Pages
▼
Tuesday, October 2, 2018
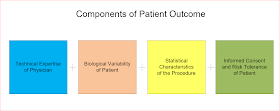
Components of Patient Outcome
It is a good idea to go back and take a look at some basic components that predict patient outcome in medical (including surgical) treatment. There is a skewed representation of practically all medical information that is portrayed in the press. A big part of that misrepresentation comes back to missing what the real components are that determine the outcome. I have listed a few of what I consider to be the major components in the above diagram and will take a look at each one in order.
Technical expertise of the physician is obvious in surgical and other invasive procedures. Henry Marsh covered it in a book on his career as a neurosurgeon (1). He discussed the process of surgery but also the unpredictable results. An operation may have seemed flawless but the patient ends up with a postoperative complication that had to be due to the surgery and dies or is permanently disabled. I have discussed the issue with neurosurgeons myself and directly observed them in action. There are clear differences in skill level and operative outcomes that appear to be based strictly on manual dexterity and coordination. There are differences based on the number of procedures that are done. Expertise is easy to conceptualize at a manual level.
Psychiatrists on the other had usually balk when I refer to the technical expertise required in the field. The clearest example in training is learning about inpatient psychiatry before proceeding to outpatient clinics. Most psychiatric trainees just don't know enough as first year residents to proceed to an outpatient clinic and start to treat anyone who walks through the door. The inpatient setting provides the training necessary to address emergencies first. Outpatient skills can be built on that foundation. An associated issue is how much you need to know. If you are immersed in medical settings like hospitals, you probably need to know about a broad range of medical and surgical conditions and how they can lead to or complicate treatment of psychiatric disorders. That knowledge base includes a broad range of basic sciences and the updates relevant for the field. Expertise in psychiatry also encompases the interpersonal dimension. Psychiatrists should be the medical specialists that have the highest level of competency in the interpersonal dimension and how their personal feelings toward patients can complicate care. That requires a significant level of training and expertise.
Biological variability is poorly understood by nonphysicians. The best examples are allergic reactions to medications and severe idiosyncratic reactions like liver failure or kidney failure in response to a medication. But they can also be more common on a population wide basis and mediated though a number of mechanisms. The variability has to do with both the way the medication is absorbed and metabolized and also specific effects that occur at the tissue level. In some cases this leads to clinical trials where the results do not seem that impressive (antidepressants, radiofrequency ablation for atrial fibrillation) but where there is a clear consensus that the intervention works.
Every procedure in medicine whether it is a prescription, a surgical procedure or a medical device is characterized by a study. The quality of those studies varies in terms of design and statistical analysis. The usual goals of early studies is to gain FDA approval for release into the market in the US and elsewhere. In the process of the safety and efficacy studies, quire a lot is learned about the drug characteristics applied over a larger population. That data is applied toward describing that population based effect to the physicians who will eventually be prescribing the medical or procedure. In some cases there are considerable political cross currents that can affect the straightforward statistical data as in the case of coronary artery bypass grafting or the use of beta blockers for hypertension or preventatively post acute MI. There is currently an active debate about prostate screening and the burdens and harm done by screening, but at the same time there are clinical trials that show prostate cancer survival is improved by radical prostatectomy (RP) - but that there is no difference between standard RP versus robotic surgery. It is doubtful that the statistical facts of the procedure will ever be far from the expertise domain.
The final critical outcome parameter is the patient's ability to consent. It is not an easy task to hear about current medications or interventions with imperfect results and decide what the best course of action is. Apart from the cognitive analysis, there is an emotional component of having a significant illness. There is also the requisite ability to tolerate risk. Practically no medical interventions are risk free but some have much higher risks that others. The risk ranges from death or disability to an allergic reaction or long list of possible side effects. The risk of not taking the medication or having the procedure done can also be significant including death.
One of the best examples in the literature about the importance of the patient related component of these outcome variables was Kurt Gödel. He was a renowned mathematician and logician who suffered from severe medical problems including gastric ulcers, prostatic hypertrophy with severe lower urinary tract obstruction who either postponed or refused treatment to the point where he was near death or in severe distress. He had a severe urinary tract obstruction and refused surgery to correct the obstruction. He elected to remain catheterized for a period of 4 years until the time of his death. He eventually died of starvation in a hospital refusing to eat because he believed his food had been poisoned and at the time of his death weighed 65 pounds (he was 5'6" in height). Gödel was one of the geniuses of the 20th century who experienced problems that consistently and adversely affected his health. Shortly before his own death and Gödel's death his friend economist Oskar Morgenstern made this observation in his diary (from reference 2; p 251) after a phone call from Gödel:
"It is hard to describe what such a conversation means for me; here is one of the most brilliant men of our century, greatly attached to me ..... [who] is clearly mentally disturbed, suffering from some kind of paranoia, expecting help from me, and I am unable to extend it to him. Even when I was mobile and tried to help him I was unable to accomplish anything. [Now,] by clinging to me - and he has nobody else, that is quite clear - he adds to the burden I am carrying." - July 10, 1977.
Morgenstern died 16 days later of metastatic prostate cancer.
The main takeaway message from this brief commentary of variables affecting patient outcome is that it is a complicated process. There needs to be open communication about the uncertainty at every step of the way. In the informed consent discussion (that should always occur) there should be enough information exchanged so that the patient/decision maker has a clear idea of the risk involved.
Even then, the most intelligent decision makers can fail.
George Dawson, MD, DFAPA
References:
1: Henry Marsh. Do No Harm. Thomas Dunne Books, St. Martin's Press; 2014.
2: John W. Dawson. Logical Dilemmas: The Life and Work of Kurt Gödel. Natick, MA: AK Peters, LTD; 1997: 229-253.
This is a great way of thinking of patient outcomes. I have never heard it in such an organized, coherent, and digestible way. Thanks for this.
ReplyDeleteThanks for reading it and your comments Victor.
Delete