I quit my job last Thursday night at about 9:30 PM. My term of employment was officially over at
the close of business today – Tuesday January 19, 2021. It happened during an exchange of fairly
terse emails with my immediate supervisors. Those emails occurred in the
context of a flurry of daytime emails that were critical and could easily be
interpreted as making me look as bad as possible. I have no plans to disclose
the nature of these conflicts or the content of those emails.
I know from experience that responding to the content of
these messages at face value and ignoring the meaning is a mistake that you can
never recover from. It is also a mistake because it assumes that the people
representing corporations have a genuine interest in you as a human being. People – no matter how good they are – are
always expendable to the modern corporation and there is no better example than
healthcare companies. I also believe that because several of my previous supervisors
said it directly to my face.
I was very clear in my email that the
reason I was quitting was a decision that happened that day. It is good to maintain clear boundaries when
it comes to these decisions. Sometimes
there is a lot of emotion involved and when that happens a lot of charged rhetoric. By the time 9:30 PM rolled around – I was
very cool. I had been in a heightened
emotional state all day. That tends to
happen when people say things about me that are not true and try to make it seem
like I am personality disordered. By
heightened emotional state I generally mean a hyperadrenergic state. Anxiety, stress, tachycardia rather than anger. That distressed state resolved as soon as I
realized the situation with the administrators was hopeless and all I had to do
was quit. As soon as that occurred, I
was able to relax and fall asleep like nothing had happened. A complete cessation of the emails was also
helpful.
That decision in the last paragraph was very important to
me. As the son of a railroad engineer, I
was socialized to be very wary of any special interest (whether it was a
company or a union) that could affect your work or personal freedom. Being very
clear on what you want to experience was all part of that socialization and at
times it was fairly stark. There is a long learning curve. I did not really become an expert at it until
I walked away from a previous job 12 years ago. I thought I was going to work
at that job my entire career and retire – much like my Dad viewed his railroad job.
I recall my father showing me the front of his Brotherhood
of Locomotive Firemen and Engineers trade paper and angrily making the
following statement:
“Do you see this big house? That is where the President of the Union
Lives! Do you think he cares about what
happens to us?” (Fairly
certain my Dad would have probably used much more colorful language but I don’t want to embellish).
Of course not, Dad.
I heard a radio program several years ago about first-generation
white-collar workers from blue collar families.
According to the speaker, they were much less likely to integrate their
business lives into their social lives.
The example given was that they would not invite their boss over for
dinner. But nobody stated the reason –
and that is basic working-class distrust of management. Second-generation white-collar workers may
also have a much higher tolerance for bullshit than blue collar folks. In my
family of origin, bullshit was not a humorous or value free word. It was generally a pejorative.
There is also the way you exist in the work place. Some people need the social aspect at work for
many reasons including reassurance that they are in good standing. A lot of us like to keep our heads down, do
the work, and not comment on all of the social behavior in the workplace. We don’t want to hear about other peoples’
problems – not because we don’t care about our fellow man but because we were
raised to mind your own business.
I am in the latter category and find that it works very well. People I work with over time know they will
be treated fairly and they know that I am very loyal to them. That may be another reason why I react so
strongly when people make things up about me.
The boundaries are significantly less clear in a white
collar setting, especially with institutional rules and training on what
constitutes civility. Unless you are fired precipitously and escorted out by
security there are the superficial niceties – even if you are dying the death
of a thousand cuts. “Oh you’re leaving?
We are sorry to see you go! Let’s have some cake in the break room! Don’t be a
stranger!” All the while stories are
being spun about what happened to either make it seem like you were basically a
jerk or you were never there in the first place. At a previous job I endured
months of gaslighting and abuse. At one
point I asked my primary care doc for a prescription for a beta blocker just to
control my heart rate and blood pressure from the stress. I joke about taking
them like M&Ms, but at the time it was no joke. That was not going to happen again.
When I think about the range of normal and pathological
workplace dynamics I always come back to the work of the late Peter
Drucker. He was described as the world’s
greatest management thinker. One of
his key concepts is the knowledge worker. In other words, employees who were trained in
a profession – in many cases an independent professional. Drucker pointed out
that these employees need to be managed differently by virtue of the fact that
they know more about the business than their boss does. Further that they are not managed for widget
production as productivity. In the
current healthcare environment, the most highly trained employees are
physicians. They are treated like production workers and clerical workers rather
than knowledge workers and in many cases replaced en masse by other
workers who can do some of what they do.
As an example, I recently did a search through my health care system
looking for a primary care internist in the event that my current internist
retires. The search pulled up 50
practitioners and only 2 were physicians.
The way health care systems deal with knowledge workers is to either get
rid of them or ration them. All part of
the unending death spiral of low-quality care in America.
One of the big human-interest stories of the pandemic is
that medical school applications are apparently way up. The reason given is the presence of Anthony
Fauci, MD in the news. In all of these
clips, only a tiny fraction of Dr. Fauci’s expertise and body of work is
visible but his demeanor and consistent references to science make him easy to
identify with. He is a physician that others want to emulate. The problem for all of these
prospective medical students is that there are very few places any more where a
physician can practice at the top of what they were trained to do. There are practically no physician
environments that maintain an academic focus that was common in every setting that I trained at in the 1980s.
Apart from the workplace politics and all of the completely
unnecessary stress it produces my immediate consideration is finding a new
job. I do not need to work. I could
simply retire. When I was working a
burnout inpatient job – I fantasized about retiring early just to escape the
place. Since then, I have concluded that
I am still at the top of my game and have an excellent skillset to offer people
with significant psychiatric problems. These
services are clearly needed. In addition, I have a unique approach to
psychiatry that I think needs to be out there to counter the low-quality
checklist approach that has very little to do with psychiatry. The problem is finding the ideal environment
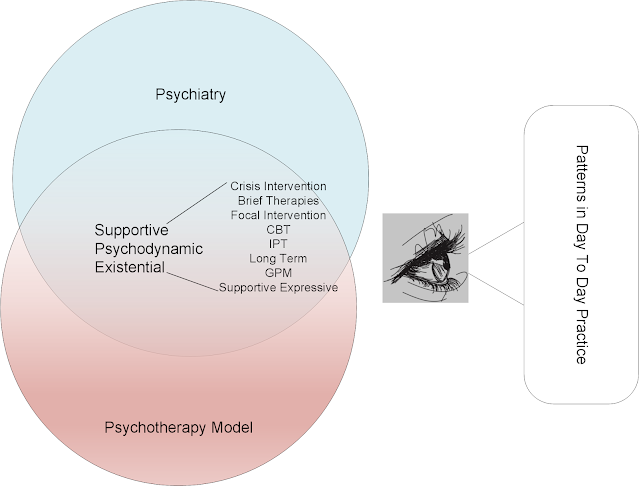
to utilize that skill set. The figure
below gives an example of the practice environments that I have worked in and
whether my skill set was utilized or marginalized.
Drawing on that experience whether I get another job at this point or retire depends on the following factors:
1: Malpractice
coverage: I could easily set up a private practice in the era of telepsychiatry
but any psychiatrist planning to retire at some point needs tail coverage. That is malpractice insurance through the
statute of limitations for malpractice in the state you practice in. In Minnesota that is three years and would
costs tens of thousands of dollars.
That’s right - three years paying out a good deal of money on the
hypothetical that you might be sued during that time – whether you have previously
been sued or not.
2: Practice
environment: The graphic below shows how
badly the practice environment has deteriorated with the invention of managed
care, pharmacy benefit managers, and an expensive labor-intensive electronic
health record (EHR). That means I have a
choice again between setting up my own office, hiring staff, buying and setting
up and EHR or going to work for a managed care company who has all of this but
expects me to become a template monkey and fill out 20-30 patient visit
templates per day. I use the term template
monkey out of respect for one of my colleagues who is a proceduralist and
told me at lunch one day that is what she had become. She presented it as a joke, but it is a
fairly depressing self-observation from one of the most highly trained MDs in
the profession and the hours it takes her to complete arbitrary forms that have
nothing to do with quality medical care.
While I am at it my inpatient and outpatient workflow is 30 minutes per patient follow up and 60-90 minutes for initial evaluations with some time in between for documentation and coordination of care. That coordination of care typically involves acquiring and reviewing records and speaking to the patient’s treating physicians. I also need to be able to dictate all of the notes rather than type them in to a template. I have yet to see dictation software work seamlessly enough, but I have seen transcription companies with industrialized versions do excellent job for a very low price. I need help from clerical resources, I don’t need to become a clerical worker.
3: Availability of
necessary equipment, tests, and specialists:
For 22 years I worked in a very collegial environment that was full of
medical and surgical consultants. I knew all of them and they knew me. There was mutual respect and plenty of
information exchange. We consulted informally
at lunch. If I had a patient with
complex problems – I would just do the evaluation, order all of the tests, make
a diagnosis and then call a consultant if necessary. I have not been in that environment for a
while and I am not used to leaving things hanging and depending that people
will follow my advice and see a cardiologist.
In fact, I know that people rarely follow through. Anyone who suggests that you can just kick
the can down the road, doesn’t really understand the practice of medicine
or psychiatry. In order to offer
treatment, I need to determine that the patient does not have serious
underlying illness and that I am not making any pre-existing conditions worse. So, I need a medically intensive
environment. I thought I could do without
it but that was a big mistake.
Apart from my current situation, this is a problem across the entire country. Medically trained psychiatrists and neuropsychiatrists are unable to find suitable practice environments. Managed care companies are quick to offer appointments with any prescriber for anxiety and depression or even more complicated problems. This is a system wide problem even though there is no organized system of mental health care in the country. If I get lucky and find the resources I need – the system will be lucky – at least in the geographic area where I can serve patients. It is a basic fact that the necessary practice environment for most medically intensive psychiatrists has become a fantasy in the United States. That fantasy could easily be remedied by a national work force supplying psychiatrists with what they need and paying them as employees.
If I am not fortunate enough to find the right practice environment
– I will be enjoying retirement and to me a lot of that will still be studying
psychiatry, medicine, and science. It is
what I do and I enjoy doing it.
Old patterns of behavior die hard – at least for me.
George Dawson, MD, DFAPA
Supplementary 1:
My official last day was the close of business on Tuesday
January 19 and that is why this is being posted later that same day.
I do wish my fellow former employees the very best (including
the administrators) and hope that everything goes well for them. After I announced my resignation, I received
at least 50 very positive emails telling me that they liked working with me and
wishing me well in the future. In many
cases they were extremely complimentary. We all worked together to help people
solve very difficult problems in a highly constrained environment. We were
typically successful to some degree. For all of the compliments all that I can
say is thank you and:
“The light that shines on me – shines on you”.