspects of this story are basically threefold. Early on Myron points out that the whole concept of "imaginary people" was something that he and his sister got directly from his mother. She talked about seeing a lawyer, a psychiatrist ("psycholotrist"), and a doctor. In every case the appointments with these imaginary professionals was foreboding. She told the children that she was seeing the lawyer in order to make arrangements to put them in an orphanage. The psychiatrist told her that her children were driving her crazy. The doctor told her she was going to die.
Myron tells the story of coming home one day when he was ten years of age and his mother telling him that she was arranging for him to go to an orphanage with a local priest. He decided he would go away to school at that time, even though he knew there were any number of ways he could have sabotaged it, basically because his mother had been threatening him with an orphanage "all of my life". As a part of that process his mother wanted reassurances that he thought about her "crying my eyes out" when he was at his "fancy school". He decided from that point on (at age 10) that he would never ask his mother for anything or look to her for anything again. He had that insight when he was 30 years old.
Carol lashed out at her mother when she was about 35 years old. Her mother reacted by crying and it was the first time she had ever seen her cry. When her mother stopped crying she said that she did the best that she could have and this lead Carol to the insight:
"And I thought, oh my god, she did. Her best was so bad. Her best was so empty. But she couldn't do any better.."
Accepting that truth and recognizing the importance that her mother had to her grandmother and aunt lead Carol to modify her emotional response to her mother.
The themes in this story are important in psychotherapy and form the basis for most psychodynamic therapies. Although they never made it explicit Carol and Myron both had unique strategies to adapt to their mother's problems. This is a story that has universal appeal. Everyone has landmarks in his or her personal history when an interaction with a parent or a sibling is an organizing event in the rest of their life. The number of possible decisions and behaviors based on that event and their complexity are are well illustrated in this family history. The resilience of these two children and how they overcame childhood adversity is remarkable.
George Dawson, MD, DFAPA
Saturday, August 24, 2013
Dream recall endophenotypes?
Dreams are important part of psychiatric practice. A discussion of dreams comes up in a number of contexts ranging from diagnoses like Post Traumatic Stress Disorder to primary sleep problems like Nightmare Disorder. Dreams can be affected by substance abuse and medications. Some people are still interested in what a dream might mean or they have their own interpretation that they want to discuss. Sleep is often a source of stress to people who come in to see psychiatrists and questions about dreams frequently come up in discussion about too much sleep or too little sleep. As a result, I have done a lot of reading and study about sleep and dreams. I have the last 5 editions of Kryger, Roth and Dement's Principles and Practice of Sleep Medicine and additional texts and journals. Since I worked in a residential settings, I see people who have their sleep observed and can tell me if they have apneic episodes or behavioral problems associated with sleep and refer them for polysomnography. Whenever I ask about sleep there are a significant number of people who tell me: "I never dream."
Is it possible that a person is not dreaming at night? Since the discovery of REM sleep it is well known that this biological process and dreaming are inextricably linked. Dream researchers have determined that dream recall is influenced by a number of factors including the setting, whether a person is awakened slowly or rapidly and the sleep stage that they are awakened from. For example, awakenings form REM sleep can result in 4 or 5 dream narratives per night. Writing dreams recalled the next morning is not likely to produce that amount of content.
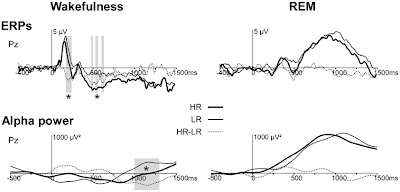
When an article suggesting a marker for differences in dream recall showed up on my Facebook feed I was naturally interested. The authors in this case had a pool of 1,000 people who completed questionnaires indicating an interest in the study. They were contacted by phone and asked the question: "on the average, how many mornings in the week do you wake up with a dream in mind?" That is an important distinction from the people I talk with because they usually say: "I dream a lot." or "I don't dream at all." For the purpose of this study the authors defined high recallers (HR) as those who recalled dream narratives or images on three mornings per week(4.42 ± 0.25 SEM dream recalls/week). Low recallers (LR) recalled narratives or images per month (0.25 ± 0.02). The subjects underwent standard polysomnography and an experimental paradigm that involved presenting a recorded voice saying first names through headphones in the alert and REM state. Event related potentials (ERPs) and alpha frequency (8-12 Hz) responses to the auditory hallucinations were recorded.
The authors summarize their data using the above graphics. The top graphic is a little confusing at first if you are used to seeing similar graphics from QEEG analysis. It is only alpha spectrum and the white lines represent occurrences of the auditory stimulus. The bottom row shows the HR - LR power and the significant difference at the Pz electrode. The black and white graphics at the bottom show ERPs and alpha power in response to first names for HR, LR, and HR-LR. In general the alpha power decreases during wakefulness and increases during REM sleep on all graphics. The HR group had a more sustained decrease in alpha power to first names at 1000 to 1200 ms during wakefulness.
The authors go on to discuss the implications of these findings including the theory that increased alpha power during REM sleep could imply microarousals without awakenings. A second hypothesis is that increased alpha power during REM sleep implies cortical deactivation rather than microarousal that would lead to decreased processing and less likelihood of awakening. The authors interpret the greater reactivity in ERPs and alpha activation in the HR state as indicating that alpha is associated with activation in sleep. They point out that the increased intrasleep wakefulness being great in HR is consistent with that observation. They go on to point out that this trait may be central to a personality organization and cognitive substrate within the brain. They pose a larger question about moving from one phenotype to the other. They make the important observation that a hippocampus needs to be in the loop for dream recall and that there may be a point where functional imaging will be able to provide that level of detail.
I could not help but wonder if dream recall is a possible endophenotype. What would happen if families were studied on their ability to recall dreams? Would there be characteristic findings on polysomnography? What would the pattern of heritability be and what would lead to transitions between phenotypes? Sleep medicine is one of the areas of psychiatry where there are clear and valid biomarkers and it would be interesting to look at those differences. In the meantime, it appears that what I have been saying to people about possible REM related dreams seems to be true based on this study. Microarousals - probably from a number of possible etiologies will probably increase dream recall of characteristic REM type dreams and you may not actually experience interrupted sleep. There is also the interesting consideration of dreaming without the hippocampus being engaged and have no dream recall on that basis.
George Dawson, MD, DFAPA
Ruby PM, Blochet C, Eichenlaub J-B, Bertrand O, Morlet D, Bidet-Caulet A (2013) Alpha reactivity to first names differs in subjects with high and low dream recall frequency. Frontiers in Psychology 4.
All of the figures in this post are from the above reference and are produced here via Creative Commons license. Please see the original article for all of the details.
Is it possible that a person is not dreaming at night? Since the discovery of REM sleep it is well known that this biological process and dreaming are inextricably linked. Dream researchers have determined that dream recall is influenced by a number of factors including the setting, whether a person is awakened slowly or rapidly and the sleep stage that they are awakened from. For example, awakenings form REM sleep can result in 4 or 5 dream narratives per night. Writing dreams recalled the next morning is not likely to produce that amount of content.
When an article suggesting a marker for differences in dream recall showed up on my Facebook feed I was naturally interested. The authors in this case had a pool of 1,000 people who completed questionnaires indicating an interest in the study. They were contacted by phone and asked the question: "on the average, how many mornings in the week do you wake up with a dream in mind?" That is an important distinction from the people I talk with because they usually say: "I dream a lot." or "I don't dream at all." For the purpose of this study the authors defined high recallers (HR) as those who recalled dream narratives or images on three mornings per week(4.42 ± 0.25 SEM dream recalls/week). Low recallers (LR) recalled narratives or images per month (0.25 ± 0.02). The subjects underwent standard polysomnography and an experimental paradigm that involved presenting a recorded voice saying first names through headphones in the alert and REM state. Event related potentials (ERPs) and alpha frequency (8-12 Hz) responses to the auditory hallucinations were recorded.
The authors summarize their data using the above graphics. The top graphic is a little confusing at first if you are used to seeing similar graphics from QEEG analysis. It is only alpha spectrum and the white lines represent occurrences of the auditory stimulus. The bottom row shows the HR - LR power and the significant difference at the Pz electrode. The black and white graphics at the bottom show ERPs and alpha power in response to first names for HR, LR, and HR-LR. In general the alpha power decreases during wakefulness and increases during REM sleep on all graphics. The HR group had a more sustained decrease in alpha power to first names at 1000 to 1200 ms during wakefulness.
The authors go on to discuss the implications of these findings including the theory that increased alpha power during REM sleep could imply microarousals without awakenings. A second hypothesis is that increased alpha power during REM sleep implies cortical deactivation rather than microarousal that would lead to decreased processing and less likelihood of awakening. The authors interpret the greater reactivity in ERPs and alpha activation in the HR state as indicating that alpha is associated with activation in sleep. They point out that the increased intrasleep wakefulness being great in HR is consistent with that observation. They go on to point out that this trait may be central to a personality organization and cognitive substrate within the brain. They pose a larger question about moving from one phenotype to the other. They make the important observation that a hippocampus needs to be in the loop for dream recall and that there may be a point where functional imaging will be able to provide that level of detail.
I could not help but wonder if dream recall is a possible endophenotype. What would happen if families were studied on their ability to recall dreams? Would there be characteristic findings on polysomnography? What would the pattern of heritability be and what would lead to transitions between phenotypes? Sleep medicine is one of the areas of psychiatry where there are clear and valid biomarkers and it would be interesting to look at those differences. In the meantime, it appears that what I have been saying to people about possible REM related dreams seems to be true based on this study. Microarousals - probably from a number of possible etiologies will probably increase dream recall of characteristic REM type dreams and you may not actually experience interrupted sleep. There is also the interesting consideration of dreaming without the hippocampus being engaged and have no dream recall on that basis.
George Dawson, MD, DFAPA
Ruby PM, Blochet C, Eichenlaub J-B, Bertrand O, Morlet D, Bidet-Caulet A (2013) Alpha reactivity to first names differs in subjects with high and low dream recall frequency. Frontiers in Psychology 4.
All of the figures in this post are from the above reference and are produced here via Creative Commons license. Please see the original article for all of the details.
Tuesday, August 20, 2013
The Psychotherapy of Psychosis
I was lucky enough to find the Practical Psychosomaticist blog recently. Jim Amos is the productive author of this excellent content that is both scholarly and creative. In a recent post and comment to my reply he said that is was good that I let people know that psychiatrists do psychotherapy. I thought I would expand upon that and more importantly the psychotherapy of severe psychiatric disorders - something I happened to learn how to do out of necessity of realizing that there needed to be a lot more communication with people than a discussion of medications and symptoms. It flows from the way psychiatrists are taught to do comprehensive assessments but these days it is not obvious.
As previously noted, my training occurred at a time when there was often open warfare between the biological psychiatrists and the psychotherapists. Even though most of the political power in departments had shifted to biological psychiatry there was still an opportunity and expectation that residents would learn how to do psychotherapy. For my last three years of training I saw at least three patients a week in hourly psychotherapy and was supervised on a 1:1 basis for each of those hours by a psychiatrist or psychologist who was also a therapist. Those sessions were frequently recorded and the supervisors listened to the audio or reviewed detailed process notes of the sessions. I had additional supervision for patients who were seen in a more standard follow up clinic setting or in a community mental health center. I had additional supervision for couples therapy, family therapy, and therapy with children and adolescents. There were ongoing seminars on psychotherapy and direct observation experts conducting psychotherapy. As a medical student, I also had a very unique experience with infant psychotherapy set up and run by two very innovative psychiatrists at the Medical College of Wisconsin.
Talking to people about their problems and how to solve them always seemed natural to me. I think that there is always an open question about whether good psychotherapists are born and not made. It makes sense that patience and empathy required are not evenly distributed across the population. When a psychiatrist learns that you may have an interest in psychiatry as a medical student, the usual areas for exploration is whether you have had personal experience with mental illness or whether one of your family members has. Even in grade school, I had extensive contact with people both inside and outside of my family with mental illness. When you have that experience it leads to an appreciation of the whole spectrum of human thought, emotion and behavior. Denying mental illness, addictions and brain disorders doesn't work. I heard the stories and personally witnessed severely disabled people being cared for at home with minimal resources.
Having that type of lifetime experience can result in a better understanding for the problem, but it does not lead to the type of technical expertise needed to talk with people in a therapeutic manner. I can recall my initial surprise when I witnessed a psychoanalyst tell a sobbing patient that he had to stop crying and try to tell us the details of his history. It seemed like the wrong thing to say, but it turned out to be highly effective in terms of changing the tenor of the interview and making it more productive. Seeing psychiatrists interact with patients and studying the theory was one of the more valuable aspects of psychiatric training and it occurred in hospital wards, clinics, research settings, texts, videos, and seminars. As the influence of psychodynamics seemed to decrease other models were also studied most notably cognitive behavioral therapy of CBT. It was similar in many ways to what had been taught as supportive psychotherapy as opposed to insight oriented psychodynamic psychotherapy. Psychotherapy supervisors practice varied schools of therapy and I mine were psychoanalysts, psychodynamicists, a Rogerian, behavioral therapists, cognitive behavioral therapists and supportive psychodynamic therapists. I eventually learned how to do an assessment and figure out what psychotherapeutic approach might be the most useful. It also provided me the skill needed to discuss past psychotherapies with patients I would be seeing in assessments. the efficacy at the time and why it might not be working several years later.
The psychotherapy of severe psychiatric disorders is a relatively new innovation. As part of my studies in the past I had read about Harry Stack Sullivan's approach and more recently (but still 40 years ago) the work of Grinker. There was some crossover with Kernberg and Kohut and their work on narcissism and borderline personality disorders. Some of the early large scale work on the psychotherapy of schizophrenia (1,2) showed that supportive psychotherapy may have an impact and that insight oriented psychodynamic therapy probably did not.
On my first job at a community mental health center, I sent a letter to the founder of Dialectical Behavior Therapy (DBT) and she sent me a copy of her research manual from field trials that were being conducted in the late 1980s. I used Beck and his associates as resources to learn about Cognitive Behavior Therapy (CBT). In the process I noted a common reference to what Beck described as the initial case of CBT in an outpatient setting with a patient who had a diagnosis of schizophrenia. Practically all of the CBT in the 1980s and 1990s was focused on depression, anxiety, and later severe personality disorders.
After three years at the community mental health center, I moved on to an inpatient setting for the next 22 years. Most of the people I saw there has severe mood and psychotic disorders or problems with severe addiction. The experience a lot of people have in these settings is not very good. It seems like a situation that is set up for containment and for many people it is. They found themselves in a crisis and many cases hospitalized for and excessive amount of emotion that fades rapidly after they leave the original situation. In other cases the emotion does not fade and they remain in a crisis in the hospital. Some people recognize that something is happening to them and they need a safe place to recover. Everyone has a theory about how they came to the hospital and whether or not they may need treatment. Inpatients on a mental health unit are often there because of legal holds based on dangerousness laws that vary from state to state.
I was able to talk with people in an unlimited manner in this setting, sometimes many times a day. I was able to engage them in a process that looked at their theories about life and about the problems that led them to the hospital. We could discuss at length what types of treatments they were interested in. I was also able to talk with them about delusions, hallucinations, and psychotherapeutic approaches to address those symptoms. At one point along the line, I noticed there was an interest in supportive psychotherapy with patients experiencing psychotic symptoms and it was summarized in 1989 in a remarkable book by Perris (3). The research evidence and theory continued to build over the next two decades with excellent courses at the annual American Psychiatric Association meeting. That included a 2009 course given by several experts in the cognitive behavior therapy of severe psychiatric disorders (4).
Decades of training and practice has undoubtedly made me a better psychotherapist. It taught me why you "practice" medicine and don't master it. It has also made me mindful of how much of the interactions between psychiatrists and the people they see, need to be seen from a psychotherapeutic perspective. That includes the environment a person is seen in and anyone else in that environment that they may encounter. It also allows for a lot of treatment flexibility that reflects a comprehensive psychiatric assessment. The best diagnostic assessment may suggest a medication is the best solution for a particular set of problems, but knowing you can also address that problem in a different way if the medication cannot be tolerated, if it fails or if the person changes their mind is a game changer.
Sometimes all it takes is an open and highly detailed conversation.
George Dawson, MD, DFAPA
1: Stanton AH, Gunderson JG, Knapp PH, Frank AF, Vannicelli ML, Schnitzer R, Rosenthal R. Effects of psychotherapy in schizophrenia: I. Design and implementation of a controlled study. Schizophr Bull. 1984;10(4):520-63. PubMed PMID: 6151245.
2: Gunderson JG, Frank AF, Katz HM, Vannicelli ML, Frosch JP, Knapp PH. Effects of psychotherapy in schizophrenia: II. Comparative outcome of two forms of treatment. Schizophr Bull. 1984;10(4):564-98. PubMed PMID: 6151246
3. Perris C. Cognitive therapy with schizophrenic patients. The Guilford Press. New York, NY, 1989.
4. Wright JH, Turkington D, Kingdon DG, Basco MR. Cognitive-Behavior Therapy for Severe Mental Illness. American PSychiatric Publishing, Inc. Washington, DC, 2009.
As previously noted, my training occurred at a time when there was often open warfare between the biological psychiatrists and the psychotherapists. Even though most of the political power in departments had shifted to biological psychiatry there was still an opportunity and expectation that residents would learn how to do psychotherapy. For my last three years of training I saw at least three patients a week in hourly psychotherapy and was supervised on a 1:1 basis for each of those hours by a psychiatrist or psychologist who was also a therapist. Those sessions were frequently recorded and the supervisors listened to the audio or reviewed detailed process notes of the sessions. I had additional supervision for patients who were seen in a more standard follow up clinic setting or in a community mental health center. I had additional supervision for couples therapy, family therapy, and therapy with children and adolescents. There were ongoing seminars on psychotherapy and direct observation experts conducting psychotherapy. As a medical student, I also had a very unique experience with infant psychotherapy set up and run by two very innovative psychiatrists at the Medical College of Wisconsin.
Talking to people about their problems and how to solve them always seemed natural to me. I think that there is always an open question about whether good psychotherapists are born and not made. It makes sense that patience and empathy required are not evenly distributed across the population. When a psychiatrist learns that you may have an interest in psychiatry as a medical student, the usual areas for exploration is whether you have had personal experience with mental illness or whether one of your family members has. Even in grade school, I had extensive contact with people both inside and outside of my family with mental illness. When you have that experience it leads to an appreciation of the whole spectrum of human thought, emotion and behavior. Denying mental illness, addictions and brain disorders doesn't work. I heard the stories and personally witnessed severely disabled people being cared for at home with minimal resources.
Having that type of lifetime experience can result in a better understanding for the problem, but it does not lead to the type of technical expertise needed to talk with people in a therapeutic manner. I can recall my initial surprise when I witnessed a psychoanalyst tell a sobbing patient that he had to stop crying and try to tell us the details of his history. It seemed like the wrong thing to say, but it turned out to be highly effective in terms of changing the tenor of the interview and making it more productive. Seeing psychiatrists interact with patients and studying the theory was one of the more valuable aspects of psychiatric training and it occurred in hospital wards, clinics, research settings, texts, videos, and seminars. As the influence of psychodynamics seemed to decrease other models were also studied most notably cognitive behavioral therapy of CBT. It was similar in many ways to what had been taught as supportive psychotherapy as opposed to insight oriented psychodynamic psychotherapy. Psychotherapy supervisors practice varied schools of therapy and I mine were psychoanalysts, psychodynamicists, a Rogerian, behavioral therapists, cognitive behavioral therapists and supportive psychodynamic therapists. I eventually learned how to do an assessment and figure out what psychotherapeutic approach might be the most useful. It also provided me the skill needed to discuss past psychotherapies with patients I would be seeing in assessments. the efficacy at the time and why it might not be working several years later.
The psychotherapy of severe psychiatric disorders is a relatively new innovation. As part of my studies in the past I had read about Harry Stack Sullivan's approach and more recently (but still 40 years ago) the work of Grinker. There was some crossover with Kernberg and Kohut and their work on narcissism and borderline personality disorders. Some of the early large scale work on the psychotherapy of schizophrenia (1,2) showed that supportive psychotherapy may have an impact and that insight oriented psychodynamic therapy probably did not.
On my first job at a community mental health center, I sent a letter to the founder of Dialectical Behavior Therapy (DBT) and she sent me a copy of her research manual from field trials that were being conducted in the late 1980s. I used Beck and his associates as resources to learn about Cognitive Behavior Therapy (CBT). In the process I noted a common reference to what Beck described as the initial case of CBT in an outpatient setting with a patient who had a diagnosis of schizophrenia. Practically all of the CBT in the 1980s and 1990s was focused on depression, anxiety, and later severe personality disorders.
After three years at the community mental health center, I moved on to an inpatient setting for the next 22 years. Most of the people I saw there has severe mood and psychotic disorders or problems with severe addiction. The experience a lot of people have in these settings is not very good. It seems like a situation that is set up for containment and for many people it is. They found themselves in a crisis and many cases hospitalized for and excessive amount of emotion that fades rapidly after they leave the original situation. In other cases the emotion does not fade and they remain in a crisis in the hospital. Some people recognize that something is happening to them and they need a safe place to recover. Everyone has a theory about how they came to the hospital and whether or not they may need treatment. Inpatients on a mental health unit are often there because of legal holds based on dangerousness laws that vary from state to state.
I was able to talk with people in an unlimited manner in this setting, sometimes many times a day. I was able to engage them in a process that looked at their theories about life and about the problems that led them to the hospital. We could discuss at length what types of treatments they were interested in. I was also able to talk with them about delusions, hallucinations, and psychotherapeutic approaches to address those symptoms. At one point along the line, I noticed there was an interest in supportive psychotherapy with patients experiencing psychotic symptoms and it was summarized in 1989 in a remarkable book by Perris (3). The research evidence and theory continued to build over the next two decades with excellent courses at the annual American Psychiatric Association meeting. That included a 2009 course given by several experts in the cognitive behavior therapy of severe psychiatric disorders (4).
Decades of training and practice has undoubtedly made me a better psychotherapist. It taught me why you "practice" medicine and don't master it. It has also made me mindful of how much of the interactions between psychiatrists and the people they see, need to be seen from a psychotherapeutic perspective. That includes the environment a person is seen in and anyone else in that environment that they may encounter. It also allows for a lot of treatment flexibility that reflects a comprehensive psychiatric assessment. The best diagnostic assessment may suggest a medication is the best solution for a particular set of problems, but knowing you can also address that problem in a different way if the medication cannot be tolerated, if it fails or if the person changes their mind is a game changer.
Sometimes all it takes is an open and highly detailed conversation.
George Dawson, MD, DFAPA
1: Stanton AH, Gunderson JG, Knapp PH, Frank AF, Vannicelli ML, Schnitzer R, Rosenthal R. Effects of psychotherapy in schizophrenia: I. Design and implementation of a controlled study. Schizophr Bull. 1984;10(4):520-63. PubMed PMID: 6151245.
2: Gunderson JG, Frank AF, Katz HM, Vannicelli ML, Frosch JP, Knapp PH. Effects of psychotherapy in schizophrenia: II. Comparative outcome of two forms of treatment. Schizophr Bull. 1984;10(4):564-98. PubMed PMID: 6151246
3. Perris C. Cognitive therapy with schizophrenic patients. The Guilford Press. New York, NY, 1989.
4. Wright JH, Turkington D, Kingdon DG, Basco MR. Cognitive-Behavior Therapy for Severe Mental Illness. American PSychiatric Publishing, Inc. Washington, DC, 2009.
Saturday, August 17, 2013
Straight Talk About the Government Dismantling Care for Serious Mental Illness
The ShrinkRap blog posted a link to an E. Fuller Torrey and D.J. Jaffe editorial in the National Review about how the government has dismantled mental health care for serious mental illnesses and some of the repercussions. Since I have been saying the exact same thing for the past 20 years, they will get no argument from me. Only in the theatre of the absurd that passes for press coverage of mental illness and psychiatry in this country can this subject be ignored and silenced for so long. It was obviously much more important to see an endless stream of articles trying to make the DSM-5 seem relevant for every man. The stunning part about the Newtown article is the commentary about what government officials responsible for policy have actually been saying about it.
The authors waste very little time examining the sequence of events in the Obama administration following the Newtown, Connecticut mass shooting. President Obama initially stated he would "make access to mental health care as easy as access to guns." and set up a Task Force under Vice President Biden to make recommendations. The authors argue that the agency that was consulted, the Substance Abuse and Mental Health Services Administration (SAMHSA) promotes a model of treating mental illness that has no proven efficacy, does not discuss serious mental illnesses in its planning document, ignores effective treatments for serious mental illnesses and actually goes so far as to fund programs that block the implementation of effective treatment programs. In an example of the obstruction of effective programming by SAMHSA funded programs following the Newtown mass shooting:
"But, alas, the situation is even worse. SAMHSA does not merely ignore effective treatments for individuals with severe mental illness. It also funds programs that attempt to undermine the implementation of such treatments at the state and county level. One such program is the Protection and Advocacy program, a $34 million SAMHSA program that was originally implemented to protect patients in mental hospitals from abuse. It was kidnapped by civil-liberties zealots and has been used to block the implementation of assisted outpatient treatment, funding efforts to undermine it in at least 13 states. For example in Connecticut, following the Newtown massacre of schoolchildren, the federally funded Connecticut Office of Protection and Advocacy for Persons with Disabilities testified before a state-legislature working group in opposition to the proposed implementation of a proposed law permitting court-ordered outpatient treatment for individuals with severe mental illness who have been proven dangerous. The law did not pass." (page 3, par 2.)
In other words, a SAMHSA funded program was opposed to a law in Connecticut that could potentially reduce violence from persons with severe mental illness.
SAMHSA administrators are quoted at times in the article. Any quote can be taken out of context but the characterizations of severe mental illness as "severe emotional distress", "a spiritual experience" and "a coping mechanism and not a disease" reflect a serious lack of knowledge about these disorders. The idea that "the covert mission of the mental health system ...is social control" is standard antipsychiatry philosophy from the 1960s. How is it that after the Decade of the Brain and the new Obama Brain Initiative we can have a lead federal agency that apparently knows nothing about the treatment of serious mental illnesses? How is it that apart from some fairly obscure testimony, no professional organizations have pointed this out? How is it in an era where governments at all levels seem to demand evidence based care, that a lead agency on mental health promotes treatment that has no evidence basis and ignores the treatment that is evidence based?
Having been a long time advocate for the prevention of violence by the treatment of severe mental illnesses my comments parallel those of the authors. Inpatient bed capacity in psychiatry has been decimated. They point out that there are only 5% of the public psychiatry beds available that there were 50 years ago. It is well known that people with mental illnesses are being incarcerated in record numbers and some of the nation's county jails have become the largest psychiatric institutions. Where are all of the civil liberties advocates trying to get the mentally ill out of jail?
Only a small portion of the beds available can be used for potentially violent or aggressive patients and that number gets much smaller if a violent act has actually been committed. Most of the bed capacity in this country is under the purview of some type of managed care organization and that reduces the likelihood of adequate assessment or treatment. The discharge plan in some cases is to just put the patient on a bus to another state.
Community psychiatry is a valuable unmentioned resource in this area. In most of the individual cases mentioned in this article, the lack of insight into mental illness or anosognosia is prominent. It is not reasonable to expect that a person with anosognosia will follow up with outpatient appointments or even continue to take a medication that treats their symptoms into remission. Active treatment in the community by a psychiatrists and a team who knows the patient and their family is the best way to proceed. All of this active treatment has been cost shifted out of insurance coverage and is subject to budget cuts at the county and state level.
Civil commitment laws and proceedings are probably the weakest link in treatment. Further cost shifting occurs and violent patients often end up aggregating in the counties with the most resources. Even while they are there, many courts hear (from a budgetary perspective) that they are committing too many people and the interpretation of the commitment law becomes more liberal until there is an incident that leads to the interpretation tightening up again. Bureaucrats involved often become libertarians and suggest that commitment can occur only if an actual violent incident has happened rather than the threat of violence.
Although Torrey and Jaffe are using the extreme situation of violence in the seriously mentally ill to make their point, the majority of the seriously mentally ill are not violent. They need the same resources. It has been thirty years of systematic discrimination against these people, their families and the doctors trying to treat them that has led to these problems. I pointed out earlier on this blog the problem I have with SAMHSA and the use of the term "behavioral health". The problems with SAMHSA and current federal policy are covered in this article and I encourage anyone with an interest to read it. If history is any indication, I don't expect anything serious to come of the criticism. I anticipate a lot of rhetorical blow back at Dr. Torrey. But as a psychiatrist who has worked in these environments for most of my career, his analysis of the problem is right on the mark.
George Dawson, MD, DFAPA
E. Fuller Torrey & D.J. Jaffe. After Newtown. National Review Online.
White House. Now Is The Time. The President's plan to protect our children and our communities by reducing gun violence. January 16, 2013.
The authors waste very little time examining the sequence of events in the Obama administration following the Newtown, Connecticut mass shooting. President Obama initially stated he would "make access to mental health care as easy as access to guns." and set up a Task Force under Vice President Biden to make recommendations. The authors argue that the agency that was consulted, the Substance Abuse and Mental Health Services Administration (SAMHSA) promotes a model of treating mental illness that has no proven efficacy, does not discuss serious mental illnesses in its planning document, ignores effective treatments for serious mental illnesses and actually goes so far as to fund programs that block the implementation of effective treatment programs. In an example of the obstruction of effective programming by SAMHSA funded programs following the Newtown mass shooting:
"But, alas, the situation is even worse. SAMHSA does not merely ignore effective treatments for individuals with severe mental illness. It also funds programs that attempt to undermine the implementation of such treatments at the state and county level. One such program is the Protection and Advocacy program, a $34 million SAMHSA program that was originally implemented to protect patients in mental hospitals from abuse. It was kidnapped by civil-liberties zealots and has been used to block the implementation of assisted outpatient treatment, funding efforts to undermine it in at least 13 states. For example in Connecticut, following the Newtown massacre of schoolchildren, the federally funded Connecticut Office of Protection and Advocacy for Persons with Disabilities testified before a state-legislature working group in opposition to the proposed implementation of a proposed law permitting court-ordered outpatient treatment for individuals with severe mental illness who have been proven dangerous. The law did not pass." (page 3, par 2.)
In other words, a SAMHSA funded program was opposed to a law in Connecticut that could potentially reduce violence from persons with severe mental illness.
SAMHSA administrators are quoted at times in the article. Any quote can be taken out of context but the characterizations of severe mental illness as "severe emotional distress", "a spiritual experience" and "a coping mechanism and not a disease" reflect a serious lack of knowledge about these disorders. The idea that "the covert mission of the mental health system ...is social control" is standard antipsychiatry philosophy from the 1960s. How is it that after the Decade of the Brain and the new Obama Brain Initiative we can have a lead federal agency that apparently knows nothing about the treatment of serious mental illnesses? How is it that apart from some fairly obscure testimony, no professional organizations have pointed this out? How is it in an era where governments at all levels seem to demand evidence based care, that a lead agency on mental health promotes treatment that has no evidence basis and ignores the treatment that is evidence based?
Having been a long time advocate for the prevention of violence by the treatment of severe mental illnesses my comments parallel those of the authors. Inpatient bed capacity in psychiatry has been decimated. They point out that there are only 5% of the public psychiatry beds available that there were 50 years ago. It is well known that people with mental illnesses are being incarcerated in record numbers and some of the nation's county jails have become the largest psychiatric institutions. Where are all of the civil liberties advocates trying to get the mentally ill out of jail?
Only a small portion of the beds available can be used for potentially violent or aggressive patients and that number gets much smaller if a violent act has actually been committed. Most of the bed capacity in this country is under the purview of some type of managed care organization and that reduces the likelihood of adequate assessment or treatment. The discharge plan in some cases is to just put the patient on a bus to another state.
Community psychiatry is a valuable unmentioned resource in this area. In most of the individual cases mentioned in this article, the lack of insight into mental illness or anosognosia is prominent. It is not reasonable to expect that a person with anosognosia will follow up with outpatient appointments or even continue to take a medication that treats their symptoms into remission. Active treatment in the community by a psychiatrists and a team who knows the patient and their family is the best way to proceed. All of this active treatment has been cost shifted out of insurance coverage and is subject to budget cuts at the county and state level.
Civil commitment laws and proceedings are probably the weakest link in treatment. Further cost shifting occurs and violent patients often end up aggregating in the counties with the most resources. Even while they are there, many courts hear (from a budgetary perspective) that they are committing too many people and the interpretation of the commitment law becomes more liberal until there is an incident that leads to the interpretation tightening up again. Bureaucrats involved often become libertarians and suggest that commitment can occur only if an actual violent incident has happened rather than the threat of violence.
Although Torrey and Jaffe are using the extreme situation of violence in the seriously mentally ill to make their point, the majority of the seriously mentally ill are not violent. They need the same resources. It has been thirty years of systematic discrimination against these people, their families and the doctors trying to treat them that has led to these problems. I pointed out earlier on this blog the problem I have with SAMHSA and the use of the term "behavioral health". The problems with SAMHSA and current federal policy are covered in this article and I encourage anyone with an interest to read it. If history is any indication, I don't expect anything serious to come of the criticism. I anticipate a lot of rhetorical blow back at Dr. Torrey. But as a psychiatrist who has worked in these environments for most of my career, his analysis of the problem is right on the mark.
George Dawson, MD, DFAPA
E. Fuller Torrey & D.J. Jaffe. After Newtown. National Review Online.
White House. Now Is The Time. The President's plan to protect our children and our communities by reducing gun violence. January 16, 2013.
Tuesday, August 13, 2013
Lessons on Medical Pricing and Service from My Toyota Dealer
I really like my Toyota dealer. They advertise that they are one of the most successful dealerships in Minnesota and I have no reason to doubt that. Everytime I end up waiting in their customer service area there are anywhere from 30 - 50 people waiting with me. Everybody checks out at the same cashier. Everybody hears the conversation between the customer and the service manager and basically the fact that the customers seem uniformly satisfied and all of their problems have been addressed. As I sat there today looking at a long line of satisfied customers I thought of a comparison with medicine.
Let me start off discussing my parallel by saying that I have always been a proponent of medical pricing being one of the most significant problems in health care. The example that I frequently post is the difference between an MRI scan of the cervical spine in Japan ($150) to the cost of the same scan in the US ($1200). But in other posts I have compared the costs of formulary to non-formulary drugs and the steep discounts that frequently apply to services by physicians. Economist Ed Lotterman discusses the effects of price discrimination in health care at this link and the reason why health care companies do it. They make more money even though they end up charging much higher prices to the people who can afford it the least. There are many other subtle (if you don't think about it too long) ways of rationing medical services to provide a high volume low quality product that really does not address the problems that most people want. As an example, I was shocked in 1987 when I encountered for the very first time a physician who refused to answer any questions about a "second" problem. He was obviously annoyed when I asked him about a medical concern that was not identified as the reason for the appointment, even though I am certain he could have answered the question in two minutes. The people at my Toyota dealer frequently have two or three or even five problems and the service manager calmly explains what has been done or what the cost will be in the event of a major repair.
As I thought more about it, my name was eventually called and I walked over to pick up the car and review what had been done. I thought I might need a price list for a comparison, so I walked back out into the service area and talked to a service manager who looked like he was about my age. I asked him for a price list and thought about what kind of reaction that would get in a medical clinic - not just the price list but asking additional questions after the appointment with the doctor was officially over. He enthusiastically replied: "No problem at all sir. It is tricky to find on our web site. Let me show you how to get it there. And let me print it out for you. My usual printer doesn't do a good job, so let me send it to a better network printer." Within a minute it was in my hand. None of the gasping and eye rolling that you might expect in a medical clinic.
What is a fair comparison? I decided against emergency departments. Car repairs are generally not life or death, even though a lot of people with non-emergency problems end up staying in emergency departments for a long time. I decided that urgent care and primary care clinics were problems the best comparisons. The Toyota dealer has three levels of maintenance based on mileage or time:
The price list shows all of the specific tasks that this dealer does for car maintenance and the task list is longer as the price increases. I can't post any medical comparisons because the actual price that you will pay is unknown. If you are insured, your insurance company generally negotiates prices with a clinic that are generally much lower than you would pay if they billed you their usual retail price. Practically all physician billing would occur at the Green or Blue Service level. As I look at the Yellow service, it is strictly maintenance without the services of a diagnostician. How many times have you had to see a doctor in order to get lab tests or an x-ray? There are a list of things you can get from Toyota without seeing a mechanic.
What about affordability? Everybody in the service center today was driving a Toyota ranging from essentially new to at least 6 years old (the age of my car). Everyone with a fairly new car wants to keep the warranty current by doing the suggested maintenance. There will always be some outliers who never change their oil, but let's assume that people generally want to protect their investment for at least 6 years or 100,000 miles. What is the trade off in terms of investment at risk driving service fees? If we look at the current per capita health care expenditure in the US it stands at $8,233 per person per year. According to the Kaiser Family Foundation in 2012, the average cost of insurance for a family was $15,745 with the worker paying $4, 316. Worker only coverage averaged $5,615 per year with the annual cost to the worker of $951. The current cost of health care for a retired couple at age 65 with Medicare is estimated to be $220,000, not including nursing home care.
The 5 or 6 year cost of health insurance for a family costs the same amount as just about any brand new Toyota on the lot. There are a couple of potential questions about the value of the purchase. If we are considering non emergency and routine medical care, does the purchaser of health insurance get the same value as the purchaser of a new Toyota? Or is medical insurance purchased strictly to protect the family against bankruptcy associated with a medical catastrophe? And do your get the same level of service?
On the service level, I don't think that primary care or urgent care clinics can compare to my Toyota dealer. I just learned today that they are open until midnight and they see all of the walk ins who want to be seen at all times. Their pricing is completely transparent and affordable to everyone who pays the same amount for health insurance that they would pay to purchase a new Toyota every 6 years. That is basically any family purchasing health insurance. Technology is a frequent argument to justify the high cost of American medicine, but people purchasing hybrids are the beneficiaries of a $6 billion research project by Toyota that put them at the forefront of that technology and made it as cost effective as purchasing any other new car. Technological innovation like that in medicine rarely translates into a cost effective solution for patients that quickly.
Without government mandates and the threat of bankruptcy, I think health insurance would be a very difficult product to sell based solely on market factors and the actual service you get for the money. That is what health care companies like to call value. I guess the bright side is that we all don't have to purchase an insurance product that would allow us to get a new car. It is hard to imagine how bad that product and the service of that product would be.
George Dawson, MD, DFAPA
Disclosure: Not a stockholder in Toyota. My only interest in Toyota is in keeping my car running well.
References:
Ed Lotterman. Price discrimination: Free market at work. November 15, 2009.
Ed Lotterman. Trip to hospital illustrates complexities of health care pricing. December 23, 2012.
Let me start off discussing my parallel by saying that I have always been a proponent of medical pricing being one of the most significant problems in health care. The example that I frequently post is the difference between an MRI scan of the cervical spine in Japan ($150) to the cost of the same scan in the US ($1200). But in other posts I have compared the costs of formulary to non-formulary drugs and the steep discounts that frequently apply to services by physicians. Economist Ed Lotterman discusses the effects of price discrimination in health care at this link and the reason why health care companies do it. They make more money even though they end up charging much higher prices to the people who can afford it the least. There are many other subtle (if you don't think about it too long) ways of rationing medical services to provide a high volume low quality product that really does not address the problems that most people want. As an example, I was shocked in 1987 when I encountered for the very first time a physician who refused to answer any questions about a "second" problem. He was obviously annoyed when I asked him about a medical concern that was not identified as the reason for the appointment, even though I am certain he could have answered the question in two minutes. The people at my Toyota dealer frequently have two or three or even five problems and the service manager calmly explains what has been done or what the cost will be in the event of a major repair.
As I thought more about it, my name was eventually called and I walked over to pick up the car and review what had been done. I thought I might need a price list for a comparison, so I walked back out into the service area and talked to a service manager who looked like he was about my age. I asked him for a price list and thought about what kind of reaction that would get in a medical clinic - not just the price list but asking additional questions after the appointment with the doctor was officially over. He enthusiastically replied: "No problem at all sir. It is tricky to find on our web site. Let me show you how to get it there. And let me print it out for you. My usual printer doesn't do a good job, so let me send it to a better network printer." Within a minute it was in my hand. None of the gasping and eye rolling that you might expect in a medical clinic.
What is a fair comparison? I decided against emergency departments. Car repairs are generally not life or death, even though a lot of people with non-emergency problems end up staying in emergency departments for a long time. I decided that urgent care and primary care clinics were problems the best comparisons. The Toyota dealer has three levels of maintenance based on mileage or time:
Yellow Service
|
Every 4 months
|
$72.95
|
Green Service
|
Every 12 months
|
$219
|
Blue Service
|
Every 24 months
|
$379
|
Friday, August 9, 2013
Don Draper loses it - Can he be saved?
Don Draper, the main character in AMC's MadMen is without a doubt the most complicated character I have ever seen on television. I have often thought about whether or not I have seen him over the years. What would be the most likely way that he would come to the attention of a psychiatrist? I can remember several years ago he went in to see his primary care physician and was told that he had hypertension (150/100). The prescribed course of action was a combination of a barbiturate and reserpine. Being seen as a complication of that therapy might be one way. He also has demonstrated that he has a progressive problem with alcohol. Everyone on MadMen drinks at work, and it is typically hard liquor. At one level it seems to be part of the Madison Avenue culture, but Don has taken it many steps beyond that to overt intoxication and vomiting in the office. Even in the 1960s, this behavior could result in a period of detoxification and residential treatment. If he really was mixing alcohol with barbiturates that is a setup for an accidental overdose or a withdrawal seizure.
Another avenue to consultation might have to do with his philandering behavior. Over the course of the show he has had two wives and he has had extramarital affairs in both marriages. During his second marriage, he befriends a cardiothoracic surgeon in his building. He admires this man and he seems like the only real friendship that Draper has been interested in over the course of the series. That does not deter him from sleeping with the surgeon's wife. During his previous marriage, he had affairs with numerous women resulting in his wife finding out and on one occasion he was punched in the face by an irate husband. None of that has had much of an impact on his lifestyle that consists of drinking a lot at work and frequently using work as an excuse to neglect his wife and family and continue extramarital sex.
Whenever I think of philandering, I think of Frank Pittman's work that I read fresh out of residency training. In outpatient practice, anxious and depressed persons have two major sources of stress - their job and their significant relationship. It is fairly common to see significant others and spouses during the treatment of an individual. The usual requests are for a basic explanation of the diagnosis and treatment plan, but in more complicated circumstances an analysis of the spouses behavior. I think that Pittman may have seen Don Draper as a subtype of philanderer that he refers to as a "hostile philanderer" who is not empathic toward women. A more psychodynamic approach might suggest that Draper is narcissistic and that might be the driving force behind his lack of empathy. In either case, the therapy focused on this problem is complicated and requires skills that focus on neutrality and a focus on the goals of therapy rather than an endless description of the problem.
A more recent approach might employ a model of sexual addiction rather than looking at the problem as repetitive marital infidelity. One of the conceptualizations of the problem is that it can be a behavioral addiction like food and gambling and that it involves and activates the same neurobiological substrates that addictive drugs and alcohol do. Some authors have developed criteria sets for sexual addiction based on the characteristics of substance use disorders, but this disorder is not listed in the main DSM or the section on "Conditions for Further Study." Some people will come in for assessment based on someone telling them that they have a sex addiction or their participation in 12-step recovery groups with that focus. Experts in the field have produced reviews of psychotherapy and pharmacotherapy that might be useful for this problem, but at this point most psychiatrists would see this as an issue for psychotherapy and would have reservations about the medical treatment of a model that has not been widely accepted.
There is also a more biological approach to infidelity. Some people may present with requests for a medication that has decreased libido as a side effect or a medication that produces that result by its physiological effect.
In the season 6 finale, Don Draper is trying to seal an advertising deal with Hershey. The staff knows they are swimming up stream, because Hershey has outstanding brand recognition and packaging. Don has to sell them on a campaign that takes their advertising to a new level. He tells a poignant story about mowing the lawn as a kid and his father taking him to the store later so that he could buy a Hershey bar. That candy symbolizing the bond between a father and son and a bridge to those memories in the past. His associates in the room are beaming. They think he has hit it out of the park. A few minutes later, he tells everyone in the room that the story he has just told never happened. He says he was raised in a "whorehouse" and one of the prostitutes would ask him to go through the trousers of her clients, looking for extra money. He would get some of that change and buy a Hershey bar. When he ate it he was living vicariously like the kid in his original story.
Can Don Draper be saved? In a way he already has. He was at a clear disadvantage in terms of childhood trauma and adapted to that by becoming somebody who he was not and trying to consciously block out that previous existence. We get a glimpse of one of his strategies from an earlier scene. I think that from an artistic point of view the writers are saying that he cannot. He could no longer suppress the truth about himself at a critical juncture in his career. That is true not only with his clients and coworkers but also with his children. In the final scene of the season, he is standing with his children in front of the whorehouse where he was raised. His daughter looks at him for some kind of reaction.
From a psychiatric standpoint the answer is a qualified yes. Certainly any psychiatrist could come up with a plan that might address some of the areas highlighted above. It would take a comprehensive formulation of his problems. Framing the problem as simple anxiety or depression or some other DSM-5 diagnosis is an obvious mistake. In many practice settings that pressure is there. There is also the chance that he might walk into an AA meeting for any number of reasons and make some changes to get his life back on track. He might even get some advice from a friend or coworker about a particular aspect of his problems that he might decide to pursue and that could lead to some changes. The main drawback to advice from a peer is that he has no peers and no close friends. Human consciousness is complex and there are many roads to change.
George Dawson, MD, DFAPA
Frank Pittman. Private Lies - Infidelity and the Betrayal of Intimacy. WW Norton and Company, New York, 1989.
Shoptaw SJ. Sexual addiction in Ries R, Fiellin DA, Miller SC, Saitz R. Principles of Addiction Medicine. 4th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2009: pp 519-530.
Another avenue to consultation might have to do with his philandering behavior. Over the course of the show he has had two wives and he has had extramarital affairs in both marriages. During his second marriage, he befriends a cardiothoracic surgeon in his building. He admires this man and he seems like the only real friendship that Draper has been interested in over the course of the series. That does not deter him from sleeping with the surgeon's wife. During his previous marriage, he had affairs with numerous women resulting in his wife finding out and on one occasion he was punched in the face by an irate husband. None of that has had much of an impact on his lifestyle that consists of drinking a lot at work and frequently using work as an excuse to neglect his wife and family and continue extramarital sex.
Whenever I think of philandering, I think of Frank Pittman's work that I read fresh out of residency training. In outpatient practice, anxious and depressed persons have two major sources of stress - their job and their significant relationship. It is fairly common to see significant others and spouses during the treatment of an individual. The usual requests are for a basic explanation of the diagnosis and treatment plan, but in more complicated circumstances an analysis of the spouses behavior. I think that Pittman may have seen Don Draper as a subtype of philanderer that he refers to as a "hostile philanderer" who is not empathic toward women. A more psychodynamic approach might suggest that Draper is narcissistic and that might be the driving force behind his lack of empathy. In either case, the therapy focused on this problem is complicated and requires skills that focus on neutrality and a focus on the goals of therapy rather than an endless description of the problem.
A more recent approach might employ a model of sexual addiction rather than looking at the problem as repetitive marital infidelity. One of the conceptualizations of the problem is that it can be a behavioral addiction like food and gambling and that it involves and activates the same neurobiological substrates that addictive drugs and alcohol do. Some authors have developed criteria sets for sexual addiction based on the characteristics of substance use disorders, but this disorder is not listed in the main DSM or the section on "Conditions for Further Study." Some people will come in for assessment based on someone telling them that they have a sex addiction or their participation in 12-step recovery groups with that focus. Experts in the field have produced reviews of psychotherapy and pharmacotherapy that might be useful for this problem, but at this point most psychiatrists would see this as an issue for psychotherapy and would have reservations about the medical treatment of a model that has not been widely accepted.
There is also a more biological approach to infidelity. Some people may present with requests for a medication that has decreased libido as a side effect or a medication that produces that result by its physiological effect.
In the season 6 finale, Don Draper is trying to seal an advertising deal with Hershey. The staff knows they are swimming up stream, because Hershey has outstanding brand recognition and packaging. Don has to sell them on a campaign that takes their advertising to a new level. He tells a poignant story about mowing the lawn as a kid and his father taking him to the store later so that he could buy a Hershey bar. That candy symbolizing the bond between a father and son and a bridge to those memories in the past. His associates in the room are beaming. They think he has hit it out of the park. A few minutes later, he tells everyone in the room that the story he has just told never happened. He says he was raised in a "whorehouse" and one of the prostitutes would ask him to go through the trousers of her clients, looking for extra money. He would get some of that change and buy a Hershey bar. When he ate it he was living vicariously like the kid in his original story.
Can Don Draper be saved? In a way he already has. He was at a clear disadvantage in terms of childhood trauma and adapted to that by becoming somebody who he was not and trying to consciously block out that previous existence. We get a glimpse of one of his strategies from an earlier scene. I think that from an artistic point of view the writers are saying that he cannot. He could no longer suppress the truth about himself at a critical juncture in his career. That is true not only with his clients and coworkers but also with his children. In the final scene of the season, he is standing with his children in front of the whorehouse where he was raised. His daughter looks at him for some kind of reaction.
From a psychiatric standpoint the answer is a qualified yes. Certainly any psychiatrist could come up with a plan that might address some of the areas highlighted above. It would take a comprehensive formulation of his problems. Framing the problem as simple anxiety or depression or some other DSM-5 diagnosis is an obvious mistake. In many practice settings that pressure is there. There is also the chance that he might walk into an AA meeting for any number of reasons and make some changes to get his life back on track. He might even get some advice from a friend or coworker about a particular aspect of his problems that he might decide to pursue and that could lead to some changes. The main drawback to advice from a peer is that he has no peers and no close friends. Human consciousness is complex and there are many roads to change.
George Dawson, MD, DFAPA
Frank Pittman. Private Lies - Infidelity and the Betrayal of Intimacy. WW Norton and Company, New York, 1989.
Shoptaw SJ. Sexual addiction in Ries R, Fiellin DA, Miller SC, Saitz R. Principles of Addiction Medicine. 4th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2009: pp 519-530.
Monday, August 5, 2013
Asthma Endophenotypes? Their Implications for Psychiatry
Asthma is an annoying and sometimes fatal disease. I have first hand experience with it because I have had asthma for at least 40 years. Like many of my personal medical afflictions that I have posted about on this blog it was initially missed and not treated. According to recent studies, that is still a common experience. When I was a teenager, wheezing when mowing the lawn was apparently considered a normal reaction. When I developed a more systemic reaction right in a physician's office, my parents were taken into an adjacent room and advised that it was apparently all "in my head" and it was some sort of psychosomatic reaction. The psychosomatic reaction responded well to epinephrine injections and diphenhydramine. Even when I was in medical school the treatment of asthma was shaky. I was taking theophylline pills twice a day for several years and the patients I began treating for exacerbations of chronic obstructive pulmonary disease were all on aminophylline drips and corticosteroids. We all had to memorize those protocols and of course know the mechanism of action (now invalidated) that was based on Sutherland's Nobel Prize winning work on cyclic AMP. Today theophylline is considered a tertiary option for uncontrolled asthma rather than a first line treatment.
As a fourth year medical student, I presented a very well received seminar on "slow reacting substance of anaphylaxis" or SRS-A now known to be a mixture of leukotrienes. Eventually the treatment of asthma changed and glucocorticoid inhalers became the treatment of choice for a while. As any primary care physician or asthmatic patient knows - no two asthmatic patients are the same. As an example, peak flow meters are routinely used to measure asthmatic control. No matter how badly I am wheezing, I can always max out that peak flow meter. Asthma is a complex disease with varied presentations and the current treatment algorithms are complex with varied medications.
The diagnostic criteria of asthma seem relatively straightforward and are listed in the table below:
Medicine texts have traditionally used breakpoints in the above parameters to distinguish mild, moderate and severe asthma. Despite what seem to be clear diagnostic criteria a recent review (8) in the New England Journal of Medicine states: "Most patients with asthma have mild persistent disease which tends to be underdiagnosed, undertreated, and inadequately controlled." The reference cited in that review points out that only 1 in 7 patients achieved good control of their asthma.
There has been a sudden surge in research on asthma phenotypes, endotypes, and endophenotypes. Endophenotypes are subtypes of a particular phenotype that are thought to have a common pathophysiological mechanism or in the case of psychiatry a biochemical, neurophysiological, neuropsychological maker that allows for the subclassification. If you have attended any serious psychiatric genetics course in the past decade you have probably heard about endophenotypes. Gottesman and Gould published a widely cited paper in the American Journal of Psychiatry in 2003 discussed the concept and its application in psychiatry. There have been 132 references to papers on endophenotype in the Schizophrenia Bulletin alone, including a special theme issue.
A group of 5 asthma endotypes have been suggested by Corren (7). He uses the definition of endotype as "a subtype of a condition defined by a distinct pathophysiological mechanism." The classification was a consensus of experts looking at clinical characteristics, biomarkers, lung physiology, genetics, histopathology, and treatment response. The following 5 endotypes were identified.
George Dawson, MD, DFAPA
1: Barranco P, Pérez-Francés C, Quirce S, Gómez-Torrijos E, Cárdenas R, Sánchez-García S, Rodríguez-Fernández F, Campo P, Olaguibel JM, Delgado J; Severe Asthma Working Group of the SEAIC Asthma Committee. Consensus document on the diagnosis of severe uncontrolled asthma. J Investig Allergol Clin Immunol. 2012;22(7):460-75; quiz 2 p following 475. PubMed PMID: 23397668.
2: Simon T, Semsei AF, Ungvári I, Hadadi E, Virág V, Nagy A, Vangor MS, László V, Szalai C, Falus A. Asthma endophenotypes and polymorphisms in the histamine receptor HRH4 gene. Int Arch Allergy Immunol. 2012;159(2):109-20. doi: 10.1159/000335919. Epub 2012 May 30. PubMed PMID: 22653292.
As a fourth year medical student, I presented a very well received seminar on "slow reacting substance of anaphylaxis" or SRS-A now known to be a mixture of leukotrienes. Eventually the treatment of asthma changed and glucocorticoid inhalers became the treatment of choice for a while. As any primary care physician or asthmatic patient knows - no two asthmatic patients are the same. As an example, peak flow meters are routinely used to measure asthmatic control. No matter how badly I am wheezing, I can always max out that peak flow meter. Asthma is a complex disease with varied presentations and the current treatment algorithms are complex with varied medications.
The diagnostic criteria of asthma seem relatively straightforward and are listed in the table below:
Diagnosis of Asthma (see additional details in National Heart, Lung and Blood Institute reference) and reference 8 below:
|
1. Recurrent symptoms of airflow
obstruction or airway hyperresponsiveness (eg. wheezing, chest tightness, cough, shortness of breath.)
2. Objective assessment as
evidenced by:
A.
Airflow obstruction as least
partially reversible by inhaled short acting beta2 agonists as demonstrated by any of the
following:
-
Increase in FEV1 of ≥ 12% from
baseline
-
Increase in predicted FEV1 of ≥ 10%
from baseline
-
Increase in PEF (liters/minute) of ≥ 20% from baseline
B. Diurnal variation in PEF of more than 10%
C. No other causes of obstruction
|
FEV1 = forced expiratory volume in 1 second (liters)
PEF = peak expiratory flow
|
A group of 5 asthma endotypes have been suggested by Corren (7). He uses the definition of endotype as "a subtype of a condition defined by a distinct pathophysiological mechanism." The classification was a consensus of experts looking at clinical characteristics, biomarkers, lung physiology, genetics, histopathology, and treatment response. The following 5 endotypes were identified.
Asthma Endotypes
|
|
Allergic Asthma
|
Childhood onset, hypersensitivity to airborne allergens, Th2 mediated inflammatory process, eosinophilia of blood and airways, inhaled corticosteroids less effective, IgE antagonists are more effective.
|
Aspirin exacerbated respiratory disease (AERD)
|
Chronic rhinosinusitis with nasal polyps, severe bronchospasm if NSAIDs are ingested, marked blood and airway eosinophilia, increased expression of leukotriene C4 synthetase, response to cysteinyl leukotriene receptor antagonists and 5-lipoxyenase inhibitors
|
Allergic bronchopulmonary mycosis (ABPM)
|
Colonization of airways by Aspergillus fumigatus, increased fungal specific IgE and IgG, elevated blood eosinophil and total IgE levels, elevated airway eosinophils and neutrophils, requires oral corticosteroids and antifungals
|
Late Onset Asthma
|
Pulmonary function testing is more impaired than allergic asthma, marked eosinophilia in blood and airways, need oral corticosteroids. May be mediated by IL-5.
|
Cross country skiing induced asthma (CCSA)
|
Triggered by exposure to cold dry air and intense exercise, not usually due to allergies, inflammatory infiltrate consists of lymphocytes, macrophages, and neutrophils rather than eosinophils, airway remodeling with thickened basement membrane, not usually responsive to inhaled corticosteroids.
|
The tables on diagnosis and endophenotype are remarkable for their parallels with psychiatric diagnosis and research. The available endotypes do probably not capture all of the clinical scenarios of asthma because patient behavior is a significant factor. The endotype classification of asthma by experts is interesting in that it includes a treatment response dimension and this has been avoided in psychiatry at the diagnostic level.
Like mental illnesses, asthma is a complex polygenic disease with considerable clinical heterogeneity. Using endophenotype approaches very similar to the approaches that have been applied to the study of schizophrenia offers the hope that classification and treatments of subtypes will be more effective and the connection between the genetics of the illness, pathophysiological mechanisms, and subtype will become more apparent. Although the parallels with mental illness are clear, asthma researchers and clinicians treating asthma have the advantage in that they can proceed without the stigmatization that only accompanies psychiatric disorders and psychiatrists.
Like mental illnesses, asthma is a complex polygenic disease with considerable clinical heterogeneity. Using endophenotype approaches very similar to the approaches that have been applied to the study of schizophrenia offers the hope that classification and treatments of subtypes will be more effective and the connection between the genetics of the illness, pathophysiological mechanisms, and subtype will become more apparent. Although the parallels with mental illness are clear, asthma researchers and clinicians treating asthma have the advantage in that they can proceed without the stigmatization that only accompanies psychiatric disorders and psychiatrists.
George Dawson, MD, DFAPA
1: Barranco P, Pérez-Francés C, Quirce S, Gómez-Torrijos E, Cárdenas R, Sánchez-García S, Rodríguez-Fernández F, Campo P, Olaguibel JM, Delgado J; Severe Asthma Working Group of the SEAIC Asthma Committee. Consensus document on the diagnosis of severe uncontrolled asthma. J Investig Allergol Clin Immunol. 2012;22(7):460-75; quiz 2 p following 475. PubMed PMID: 23397668.
2: Simon T, Semsei AF, Ungvári I, Hadadi E, Virág V, Nagy A, Vangor MS, László V, Szalai C, Falus A. Asthma endophenotypes and polymorphisms in the histamine receptor HRH4 gene. Int Arch Allergy Immunol. 2012;159(2):109-20. doi: 10.1159/000335919. Epub 2012 May 30. PubMed PMID: 22653292.
3: Matteini AM, Fallin MD, Kammerer CM, Schupf N, Yashin AI, Christensen K,
Arbeev KG, Barr G, Mayeux R, Newman AB, Walston JD. Heritability estimates of
endophenotypes of long and health life: the Long Life Family Study. J Gerontol A
Biol Sci Med Sci. 2010 Dec;65(12):1375-9. doi: 10.1093/gerona/glq154. Epub 2010
Sep 2. PubMed PMID: 20813793; PubMed Central PMCID: PMC2990267.
4: Bisgaard H, Bønnelykke K. Long-term studies of the natural history of asthma
in childhood. J Allergy Clin Immunol. 2010 Aug;126(2):187-97; quiz 198-9. doi: 10.1016/j.jaci.2010.07.011. Review. PubMed PMID: 20688204.
5: Chan IH, Tang NL, Leung TF, Huang W, Lam YY, Li CY, Wong CK, Wong GW, Lam CW.
Study of gene-gene interactions for endophenotypic quantitative traits in Chinese
asthmatic children. Allergy. 2008 Aug;63(8):1031-9.
doi: 10.1111/j.1398-9995.2008.01639.x. PubMed PMID: 18691306.
doi: 10.1111/j.1398-9995.2008.01639.x. PubMed PMID: 18691306.
6: Thompson MD, Takasaki J, Capra V, Rovati GE, Siminovitch KA, Burnham WM, Hudson TJ, Bossé Y, Cole DE. G-protein-coupled receptors and asthma endophenotypes: the cysteinyl leukotriene system in perspective. Mol Diagn Ther. 2006;10(6):353-66. Review. PubMed PMID: 17154652.
7. Corren J. Asthma phenotypes and endotypes: an evolving paradigm for classification.
Discov Med. 2013 Apr;15(83):243-9. PubMed PMID: 23636141.
8. Bel EH. Clinical Practice. Mild asthma. N Engl J Med. 2013 Aug 8;369(6):549-57.
doi: 10.1056/NEJMcp1214826. PubMed PMID: 23924005
7. Corren J. Asthma phenotypes and endotypes: an evolving paradigm for classification.
Discov Med. 2013 Apr;15(83):243-9. PubMed PMID: 23636141.
8. Bel EH. Clinical Practice. Mild asthma. N Engl J Med. 2013 Aug 8;369(6):549-57.
doi: 10.1056/NEJMcp1214826. PubMed PMID: 23924005
Subscribe to:
Posts (Atom)