I recently participated in an Addiction Medicine Journal Club where the presenter used a novel presentation technique called Abstract Attack. The result in terms of group process was so good – I thought I would present it here for further exposure and comment. As a qualifier I would add that I have not spoken directly to the creators and base this post on my direct participation in the format and the PowerPoint from the creators (1) and the presentation I attended (2).
Standard presentations in medicine and other academic
fields typically consist of a single presenter charged with presenting data or
techniques for information and some discussion.
The expertise of the presenter and role of the audience varies considerably. For example, in my Biochemistry course in
medical school the seminars were focused on techniques and concepts. The course
instructor would typically choose a paper or two on a clear topic like
diphtheria or cholera toxin. The
presenter was responsible for presenting those two papers at the minimum with
additional papers as necessary. That was in 1978 – well before the Internet and
online resources. All papers had to be obtained as hard copies from the medical
library. We would have two or three biochem
seminars per week – so there were always a number of presentations to prepare
for and the information content was variable.
My pharmacology course used a similar format but slide presentations
were allowed. Since there was no digital presentation software – the slides had
to all be shot on 35 mm film and projected.
That was the standard until well after I completed residency and started
working. Eventually presentation software was developed making the job much
easier.
Microsoft PowerPoint eventually evolved into the standard
presentation format but it is not without controversy. In the past 15 years there have been numerous
presentations and papers written about everything that people consider to be
wrong with PowerPoint. That criticism is
highly variable such as too little to too much information, being more boring
that an extemporaneous lecture, problematic graphics and format on the slides,
reading the slides, and competing software that claims to produce a better
presentation. The competition angle is
an interesting one because in the beginning I bet on (and paid for) two
competing products before it became apparent that PowerPoint would be the
winner. It is difficult to win against a product that is installed on most
business computers in the country.
My person bias is that I like the PowerPoint format. The product is greatly improved in the past
decade and can also be used to produce graphics for other applications. I have attended seminars and courses on this
to improve the approach with PowerPoint from a graphical standpoint and my
slide making has improved considerably. I think it is very useful to put up graphics
and texts that provide more information to the audience while I am free
associating to the slides. To me the main difference between a verbal only
lecture and a PowerPoint presentation is the greater informational content. Consider that TED Talks are supposed to
present a great idea in 18 minutes. I am
supposed to be presenting many ideas and facts in 50-50 minutes. That is what a
PowerPoint presentation is for.
The doesn’t mean that all high information PowerPoints are
successful. The speaker still has to be fairly good in both presentation style
and engaging the audience. The audience has to be well behaved and focused on the
content. I was giving a fairly detailed lecture on alcohol use and the latest
World Health Organization (WHO) report on the scope of the problem. There was a student in the audience checking
the data on my slides (taken directly from the report) about what he could find
on his phone and arguing about it. There are always unexplained emotional
reactions in the crowd and in some cases, people get up and leave – even when
nothing presented is really controversial. We have all attended presentations
when the discussion starts with the dreaded: “I don’t have a question but I
would like to comment……” followed by a 10 minute long irrelevant digression.
When you experience all of those occurrences at conferences
and lectures, you can’t help thinking: “Is there a better way to keep all of
this on track?” Limiting the discussion, not taking questions, or having all of
the questions submitted and moderated are certainly possibilities that I have
seen used successfully. But I was recently exposed to a presentation format
that structured the responses right in PowerPoint and that led to a focused
high-quality discussion. I will explain
the format and hopefully provide a good example of how to approach the problem.
The method is called Abstract Attack and it was
apparently devised by members of the University of Minnesota North Memorial
Family Medicine Program. Rene Crichlow,
MD, FAAFP is credited with the concept and in the PowerPoint I acquired her
co-presenters were Tanner Nissly, DO, and Jason Ricco, MD, MPH (1). I first experienced this approach in a
journal club teleconference (2) that was presented by Ian Latham, MD a resident
from the UMN program on an article about lorazepam versus phenobarbital for
alcohol detoxification based on a 2021 paper (3).
The overall goals for this presentation format are from
family practice curriculum. In the
initial presentation the authors use the Accreditation Council for Graduate
Medical Education (ACGME) requirements for scholarship to develop the Abstract
Attack approach. Those scholarship requirements
can be found in the document on common requirements for all residency programs.
Interested readers can find the specifics in a box graphic on page 26 of this
document. It is an elaboration of the
way all physicians are trained to critique scientific and clinical studies and
the application of the studies to clinical work. The primary goals of Abstract Attack (1) are
cited as:
1. "Abstract
Attack", a method to provide uniform acquisition of skills and
knowledge
2. Sufficient for a
practicing clinician to confidently, participate in efficient and effective
Evidence Based critique of the medical literature at the point of care
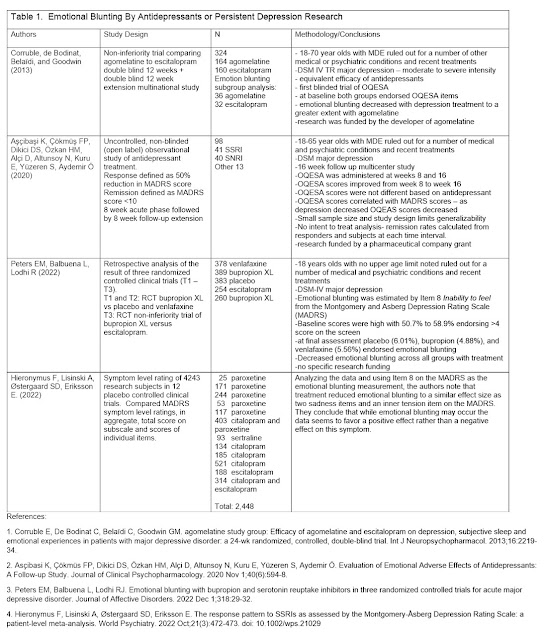
The overall process is described as patient rather than disease oriented and adhering to a critical appraisal pathway that answers the questions: Pertinent to your patients’ care? Consistent or Inconsistent? Valid or Invalid? The structured order of presentation is given in the slide below:
In the session I attended (2) the author discussed the overall goal of being able to present journal articles with the assumption that nobody else has read it. He proceeded to illustrate how the presented information could be discussed at the level of every slide by the following prompts (that he incorporated in every slide):
What is interesting about this?
What is concerning about this?
What do I need to know more about?
I will illustrate with a few slides from a recent JAMA paper (5). The slides cueing the discussion might look something like this.
Additional slides are provided on the methods and
results. That is followed by a slide
with questions exploring how the study potentially impacts clinical practice
and what additional information or studies may be needed. Supplemental slides can contain information
on the scientific and statistical concepts used in the paper. The emphasis is clearly proceeding from the clinical
trials to clinical practice.
My direct experience with this format is that there was
timely discussion every step of the way.
Senior clinicians and physicians can add commentary early in the process
about what they see are being important about the study. The audience is clearly engaged without every
reading the paper. The presenter can add critical information in supplementary
slides at the end after the discussion on how impactful the information is on
clinical practice and what else might be needed.
Overall, I thought this was a breakthrough in how to make
these presentations efficiently when everyone’s time is at a premium. Dr.
Crichlow and her colleagues are to be congratulated. I have made a comparison slide below.
George Dawson, MD, DFAPA
References:
1: Crichlow R,
Nissly T, Ricco J. Trans-formative
Journal Club Experience as a Basis for a Longitudinal EBM Curriculum. PowerPoint Presentation. Accessed on October 16, 2022.
2: Latham I.
Phenobarbital Versus Lorazepam for Management of Alcohol Withdrawal Syndrome: A
Retrospective Cohort Study Addiction Medicine Journal Club. PowerPoint Presentation. August 2, 2022.
3: Hawa F, Gilbert
L, Gilbert B, Hereford V, Hawa A, Al Hillan A, Weiner M, Albright J, Scheidel
C, Al-Sous O. Phenobarbital Versus Lorazepam for Management of Alcohol
Withdrawal Syndrome: A Retrospective Cohort Study. Cureus. 2021 Feb
11;13(2):e13282. doi: 10.7759/cureus.13282. PMID: 33728215; PMCID: PMC7949711.
4: Accreditation
Council for Graduate Medical Education (ACGME).
Common Requirements Currently In Effect.
7/1/2022: https://www.acgme.org/what-we-do/accreditation/common-program-requirements/ Accessed on 10/19/2022.
5: Florian J, van
der Schrier R, Gershuny V, Davis MC, Wang C, Han X, Burkhart K, Prentice K,
Shah A, Racz R, Patel V, Matta M, Ismaiel OA, Weaver J, Boughner R, Ford K,
Rouse R, Stone M, Sanabria C, Dahan A, Strauss DG. Effect of Paroxetine or
Quetiapine Combined With Oxycodone vs Oxycodone Alone on Ventilation During
Hypercapnia: A Randomized Clinical Trial. JAMA. 2022 Oct 11;328(14):1405-1414.
doi: 10.1001/jama.2022.17735. PMID: 36219407.
Supplementary Info:
Any slide above can be enlarged by clicking on it.