There is a paper that just came out (1) that I consider a
must-read for all psychiatrists. Some
experts might qualify that and say that it is only necessary to know the
subjects if you are treating the medically ill, the elderly, pediatric
patients, patients with cardiovascular disease, or patients with cardiac risk
factors. The problem with those qualifications is that you have to know
everything in this paper (and others) in order to make that determination.
Beyond that you have to been trained in how to determine if your patient is
seriously ill or not. In the case of all medical specialists, serious illness generally
means treatment by another specialist or in a more intensive setting. For that
reason, the cardiac aspects of care in this paper are required knowledge.
Three of the authors of this paper are cardiologists, two
are psychiatrists, and one is a clinical pharmacist. They have produced a very
practical document on identifying problems with tachycardia, QTc prolongation,
sudden cardiac death, myocarditis, and dilated cardiomyopathy. They provide very specific endpoints and
suggest some basic intervention that can be done before the patient is referred
to cardiology. Examples would be assessment of tachycardia, suggested treatment
thresholds, common treatment interventions like beta-blockers and calcium
channel blockers, and referral to cardiology if there is a progression to other
cardiac symptoms, nonresponse to the initial therapy, or an arrhythmia beyond
sinus tachycardia. They provide similar guidance on the other common conditions
and relate them to second-generation antipsychotics (SGAs).
All of the authors are from the United Kingdom. I am not familiar with the standard settings
for practicing psychiatry in the UK, but in the US there is a high degree of
variability. For example, in practicing on inpatient settings it is not a
problem to order ECGs or even stat ECGs. Echocardiograms and other imaging
studies of the heart are easily obtained as well as cardiology consultation. In
a previous inpatient setting where I practiced, I requested a cardiology
consultation for a young woman with a QTc of 520 ms who required treatment with
antipsychotic medications. She was seen immediately and an electrophysiology study
was done. After that study I was advised by cardiology that I could safely
treat the patient with olanzapine. At the other end of the spectrum, I know
there are psychiatrists reading this who have no access ECGs, medical testing,
or cardiology consultants. They are often practicing in an office that lacks a
sphygmomanometer or staff routinely checking patient vital signs. Many of those
office settings are essentially nonmedical and any psychiatrist practicing there
- would need to bring in their own equipment and probably take their own vital signs. A basic standards would be that every practice setting for psychiatry in the country should have
the tools to make the measurements recommended in this paper, but I am not aware that any standard like that exists.
The second obstacle to realizing these guidelines is the way
electronic health records (EHR) are set up. Major organizations and the EHR
companies themselves produce templates that are typically designed for business
purposes rather than medical quality. A visit to a psychiatrist in that
organization results in that template being filled out with a business rather
than a clinical focus. In other words, sections of bullet points are completed
based on what coders believe will capture the necessary billing from insurance
companies. One of the key sections is often the review of systems (ROS). Because
these documents are not designed by physicians and there are no uniform
standards, a functional review systems is often not there. In the case of
cardiac symptoms, there needs to be a clear section that encompasses all the
symptoms described by the authors in this paper. As an example, take a look at
the cardiac symptomatology that I recorded in this post and the modified
extended review of systems that I typically ask patients about.
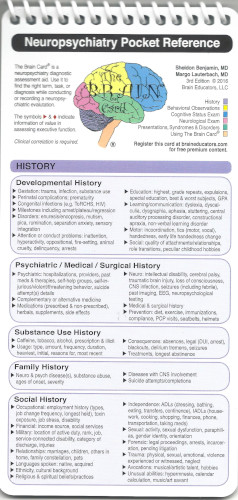
Any inpatient or outpatient assessment done by a psychiatrist should include a thorough medical history, a review of systems that is focused on medical rather than psychiatric systems, a set of vital signs including noting whether or not the cardiac rhythm or pulse is regular or irregular and a further description of the irregularity. A focal exam for additional heart and lung findings and determination of pulses and peripheral edema may be indicated. The take home point is that this history taking combined with a few additional findings should be all that is necessary to order further tests like an ECG, refer for an acute assessment, or refer to a primary care physician or cardiologist for further assessment. If the patient is being followed for the metabolic complications of SGAs, there may already be a fasting blood glucose, and lipid profile in the chart to assess additional risk factors. Over the years I have also found that recording a theory about why I think the patient is symptomatic is also very useful. In my practice that has ranged from medication side effects to an acute myocardial infarction.
Any inpatient or outpatient assessment done by a psychiatrist should include a thorough medical history, a review of systems that is focused on medical rather than psychiatric systems, a set of vital signs including noting whether or not the cardiac rhythm or pulse is regular or irregular and a further description of the irregularity. A focal exam for additional heart and lung findings and determination of pulses and peripheral edema may be indicated. The take home point is that this history taking combined with a few additional findings should be all that is necessary to order further tests like an ECG, refer for an acute assessment, or refer to a primary care physician or cardiologist for further assessment. If the patient is being followed for the metabolic complications of SGAs, there may already be a fasting blood glucose, and lipid profile in the chart to assess additional risk factors. Over the years I have also found that recording a theory about why I think the patient is symptomatic is also very useful. In my practice that has ranged from medication side effects to an acute myocardial infarction.
With those issues we can proceed to consider the assessments
and treatments recommended by this group. I am not going to repeat the content
of the paper here. I recommend that any
interested psychiatrist or psychiatric resident get a copy of this paper and
study it in detail if you are not already familiar with the concepts. I will
list a few of the points that I found to be interesting after doing these
assessments for a long time.
The section on the QTc interval was interesting because the
authors provide very clear guidance on measuring QTc, the problems with that
measurement, and very clear guidelines on what to do about that measurement.
They cite the threshold for stopping or reducing treatment with QTc prolonging
agents as an interval greater than 500 ms or relative increase of greater than
60 ms. They also use the American Heart Association definitions of prolonged as QTc > 450 ms in men and > 460 ms in women. They point out that the most common
calculation of QTc (Bazett’s formula) overcorrects heart rates greater
than 100 BPM and they suggest that other formulae may be used for that situation. Like
many psychiatrists I have ordered hundreds of ECGs for determining baseline
cardiac conduction. The vast majority have been normal. The ones that were not - were typically unrelated to the medication I was prescribing. Many conduction
abnormalities were related to increasing age and latent cardiac problems. The
other common scenario where I am concerned about cardiac conduction is
polypharmacy. It is possible for a person to be taking multiple medications for
psychiatric indications - all of which may affect cardiac conduction. The drug
interaction software for most EHRs as a very low threshold for this type of
interaction.
The myocarditis section of this paper was very interesting.
In Table 1 - the authors included prevalence figures for myocarditis in the
same table where they documented the prevalence of tachycardia for each
medication. The figures are based on isolated case reports. The review the
controversy about clozapine and widely variable reports of incidence. The
incidence quoted for Canada and the USA was 0.03%. Different criteria used to
diagnose myocarditis was considered an important point of variance. A set of
clinical criteria is provided in the paper as well as when to refer to a
cardiologist. In addition to the ECG, serum troponin, C-reactive protein,
echocardiogram, and cardiac MRI are considered. The referral indicators
included elevated troponin, CRP, and abnormalities at echocardiogram. My
interpretation is that psychiatrists in the US who have access to those
measures and ready access to cardiologists could potentially use those markers.
The most reasonable approache is to be able to recognize the symptoms of
myocarditis clinically and be able to refer the patient to cardiology were most
of the testing could occur. The clinical description of myocarditis in the paper
sounded very similar to typical viral myocarditis with chest pain, dyspnea, flu-like
illness, fever, and fatigue. These are nonspecific symptoms especially during
influenza season. The clinician has to have a high index of suspicion based
on treatment with clozapine. The paper contains an ECG tracing of saddle
-shaped ST elevation considered to be a finding consistent with myocarditis. It
was visible in most leads.
The approach to dilated cardiomyopathy was very similar in
terms of recognizing the symptoms of congestive heart failure and the necessary
investigations. There was guidance and when to request an echocardiogram based
on BNP and in NT-ProBNP measures as well as when referral to cardiology was
indicated. The standard of care in the US is the psychiatrist recognizing what is
happening but not treating dilated
cardiomyopathy. In most clinical with limited resources, this is a good reason to have a referral relationship with a primary care clinic - especially one that can do the testing on site. There are many primary care and even urgent care clinics that cannot do the testing suggested in this paper.
In the case of myocarditis and dilated cardiomyopathy, the
question of whether a patient should be re-challenged if they need the offending
medication and their underlying cardiac condition has improved. The authors
suggest close consultation with a cardiologist at that point. Given the data my
own practice has been to not re-challenge with the offending medication but to
try a different treatment modality. The concern in the article is that the
patient’s ability to function from a psychiatric standpoint may require use of
that specific medication. I do not think that enough is known about the outcome
of either condition to resume the original medication, but if favorable
outcome studies or case reports exist, I might revise that opinion.
All things considered this is an outstanding article on the
cardiotoxicity of SGAs. The graphics in the paper also excellent with
management flow diagrams and well-designed tables. The authors restate that cardiotoxicity is
very low. It is the job of every
psychiatrist who prescribes these medications and others to make sure that
patients are monitored for these complications. There is always a question of
what constitutes adequate informed consent when we are talking about a
potential complication rate of 0.03%. At that level it is certainly possible
that many psychiatrists have never seen these complications and never will. I
think it is reasonable to let people know that medications they are taking can
cause rare but potentially serious side effects including death. The informed
consent issue was not touched on in the paper but a day-to-day practice it is
an important one. From a practical standpoint I generally advise people that if they are taking a medication with rare but potentially life threatening side effects, they have to take all physical symptoms seriously. Physical symptoms cannot be attributed to common explanations like colds, the flu, or gastroenteritis.
This paper had a very specific focus and it did not touch on the other metabolic and neurological complications of these medications that require additional screening. One of the reasons I posted my ROS document on this blog was to make ti easy for any clinic or psychiatrist to build their own template with the relevant questions needed for their own patient population.
This paper had a very specific focus and it did not touch on the other metabolic and neurological complications of these medications that require additional screening. One of the reasons I posted my ROS document on this blog was to make ti easy for any clinic or psychiatrist to build their own template with the relevant questions needed for their own patient population.
George Dawson, MD, DFAPA
References:
1: Sweeney M, Whisky
E, Patel RK, Tracy DK, Shergill SS, Plymen CM.
understanding and managing cardiac side effects of second-generation
antipsychotics in the treatment of schizophrenia. Br J Psych Advances 2019:
1-15.
2: Patel RK, Moore AM, Piper S, Sweeney M,
Whiskey E, Cole G, Shergill SS, Plymen CM. Clozapine and cardiotoxicity - A
guide for psychiatrists written by cardiologists. Psychiatry Res. 2019 Jul
24:112491. doi:10.1016/j.psychres.2019.112491.
[Epub ahead of print] Review. PubMed PMID: 31351758.