Friday, December 30, 2016
Breakfast With My Old Mentor
I have some other posts ready to go, but I wanted to end the year on a positive note. I could not think of anything more positive than my old mentor being back in town and suggesting that we meet for breakfast. I would not be where I am today without mentors. Mentors who told me what to do and silent mentors who I could just identity with. Both types have been invaluable to a guy who did not have a clear idea of what he wanted to do in life. When it comes to people who carefully plan their life and people who are on kind of a random walk - I was firmly in the latter camp until some time after college.
The only reason I went to college was to play football. I got a scholarship. It did not take long to discover that was a bad idea. That discovery was facilitated by a gangrenous appendix. During the hospital stay, one of my professors came in to visit. He basically told me to snap out of it, drop the idea of coaching and a physical education minor, and do something more rigorous academically. He literally told me that I was wasting my time. He was very animated about it. When he left I wondered why an unpopular professor with a reputation for eccentricity would visit a freshman who he had only known for about a month and tell me that my life trajectory was wrong. And why would I immediately see that he was right?
It was not long before I had met chemistry and biology professors that I could identify with. I also had very positive experiences with the English and Philosophy professors. That led to increasing motivation and academic rigor. Medical school was not much different. It was natural to gravitate to neuroanatomists, biochemists, neurosurgeons, neurologists, internists, endocrinologists, nephrologists, cardiologists, and infectious disease specialists. Learning medicine and psychiatry in medical school and residency was an exciting immersive educational experience. Not all of the professors were stimulating or inspiring. I did not consider those fields for a second. After the computer match of several specialties psychiatry was the next step.
I met my mentor in my PGY2 year in 1984. He had just left private practice to do research. There was never any doubt that he was extremely knowledgeable in psychiatry. At the time there was an active debate between the so-called biological psychiatrists and the psychiatrists who were more psychotherapy oriented. The biological psychiatrists were basically phenomenologists in search of biological paradigms at the time. Some of the more prominent paradigms at the time were psychopharmacology, genetics, primate research and neuroendocrinology. In many cases, residents were split by identification with some faculty or alienation from others. My mentor was comfortable in all areas. We could discuss biological theories and then how to introduce and conduct psychodynamic psychotherapy. He explained how he did it and it made things possible. He highlighted our discussions with with examples from his own experience. He asked me questions about what it was really like to be a psychiatrist: "Suppose you are at a cocktail party and a person approaches you. That person appears to be acting out. Do you react to them like psychiatrist or not? Do you think that you can put being a psychiatrist on hold?" Questions that most PGY2s have not had time to contemplate when doing night call on psychiatric units full of transplant patients - many with difficult to control diabetes. All of this was worked in between seeing patients and doing the usual patients presentation in the clinic and the hospital.
I moved on to a different program for the last two years. The same biological psychiatry versus psychotherapists going on in the new program where interestingly there were biological researchers with strong interests in both psychodynamic and behavioral therapy. It was the only program where I have ever seen pharmacotherapy contingent on whether or not the behavior therapy was attempted or successful. Even more psychiatrists with the same orientation as my original mentor.
We ordered breakfast and settled in. It was the first time we would be talking for an hour in 32 years. I had talked with him briefly outside of a lecture that he was getting ready for at an APA meeting. He brought me up to speed on what he was doing. He got in on the ground floor of psychiatric research in a particular specialty and it was apparent that he knew most of the field cold. He e-mailed me several papers later. We discussed a few medical problems and the morbidity of the aging process. We discussed some issues that come up teaching residents and I remembered some of the things he told me about my personality and style that were dead on. We talked about my concern over the FDA contraindication for bupropion in active or resolved eating disorders and what needed to be done about that. We discussed the historical development of the DSM and its limitations. He told me something I had never heard there - organized psychology tried to come up with an alternative to the DSM-III and failed. I informed him about the Psychodynamic Diagnostic Manual (PDM) and my experience discussing it with some East Coast clinicians. We made a few jokes - technically we were peers, but he was always easy to relate to. As the hour wound down we settled on a few truths that we had come to over the years about psychiatry and I thought I would include them here as a positive jumping off point for the new year:
1. It is all about the biology -
I have always reflected on my teachers of clinical psychiatry and concluded that I was very fortunate to be taught by the best from two very different programs. That all started with my mentor. About two thirds of the way into our conversation he made this statement and I found myself in complete agreement. When I was in medical school psychiatry was in a very primitive state and a lot of that was due to the nature versus nurture argument. The psychiatric assessment and mental status exam has not changed since that time. There are generally 200 - 300 data points gathered in a standard assessment and the goal is to come up with a formulation of the problem and a separate list of diagnoses. If you are a resident of course they need to be DSM diagnoses. The problem then as now is that the explanatory power of the formulation is not necessarily robust. At the end of that presentation somebody in the crowd could always say: "So is it nature or is it nurture?" On either end of that spectrum the formulation could encompass - "Who cares if it is nature or nurture - I just prescribe medication for specific diagnoses." to "I only do psychotherapy - this is repressed narcissistic rage. I prescribe a little amitriptyline if needed for sleep." Hardly robust explanatory paradigms and the old Popperian baggage that psychoanalytic theories were not falsifiable.
The biggest missed opportunity during residency was not capitalizing on the neuroscience of the day. The academic centers where I was studying were firmly into primatology, neuroendocrinology, and psychopharmacology. Nobody seemed to pick up on Kandel's early work for about a decade. There was much debate about what biological psychiatry was and the definition I was picking up on at the time was treatment with medications. There was a focus on neurotransmitters and neural transmission. But my entire residency occurred before the advent of selective serotonin reuptake inhibitors (SSRIs) and atypical antipsychotics (AAPs). The most effective medication for the indication was lithium and that is still probably the case. Over the intervening decades neuroscience has taken off. We now have an early appreciation of the complexity of the brain and nervous system with advances every year. We are very close to the point where we are able to investigate putative neuroscience based mechanisms for stress, psychological trauma, environmentally determined epigenetic changes that cause important changes in behavior, common psychiatric syndromes, genetically determined changes in drug metabolism, and primary genetic transmission of mental disorders. There has been an explosion of information about the molecular biology of addiction and dementias. It seems that many people have discovered in the last 10 years what Kandel was writing about in 1979 - psychotherapy changes biology. How else would it work? All of this information is immediately relevant for psychiatrists.
2. The last thing that we need is another research proven psychotherapy -
I found that I had psychotherapy training in residency that was second to none. As a resident that occurred primarily as one hour of direct supervision for every hour that I was in session with a patient and that was about 450 hours per year for three years. The psychotherapy supervisors were diverse in terms of their orientation. I picked up additional training on inpatient services from psychoanalysts and others. It seemed obvious to me that you have to say something useful to people when you see them and that typically flowed from one form of therapy or the other. In psychiatry due to the severity of the problem and the general lack of medical care - flexibility was necessary. I can recall making a diagnosis of probable partial complex seizures in a patient I thought that short term psychodynamic crisis oriented therapy might be useful.
Over the years, psychotherapy research led to more manuals for standardized approaches. I remember getting an early copy of Linehan's Dialectical Behavior Therapy mailed directly to me from the inventor herself. I accumulated a library of psychotherapy texts on supportive, psychodynamic, behavioral, cognitive behavioral, and the more recent modifications. But the problem with psychotherapy was never a lack of useful models. There was fairly good evidence that psychotherapy may not be all that specific. Therapists from different schools could both get good results. There was a general lack of adequate research of psychodynamic/psychoanalytic therapy. There were also some clinical trials that may have left the wrong impression. I recall an early partially negative trial of psychotherapy in schizophrenia that seemed counter to older anecdotal literature. More recent cognitive behavioral therapy of schizophrenia and other severe mental illnesses seems to correct the idea that psychotherapy is not useful.
In our discussion of psychotherapy we both agreed that there is really no research based psychotherapy available largely due to managed care environments. I thought the average number of sessions for most managed care patients was 3. He had just read an article suggesting it was 1. Either way the practical limitations for psychiatrists in these settings is that they are scheduled for brief medication focused visits and long intervals. A person with a severe mental illness who is not in a crisis situation may be seen every 3 months for 15 - 20 minutes. But even in that rationed and sparse setting, I worked with a psychiatrist who established incredible relationships with people. I had people asking me for years after he left, if I knew what had become of him.
We both agreed that it was futile to keep doing psychotherapy research on heterogeneous populations and inventing different psychotherapies when the results are generally the same (and probably limited by varying subject characteristics) and research proven psychotherapy cannot be provided due to managed care rationing. The therapeutic alliance and useful discussions with patients need continued application. Nothing useful tends to happen unless the patient believes they are clearly understood and that is communicated by the psychiatrist.
3. Residents have to care about the DSM - we don't -
Through all of the fake news about the release of the DSM-5, I maintained that all of the hype was hardly necessary for a very imperfect classification system that is slightly important to psychiatrists - but nobody else. We agreed it was useful for residents to learn but really not that important for practicing psychiatrists. The basis of that agreement and the need for the residents to learn it is that we know all of the deficiencies and the few strong points better than anybody else. It caused me to recall the electronic medical record that I use. Each major diagnostic category has about 240 listed diagnoses or nearly the total in the DSM-5. There are so many that I can have difficulty finding the correct one. Like most psychiatrists, I am using about 1/4 of the diagnoses and recognize the limitations not only of those diagnoses - but limitations of the idea that simple verbal descriptions can parse the most complicated organ into a large number of useful diagnoses.
All in all it was a good breakfast. I was happy to see my mentor and he was happy to see me. Along the way I think I evolved into a competent clinical psychiatrist with a very similar skill set (except the extensive research). I know that the other residents in my class did the same.
I feel privileged and elevated by acquiring those skills directly from my mentors and colleagues along the way. It transformed my early random walk into academics into a focused professional life.
And I am very grateful for that.
Happy New Year!
George Dawson, MD, DFAPA
Attribution
Eggs Benedict picture at the top is By balise42 (http://www.flickr.com/photos/ipalatin/5261997126/) [CC BY-SA 2.0 (http://creativecommons.org/licenses/by-sa/2.0)], via Wikimedia Commons at https://upload.wikimedia.org/wikipedia/commons/2/2b/Eggs_benedict.jpg
Wednesday, December 28, 2016
The Moral Dilemma Of Alcohol Exposure
Before anyone schools me about Prohibition - I give lectures on Prohibition. I know it doesn't work and I know the reasons why. I also know that talking about restricting intoxicants in any way is counter to the current zeitgeist of liberalizing their availability.
I also treat alcoholics and I know how that works. When I see Minnesota's largest and most famous retailer opening up large and attractive liquor stores where there used to be not so attractive foods courts and positioning it right across from the cash registers - I know that will be a problem for a lot of people trying to stay sober. I know that for many people in recovery - an attractive liquor store in their favorite retail store or grocery store creates a very high probability of relapse - even if they know that relapse may result in death or severe disability. In Minnesota liquor stores hours is another issue. In states where liquor sales are prohibited like Minnesota, it is incentive to drive across the border into bordering states in order to buy alcohol. A modification is the availability of low alcohol content beer from grocery stores and gas stations.
Another proxy measure for relapse risk would be the total number of bars in each state. That data is harder to get. I have information from a tavern owner that the business organization representing them sets the maximum number at 1 tavern or bar per 500 people, but the actual limits are subject to local jurisdiction. In reality the maximum tavern/bar concentrations occur in North Dakota, Montana, Wisconsin, and South Dakota ranging from 1621 - 2268 people per tavern/bar. At the lower end Virginia ranks 50th at 64,773 people per tavern/bar. (US Census Bureau Data per The Forum).
Are retailers that desperate that they all need to compete in this low margin business? Why are governments in this business at all? I know that there are vocal people everywhere who argue for their unalienable right to intoxicants. One of the main arguments has always been that the vast majority of people can drink and not incur any problems from it. What about the people who cannot? Binge drinking, alcohol poisoning, and excessive alcohol use are all major public health problems according to the CDC. The direct and indirect cost of excessive drinking in the US is about $249 billion in direct and indirect costs.
One of the main arguments of cannabis advocates is how dangerous alcohol is. Alcohol costs $1.90 per drink according to the CDC in complications from drinking. That cost is probably artificially low because treatment and detoxification from alcohol is rationed and most people don't get anywhere near the level of treatment they need. In Twin Cities metro hospitals - drug and alcohol use can account for up to 60% of admissions. Potential consumer advocates in this case belong to an organization that values anonymity and as far as I know has not been very politically active.
The CDC (Community Preventive Services Task Force) suggests that alcohol excise taxes need to be increased, alcohol outlet density needs to be decreased, hours of sales need to be decreased rather than increased, and retailers need to be held liable for damages caused by underage or intoxicated drinkers. The tax suggestion reminds me of the general theory of sin taxes and why they really don't work from a governing standpoint. It basically generates money for politicians to spend and is typically diverted away from any stated use that involves treating complications of the activity.
To me the alcohol issue is much bigger than who sells it, but governments have a big problem at the moral and public health levels. Just carrying forward the CDC recommendations invites rhetorical response about prohibition or temperance. I have found myself in illogical arguments with both individuals and families about the right to drink oneself to death. Make no mistake about it, the issue was not suicide - just continuing to drink with advanced liver disease and repeated hospitalizations for bleeding problems and encephalopathy due to advancing liver disease and the associated anatomical and physiological changes.
At its base, the alcohol problems and tolerating excessive alcohol use is a cultural problem. In the Midwest where binge drinking is most prominent, teenagers start drinking in middle school. In many areas it is a rite of passage. Even though the majority of people don't drink. It is very difficult to find social settings that are alcohol free. Alcohol use in most settings is promoted as the social norm with the exception of a few subcultures. Barring a widespread cultural movement that promotes moderation or abstinence, it appears that the usual educational measures about the dangers of alcohol use will be the primary intervention point. Secondary and tertiary prevention depends on a robust system of care for alcohol use and that currently does not exist. In some cases close monitoring by the correctional system for people with DWI infractions can be effective, but that does not address either the group of people who do not come to legal attention or those for which legal intervention is not a deterrent. It also does not provide long term solutions to the problem of continued alcohol use.
Despite all of the current hype about how some intoxicants are wonder drugs and the ongoing arguments about legalization of all or most intoxicants - I can't help but see this as another moral dilemma. The will of the many basically writing off the serious problems of the few. This often plays out in families where one member clearly has a severe drinking problem and the others (usually a spouse) refuses to not drink in front of them or not have alcohol available in the home. It all comes down to the rationalization that everyone can control their drinking or that drinking can be seen as bad behavior and that is obviously not true.
The moral dilemma of increasing alcohol availability or the government sanctioned availability of any intoxicant is the same. It is based on the theory that people in general can use these intoxicants without damaging other members of society or themselves to the point that they do not become a cost to the rest of society. That essentially writes off the group of people with uncontrolled use who cannot do that. American society traditionally handles that problem by punishment and rationing availability of treatment and detox services. Functional detox services staffed by physicians are practically unheard of. Contrary to that guy in your freshman philosophy course who doubted the meaning of everything - moral philosophers can also add a perspective here. Consider this quote from Blackburn about the nature of moral knowledge:
"There are countless small unpretentious things that we know with perfect certainty. Happiness is preferable to misery, and dignity is better than humiliation. It is bad that people suffer and worse if a culture turns a blind eye to their suffering. Death is worse than life; the attempt to find a common point of view is better than a manipulative contempt for it." (1).
The availability and treatment of alcohol related problems in American society on one hand and the motivation to profit from it on the other hand seems to stand Blackburn's quote on its ear. In the US there is a clear blind eye approach to alcoholism.
It may be time to come up with a better plan for living.
George Dawson, MD, DFAPA
References:
1: Simon Blackburn. Being Good - A Short Introduction To Ethics. Oxford University Press. Oxford, UK. p. 134.
Graphic:
Liquor store density is from Health Indicators Warehouse at www.healthindicators.gov and is in the public domain. This graphic was generated on that site. (click to enlarge)
Monday, December 26, 2016
Basic Models
In order to bring some clarity into the discussion of why neuroscience is important for psychiatrists, I thought I would get back to the basics. I have three models in the above graphic that I think represent the basic conceptualizations of the brain in my lifetime. They are very basic models, but I think reasonable jumping off points for further discussion. They also serve to make my point about the importance of neuroscience. I realize that there is a natural human tendency to be argumentative. When I mention neuroscience or even science it seems that many psychiatrists and interestingly their detractors both get irritated. I can understand why the detractors are irritated since many of them are at the level of Black Box thinking in the above diagram. I will elaborate further, but many of them seem to consider the brain an amalgam of various qualities that either defy understanding or are unnecessary to understand because the brain may be involved at the very periphery of human behavior if at all. But I don't understand any attitude on the part of brain professionals like psychiatrists that doubt the importance of neuroscience. With that let me proceed with the three levels of thought about the brain in the above diagram.
The Black Box embodies what people have thought about the brain since the beginning of time. The brain is a mystery on the one hand and immutable on the other. The reality of that situation could not be denied for long. It was obvious that people with clear brain damage who survived the initial insult could have a number of changes in cognition, personality, and social behavior. The black box view eventually gave way to mind-body dualism that held there were a number of mental phenomenon that could not be explained by physical properties alone. That is really the last refuge of the Black Box and that is that the conscious human state has not been explained in terms of how it arises from the neural correlates of consciousness. It is an active area of research in the Clear Box area today. It is always interesting in terms of who adheres to Black Box thinking these days. I can't think of any legitimate science that occurs using this model. Pre-modern and modern neuroscience if anything has clearly dispelled black box and most mind-body duality. Some philosophers and antipsychiatrists are at this level.
In the Grey Box Box things got clearer. The transition from Black to Grey to Clear is not a well defined boundary. The best example that I can think of is German neuropsychiatry at the beginning of the 20th century. Much of that movement was focused in asylums. There is a famous picture of giants in the field like Kraepelin. Alzheimer, Nissl, Binswanger and others who were active at the time. These psychiatrists made good phenomenological observations but they were also focused on gross neuroanatomy. In the case of some illnesses like Alzheimer disease some observations could be made at autopsy. In the case of schizophrenia and bipolar disorder, gross anatomical changes were not evident. Although that is a negative finding. it is a finding that propelled a century of more sophisticated neuroanatomy, neurophysiology and the beginnings of a much more sophisticated molecular biological approach to functional mental illnesses or illnesses with no gross anatomical or physiological markers.
While neuroscience was moving forward at a slow pace, there was some slight progress on the fronts of diagnosis and treatment. The DSM is always a controversial document, largely because there is never any shortage of self-proclaimed experts in psychiatry. Psychiatrists know the limitations, what can be tested for, what physical illnesses are important to rule out, and what states can be cause by drug or alcohol intoxication, chronic use and withdrawal. These medical and intoxicant induced states are all clear medical illnesses by any definition as well as the associated syndromes. There is a disclaimer in the DSM about who should be using it. Training is required to conduct the appropriate evaluations and make the appropriate diagnosis. Further training is required to assure that patients can be safely treated. Associated medical conditions need to be recognized and diagnosed. All of this came about as a result of a medical focus that was reemphasized with the advent of the DSM. Prior to that there was an overemphasis on psychoanalysis and psychodynamic psychotherapy. A darker Grey Box consisted of a brain full of psychoanalytic constructs and the diagnosis and treatment was overly dependent on this model.
DSM technology was a required step in refocusing psychiatry on medicine and the brain as an organ. But that occurred 40 years ago. During that time, psychiatrists diagnoses and treat people based on clinical experience and general patterns that they recognize in the course of their training and practice. In some cases the DSM has very clear criteria that are very helpful - like the definition of a manic episode. In other cases - like the difference between anxiety and depression there are problems. The same patients can endorse predominately anxious symptoms one week and predominately depressive symptoms the next. The severity of the illness can typically lead to a clearer diagnosis and that is most likely due to the fact that the boundary between a clinical case and normal is arbitrarily defined as impairment in functioning. More impairment should lead to clearer diagnosis. Better markers to classify illness and hopefully predict treatment response are needed. The search for these markers is an active area of investigation. Psychiatry will remain in the Grey Box without these markers and more clear-cut treatments that address the underlying biological changes.
A lot of pharmacological research was done during the DSM era. There was a lot of discussion about neurotransmitter and receptor pharmacology and the implications for scientific treatment. Like all science, receptor pharmacology and post synaptic cell signalling mechanisms do not stand still. There are many theories of receptor and drug pharmacology that have stood the test of time. With a focus on the pathological nobody could hope that drugs that were often accidentally discovered would lead to highly effective treatments or a more comprehensive theory of mental illness or normal brain function. Clinical trials of psychiatric drugs and studies of pharmacology and physiology are are also limited by research subject heterogeneity. That is a problem with research on any complex polygenic illness. In the case of pure mental illness where any medical cause has been ruled out, the DSM criteria alone are a poor filter for selecting homogeneous populations for research.
Drug and psychotherapy research in the Grey Box have both suffered from treatments being applied to heterogeneous populations. There is no researcher that I know who thinks that any two people with a DSM diagnosis are similar to the point that drug or medication response would be high or necessarily reproducible. Apart from the diagnostic problem, the DSM suggests homogeneity in a context where any seasoned clinician knows differently.
The Clear Box is the goal here. The knowledge needed to get to this box is much more comprehensive. It recognizes brain complexity and the importance of the conscious state rather than just a collection of DSM descriptors. Despite the fact that many of the basic mechanisms were elucidated over 40 years ago neuroscience has detractors just like psychiatry. A common strategy of neuroscience detractors is to take either a research finding or a media quote and "debunk" it with fanfare in the popular media. Ulterior motives are often suggested for connecting neuroscience primarily with psychiatric disorders. Many of these detractors depend on their own characterization of the original research and the cultural phenomenon of piling on with negative criticism to score what appears to be a victory with the vocal and like minded. They use the same strategy in claiming that mental illness or addictions are "not diseases" like "real" diseases - despite the fact that the general population considers them to be equivalent. I find nothing compelling about critiques of ongoing science and medicine by the unqualified. The main problem is that the people truly qualified to produce the criticism are ignored in favor of what amounts to unscientific criticism. There is a secondary problem with the proliferation of journals, especially opinion pieces rather than scientific papers.
Another interesting thought that I had about the Clear Box is that many people have no difficulty at all in recognizing that machine intelligence is improving and that at some point it might exceed human intelligence. They don't seem to have any problem in figuring out whether a computer may have negotiated the Turing Test and seem indistinguishable from another human being. Many people seem to have difficulty recognizing the computational capacity of the human brain and the result of that complexity. Despite some philosophical arguments - that is a possible reason for not seeing the Clear Box as the preferred state of brain knowledge.
I have tried to point out many times that one key element of the mischaracterization of neuroscience in psychiatry is a basic lack of understanding of science. Science is a process and a dialogue. Medical science is more of a process and a dialogue than physical science - the processes involved are more complicated and the experiments involve proportionally fewer relevant variables. There are no differential equations based on a few variables that explain how the brain works. Entire blocks of research can end up partially true or a dead end. That does not mean there is some grand conspiracy - that just means it is time to move on to a new paradigm.
George Dawson, MD, DFAPA
Quotation Credit:
"The brain is the most complex object in the known universe" is a quote from Christof Koch, Chief Scientific Officer of the Allen Institute for Brain Science and well-known consciousness researcher.
Tip For The Better Graphic:
The graphic at the top is rendered with Visio. Blogger makes it blurry and ill defined. Click on it for the sharp Visio version.
Saturday, December 24, 2016
KFF / Washington Post Survey Of Opioid Users
The Kaiser Family Foundation and the Washington Post have released a survey of prescription opioid users to the general public. Reading through this survey and the accompanying explanations does not seem to match a few realities about the ongoing opioid epidemic. Some important dimensions of addictive drugs are left out. It is not clear to me who designed the survey. My only intent here is to critique it from the standpoint of an addiction psychiatrist and the current literature on what may have been more comprehensive questions. The key dimension with opioids and any other potentially addictive drug is that a drug is being prescribed and a certain part of the population will over administer as a result of their biology. The exact percentage of people with that tendency is unknown. After reading through the survey results, this survey suggests the number of people is about a 30% - but there are some red flags. Other literature suggests that the number is lower. The current opioid epidemic correlates with wider availability of these medications.
In order to understand the right questions to ask in a survey to detect problems with opioid use a brief review of the reinforcing effects of opioids are in order. On the positive reinforcing side many people feel and intense euphoria with first use. Many report increased energy and a sense of well being. In some cases people feel that they are thinking more clearly and in the extreme that their personality has been transformed. Many people report that they feel like they have been transformed into the person they thought that they could always be. All of these perceptions of the effect of opioids are highly reinforcing of future use. It also highlights the problem when opioids are given for minor injuries in that a susceptible population is being exposed to these effects. Another area of concern is post operative use. A significant number of people continue to take opioids long after surgical procedures are done and wound healing is accomplished.
Another source of positive reinforcement is what has been considered self medication. When a medication has the properties noted in the previous paragraph, it can take on magical qualities. In American culture illicit drugs and opioids in particular take on magical qualities. They are seen as the silver bullet for acute and chronic pain - when neither case is true. When that belief is widespread and the medication reinforces its own use - people begin to use it for insomnia, anxiety, depression, and as a general solution to stress. Some people will report that they just "don't want to feel anything" and will take enough of the drug to do that. Taking the medication for these secondary effects can also reinforce use and lead to escalation of the dose.
Negative reinforcement is another aspect of addictive drugs. In the case of negative reinforcement, the frequency of any behavior to decrease the response to an aversive stimulus increases. With opioids the aversive stimulus is opioid withdrawal and the early symptoms are associated with cravings to use opioids and continue the addiction. During that phase of addiction there is typically a tolerance to the euphorigenic and other positive reinforcing effects of opioids. People are using opioids at this time primarily to prevent withdrawal but now the withdrawal has a host of associated effects like insomnia. anxiety, and depression that also must be avoided.
That landscape of addiction, tolerance, withdrawal, positive reinforcement and negative reinforcement does not make this an easy problem to study. There is an even larger problem and that is that decision-making is compromised in the direction of continuing the addiction. That translates to dishonesty about use and in many cases dishonest behavior necessary to acquire and use drugs. That dishonesty in the service of addiction is a major problem in studying addiction and providing clinical services. It is the reason for toxicological testing, collateral information, and establishing sober environments with no access to intoxicants. Any survey of patients with potential addictions should address how this issue has been handled in the sample. Studies have been done on the predictive value of specific behaviors with opioids like purposeful oversedation, lost prescriptions, mixing alcohol with opioids, early prescription renewals, etc. but many of these stuides also depend on self report.
How does the KFF/Washington Post survey do? First off the random sample is a combination of people using prescription opioids (N=807) or in the household where a person uses opioids (N=187). The indication for opioid use is chronic noncancer pain. The threshold was using for two months in the past 2 years. Only 55% of the respondents were currently taking opioids. The study was all done by telephone interview. The respondents ranked prescription painkiller abuse as a serious problem (84%) and only slightly less serious than obesity, cancer, heart disease, alcohol abuse or heroin abuse (89-95%). The lowest ranking of seriousness in that category was heroin abuse at 89%. 25% of the respondents began taking opioids for postoperative pain and 44% for chronic pain.
The section on motivation for using opioids indicated that pain relief was the major reason people were taking opioids and 92% or people ranked pain relief as either "very well or somewhat well". Secondary reasons included dealing with stress, to get high, or to relieve tension (12-34%). Of the secondary reasons getting high has the highest ranking of 34%. There are several chronic pain studies that suggest that for chronic neuropathic pain - the relief from opioids is on par with pain relief from non-opioid medications for the same application.
Physicians did not get rated very highly in the survey with only 2/3 of them warning patients about the addictive potential of opioids or talking about non-opioid strategies for treating pain. Only 1/3 of physicians had a plan to get people off opioids. Physicians did better in terms of warning patients not to use alcohol concurrently with opioids and discussing side effects but only slightly better in terms of advising patients on keeping opioids out of the hands of others.
In medical practice, especially with electronic health record systems there is often an emphasis on pre-existing alcohol or substance use disorders. The closest this survey comes is to ask about the number of alcohol drinks per week. About 22% of respondents had more than one drink per day. There is a lot of room on the high side. There is also a dissociation between known addictive disorders and opioid prescriptions. Many physicians believe that people with a known addictive disorder to a non-opioid including alcohol can control their use of opioids for pain. They are often reassured by these patients who tell them that they have never had a problem with opioids.
Only 18% of respondents had difficulty getting their prescriptions refilled. That contrasts with the 1/3 of patients taking the medication to get high.
The degree of polypharmacy in the sample was striking with 32% taking 7 or more prescription drugs and 25% taking 4-6 prescription drugs. Slightly over half of the sample were taking medications for insomnia, depression or anxiety. Benzodiazepines and z-drugs were not specified. The survey did ask about alcohol use while taking opioids and it is a clear problem. In addition practice it is common to see patients who are using benzodiazepines and z-drugs with opioids. It is also common to see people taking one, both and both in combination with alcohol. In addiction practice it is important to determine if anxiety, depression, and insomnia are primary, caused by the addiction, or associated with chronic intoxication or withdrawal states.
On the specific question of risk of addiction 2/3 of respondents said that "The benefits of pain relief outweigh the risk of addiction." One third of the sample said they were dependent on the drugs and would find them hard to stop. When that question was rephrased with the description "addicted" 23% thought they were addicted to the painkillers. Of the respondents who thought they were dependent or addicted - 1/3 sought treatment and 2/3 did not. An interesting study might look at videotapes of the informed consent procedure and what information the patient recalls after that procedure. My experience suggests that a large percentage of people who are actively using opioids and alcohol do not recall what was said in the initial consultation by comparison with the documentation.
The survey attempts to parse blame for the prescription painkiller epidemic and in that series of questions the groups ranging from most to least blame (61% to 15%) were ranked the patients themselves > doctors > drug companies > government > hospitals > law enforcement > pharmacies and pharmacists. The key elements here are wider access to opioid medications as a result of an initiative to treat chronic pain and a movement away from gatekeepers.
Given the limitations of a survey, I thought that the self assessment of the number of people who though they were dependent or addicted to painkillers was striking. The number of people seeking treatment though low is much higher than what has been estimated using other methodologies like the NSDUH survey. It may suggest that survey technologies alone or in combination with other corroborative methods may be useful in further studies of this phenomenon. One of the real questions out there is the number of people in the wild who are at high risk for the initial highly reinforcing properties of opioids. If I had to guess, I would put that number at about 40% of the population. There is a significant and slightly smaller group who get immediate negative effects and do not tolerate opioids at all. By definition, there may be a safe third portion of the population who can benefit from opioids with very low addiction risk. Clearly defining that population, hopefully with biological markers would have a significant impact on the problem of addiction to opioids. It would also have implications for a more elaborate diagram of the neurobiology of opioid addiction.
For physicians the problem is as clear as ever. The vast majority of this sample (95%) got prescription pain relievers to alleviate their acute or chronic pain and 1/3 end up using the drug for other reasons including getting high. That is due to the inherent properties of addictive compounds. The practical problem is how to address that risk in medical practice.
George Dawson, MD, DFAPA
References:
1: Drew Altman. Understanding Who Opioid Users Are Underscores Challenges. December 19, 2016. KFF.org
2: The Washington Post/Kaiser Survey: 1 in 3 Long-Term Prescription Painkiller Users Think They’re Addicted or Dependent. KFF.org
Saturday, December 17, 2016
Thinking and Shoveling the Snow
I got a late start today. It was 1:30 in the afternoon but the sun was already low in the sky. That violates one of the cardinal rules of snow shoveling. If you are shoveling light snow and can get most of it up off the concrete - the sun will do the rest of the work and melt it off. If it is too cold to melt on a dark surface sublimation can occur and it will transition directly from a solid to a vapor. At this temperature and sun angle - I would be lucky to get 2 hours of melting.
One of the other cardinal rules of snow shoveling is that timing is everything. I was up briefly at 7AM today. It was still dark out, but there was plenty of activity in the neighborhood. People shoveling, snowblowing, and plowing. It was still snowing lightly at the time. If you clear off the snow too early, there will be another inch or two of snow on top of your concrete. If that happens consistently you might not see concrete again until the spring thaw. I looked around and that had happened to several neighbors. I also noticed that one of my neighbors had cleared off about 90% of the heavy snow from my driveway with his snowplow. I am very appreciative of that. At a psychological level it is a mixed blessing. In my 20s, 30s, 40s, and even 50s I was a snow shoveling machine. I would attack any depth or distance of snow with a thin steel scoop shovel and dispatch it as fast as I could. Now I am becoming the old guy down the street who might be overdoing it. Maybe they are right - decreasing snow shoveling vigor may be just another sign of heading toward decrepitude.
I have the inevitable associations to learning how to shovel snow from my father. The theory of extending the shoveled surface out onto the grass for an inch or two so that any run off does not pool on the concrete and freeze. Today for the first time, I realized why we used steel scoop shovels with short handles. These were the shovels my old man used to shovel coal into a steam engine locomotive boiler when he started out as a fireman on the railroad. He let me watch him once in a switchyard near our house. I was only 5 or 6 at the time, but he was shoveling coal the size of softballs into that boiler. You could only do that job with a light steel short handled shovel. I have the usual associations about knowing my father for only 16 years or less than half the time I knew my father-in-law. Today I had the thought that all of my interactions with and reactions to my father were the product of a brain that was 10-15 years away from neuroanatomical maturity. What would it have been to know him as a mature adult? How has that affected me? If I had a son myself - what would I try to pass on to him about snow shoveling? At this point - not having a son I will never know. The snow shoveling knowledge of the Dawson clan dies with me. Even the most liberal college will probably not have a "Snow Shoveling 101" for the curious.
I drag out the snowblower and fire it up. There is still an uneven 3 - 8 inches of snow to clear up. The snowblower is about 20 years old. It was a birthday present to my wife. Believe it or not she requested it - but she might have not disclosed her real motive for that. She was probably concerned about me throwing snow around with that scoop shovel like a blender and thought: "OK - how long can he keep doing that before something bad happens?" She tells me to use the electric starter so it doesn't freeze up and I oblige. I start snowblowing in an arc over 90 degrees back and forth blowing all of the snow to the eastern side of my driveway. I realize that my driveway alone has more area than all of the concrete that my father and I used to shovel at the family home. I wish that I knew more about graph theory. The pattern that I use to shovel the driveway could probably be optimized by graph theory.
After that I get out a shovel. It is no longer a scoop shovel. It is an all plastic shovel with a 90 degree bend in the middle. They sell a lot of these shovels these days. I am very skeptical of the mechanical advantage, but it does allow a more erect posture in the process. I am using it because I have to shovel on a textured concrete sidewalk and can't use steel shovel or a snowblower without scratching the surface. I shovel a scoop wide margin up the right hand side of my walkway and then come back cross cutting the width of the side walk. Swing the shovel from left to right and throwing the snow off the end - the same way my father used to shovel coal. It takes 30 swipes and I am clear. I check my heart rate and it hasn't budged. The last time I shoveled a week ago it was up about 20%. As I was shoveling I thought of an exercise device that would mimic snow shoveling. In many ways it is a whole body work out. Kind of like a kettle bell at the end of a longer handle.
I also fantasize about high tech approaches. For some reason I have become more and more fascinated with tractors. I was watching the Discovery Channel late one night and saw a small Swedish tractor that was designed to clear airport runways. They were using it to build an ice castle. It was designed to eject large amounts of snow directly over the front of the drivers cab. I think about what a great time it would be to drive this tractor all day long - moving tons and tons of snow. I conclude it is a narcissistic snow shoveling fantasy - a probable reaction to my concerns about becoming a less competent snow shoveler. Still it would be nice to drive that tractor even for a day or two...
I come back to the main driveway and decide that I need to go over it with a shovel it see if I can expose more of the concrete surface to the sun. This time I create several shovel widths down the west side and cross cut from west to east about 60 times. I look at my activity monitor and notice that it has only taken about 3000 steps to do the entire job. I have the thought that with the exception of some time I spent in East Africa, I have been shoveling snow for 50 years. I also recall that in the famous Halloween blizzard/storm of the century my father-in-law and brother-in-law shoveled a foot of snow away from my old Chevy Chevette, crawled under it, and dropped in a new starter motor. It was parked on the street at the time, it was nighttime, and it was 5 below. They had to run a hundred yards of extension cord out to the street to do the work.
You might say that I am emotionally connected to the snow and shoveling it. There is a lot of meaning there and in my 50th years of shoveling it - that meaning is not diminished. It might explain why I have no interest in moving to warmer climates. Thinking a lot about things has always worked for me. Shoveling snow is time to think and reflect.
I occasionally think of the limitations to all of this thinking.
Driving motorcycles is just one example. I stay off of them.
George Dawson, MD, DFAPA
Friday, December 16, 2016
Alcohol Overuse After Gastric Bypass Surgery
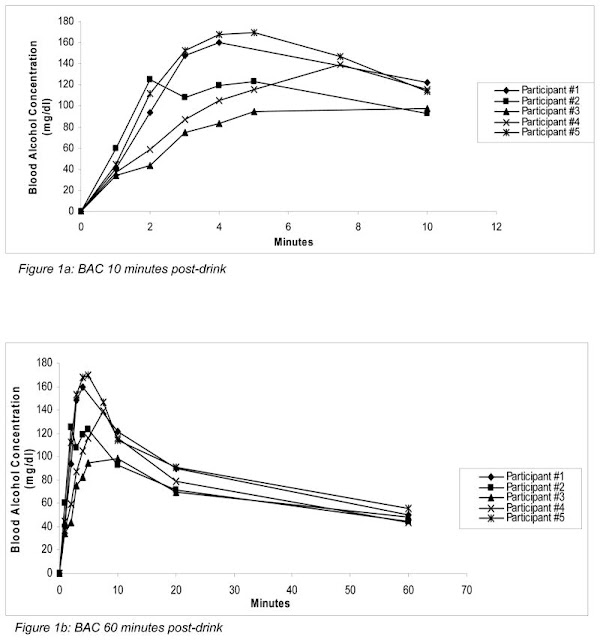
Alcohol use disorders after gastric bypass procedures are a significant complication of this surgery. I typically see people who have developed the disorder after the gastric bypass procedure. The majority of those procedures these days are Roux-en-Y (RYGB). The surgical mechanics of RYGB are widely available and I am not going to review them here. This post is about how the procedure can change a person into a problem drinker endangering both their health and in some cases leading to substantial weight gain after initial losses from the bypass procedure. Although there are other surgical techniques used for gastric bypass that also lead to this complication RYGB is the most common technique and is more likely to be studied. In the figures above, blood alcohol levels are determined in individuals who had undergone RYGB surgery after ingestion of alcohol.
One of the well known principles in addiction medicine is that overuse of any potentially addictive substance generally follows pharmacological principles especially as tolerance to a drug develops. Other factors such as economics, whether a drug can be used by a particular route, and biologically determined sensitivities to drugs can modify that basic concept. To illustrate, most current opioid users with addiction problems started by using prescription painkillers. They may have modified the original prescription pills by crushing them and either smoking or snorting them. In some cases, they crush the pills, dissolve them, crudely filter them and inject them. In this case they are trying to optimize the time to peak drug concentration Tmax and maximum drug concentration Cmax for maximum effect. In the case of alcohol, it is generally too dangerous to use by the inhaled or intravenous route. The effects are limited by absorption and elimination by zero order kinetics.
The graphics at the top of this page are from reference 1. It shows the results of blood alcohol concentration of 5 RYGB patients after drinking a solution of 40% vodka and orange juice calculated to contain 0.3 gram per kilogram body weight. The vodka and orange juice mixture was adjusted to contain a 50:50 mix of vodka:orange juice. Mean dose of ethanol given was 26.9 ± 2.3 grams or about 2 standard drinks consumed over a period of 5 minutes. On the graphs alcohol concentration is given as mg/dl. In the US, the current legal driving limit is 80 mg/dl or 0.08%. The researchers decided to look at the time from 0-10 minutes apart from 0-60 minutes because previous work started the measurements at 10 minutes. The other point to notice in these graphs is that there is no control group. That is unfortunate given the variable methods (alcohol dose and consumption time) that are used to determine the pharmacokinetics of alcohol in research papers that look at this question.
A comparison with control subjects in the literature can be done, but I could not find any studies that used a dose of 0.3 g/kg of ethanol. Many studies used a dose of 0.6 g/kg. The study used in the comparison below used a dose of 0.8 g/kg ingested over 30 minutes. Comparing Tmax and Cmax for the study on RYGB patients to a study of 12 healthy male controls shows the following differences:
Experimental differences aside. the Cmax and Tmax for alcohol in the RYGB patients are markedly different. The time to peak alcohol levels was only 5.4 minutes in the RYGB group and at that time the average Cmax easily exceeded the legal driving limit on what amounts to 2 standard drinks. Although the study did not correlate the rapid peak of alcohol with effects, they are readily observed by any clinician interested in how intoxicants affect the conscious state of the patient. People typically tell me that they feel immediate intoxication or in some cases blackout. The intoxication is a rapid sense of euphoria combined with an immediate cessation of negative mood states. In the case of blacking out, this is a frequent end point with severe alcohol addiction. Many people are self professed "black out drunks" and that is their preferred endpoint of acute intoxication and the goal of subsequent drinking sessions. These states are highly reinforcing for susceptible people and probably explain the greater than expected occurrence of alcohol related disorders following RYGB surgery. Looking at the prevalence of alcohol use disorder (AUD) before and after RYGB surgery, Mitchell, et al found that 8% had AUD within the 3 year post op period including 48% who had no prior history of AUD. Including a more permissive screening tool the number increased to 18.4% and 40.6% respectively. A previous study showed that the prevalence of AUD symptoms was greater in year 2 post gastric bypass surgery (9.6%) and was associated with a number of preoperative variables including RYGB, male sex, smoking, and regular alcohol consumption before the procedure.
The studies that look at the prevalence of alcohol use are interesting. From the perspective of an addiction psychiatrist who only sees patients selected for addiction, observing the effect of scale is significant. As an example, the patients who I see with this problem are predominantly women and practically all of them did not have an alcohol use problem prior to surgery. In many cases they did not drink alcohol. Practically all had undergone RYGB but there were also people with other bypass procedures.
An additional research question has been whether the anatomic changes in RYGB lead to changes in the brain and central nervous system that changes addictive behavior. The model used for these investigations have been obese rats that have undergone RYGB and intravenous self administration of alcohol and drugs. That model would eliminate pharmacokinetic considerations from oral administration with rapid increases in plasma concentration in a short while. Rats with RYGB self administer intravenous alcohol and opioids at a higher rat than rats that have not had gastric bypass surgery suggesting a centrally mediated mechanism more independent of gut absorption (5,6). One set of authors (5) proposed that in obesity there is blunted dopamine and ghrelin signalling. They make the case that leptin and ghrelin both affect dopaminergic signalling in the reward system. (see diagram - click to enlarge).
Despite being well known to eating disorder and addiction specialists, I don't think the phenomenon of alcohol overuse in gastric bypass patients is well known. It has implications for informed consent for this surgical procedure, some risk factor modification, and follow up. It also may have implications for the diagnosis and treatment of alcohol use disorders. As an example, binge drinkers and blackout drinkers are a known subset the population of people with alcohol use disorders. Does this group have any similarities with the population of RYGB patients who develop alcohol use disorders? What would pharmacokinetic studies of alcohol in this group show? If a profile of peptide hormone changes in the RYGB group is defined - should that be studied in binge and blackout drinkers as well?
These might lead to useful endophenotypes for alcohol use disorder that could lead to treatment interventions.
George Dawson, MD, DFAPA
References:
1: Steffen KJ, Engel SG, Pollert GA, Li C, Mitchell JE. Blood alcohol concentrations rise rapidly and dramatically after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2013 May-Jun;9(3):470-3. doi: 10.1016/j.soard.2013.02.002. PubMed PMID: 23507629; PubMed Central PMCID: PMC4487806.
2: Jones AW, Jönsson KÅ. Between subject and within subject variation in the pharmacokinetics of ethanol. Br J Clin Pharmac 1994; 37: 427-431.
3: Mitchell JE, Steffen K, Engel S, King WC, Chen JY, Winters K, Sogg S, Sondag C, Kalarchian M, Elder K. Addictive disorders after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2015 Jul-Aug;11(4):897-905. doi: 10.1016/j.soard.2014.10.026. PubMed PMID: 25862182; PubMed Central PMCID: PMC4430439.
4: King WC, Chen JY, Mitchell JE, Kalarchian MA, Steffen KJ, Engel SG, Courcoulas AP, Pories WJ, Yanovski SZ. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012 Jun 20;307(23):2516-25. doi: 10.1001/jama.2012.6147. PubMed PMID: 22710289; PubMed Central PMCID: PMC3682834.
5: Polston JE, Pritchett CE, Tomasko JM, Rogers AM, Leggio L, Thanos PK, Volkow ND, Hajnal A. Roux-en-Y gastric bypass increases intravenous ethanol self-administration in dietary obese rats. PLoS One. 2013 Dec 31;8(12):e83741. doi: 10.1371/journal.pone.0083741. PubMed PMID: 24391816; PubMed Central PMCID: PMC3877092.
6: Biegler JM, Freet CS, Horvath N, Rogers AM, Hajnal A. Increased intravenous morphine self-administration following Roux-en-Y gastric bypass in dietary obese rats. Brain Res Bull. 2016 May;123:47-52. doi: 10.1016/j.brainresbull.2015.08.003. PubMed PMID: 26304761; PubMed Central PMCID: PMC4761525.
Attributions:
Male controls (n=12)
|
RYGB patients (N=5)
|
|
Cmax (mg/dl)
|
106
|
138.4
|
Tmax (min)
|
60
|
5.4
|
Despite being well known to eating disorder and addiction specialists, I don't think the phenomenon of alcohol overuse in gastric bypass patients is well known. It has implications for informed consent for this surgical procedure, some risk factor modification, and follow up. It also may have implications for the diagnosis and treatment of alcohol use disorders. As an example, binge drinkers and blackout drinkers are a known subset the population of people with alcohol use disorders. Does this group have any similarities with the population of RYGB patients who develop alcohol use disorders? What would pharmacokinetic studies of alcohol in this group show? If a profile of peptide hormone changes in the RYGB group is defined - should that be studied in binge and blackout drinkers as well?
These might lead to useful endophenotypes for alcohol use disorder that could lead to treatment interventions.
George Dawson, MD, DFAPA
References:
1: Steffen KJ, Engel SG, Pollert GA, Li C, Mitchell JE. Blood alcohol concentrations rise rapidly and dramatically after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2013 May-Jun;9(3):470-3. doi: 10.1016/j.soard.2013.02.002. PubMed PMID: 23507629; PubMed Central PMCID: PMC4487806.
2: Jones AW, Jönsson KÅ. Between subject and within subject variation in the pharmacokinetics of ethanol. Br J Clin Pharmac 1994; 37: 427-431.
3: Mitchell JE, Steffen K, Engel S, King WC, Chen JY, Winters K, Sogg S, Sondag C, Kalarchian M, Elder K. Addictive disorders after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2015 Jul-Aug;11(4):897-905. doi: 10.1016/j.soard.2014.10.026. PubMed PMID: 25862182; PubMed Central PMCID: PMC4430439.
4: King WC, Chen JY, Mitchell JE, Kalarchian MA, Steffen KJ, Engel SG, Courcoulas AP, Pories WJ, Yanovski SZ. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012 Jun 20;307(23):2516-25. doi: 10.1001/jama.2012.6147. PubMed PMID: 22710289; PubMed Central PMCID: PMC3682834.
5: Polston JE, Pritchett CE, Tomasko JM, Rogers AM, Leggio L, Thanos PK, Volkow ND, Hajnal A. Roux-en-Y gastric bypass increases intravenous ethanol self-administration in dietary obese rats. PLoS One. 2013 Dec 31;8(12):e83741. doi: 10.1371/journal.pone.0083741. PubMed PMID: 24391816; PubMed Central PMCID: PMC3877092.
6: Biegler JM, Freet CS, Horvath N, Rogers AM, Hajnal A. Increased intravenous morphine self-administration following Roux-en-Y gastric bypass in dietary obese rats. Brain Res Bull. 2016 May;123:47-52. doi: 10.1016/j.brainresbull.2015.08.003. PubMed PMID: 26304761; PubMed Central PMCID: PMC4761525.
Attributions:
1. Figure at the top of this post is used with permission from copyright holder Copyright © 2013 American Society for Metabolic and Bariatric Surgery. Published by Elsevier Inc. All rights reserved through license 4007221260909 via the Copyright Clearance Center.
2. Figure at the bottom is from VisiScience and is used per their licensing agreement.
2. Figure at the bottom is from VisiScience and is used per their licensing agreement.
Sunday, December 11, 2016
Brandolini’s Law
There was an informative editorial in Nature this week by Phil Williamson - a scientific expert on ocean acidification. I like the concept of bullshit and have referred to Professor Harry Frankfurt's classic essay on it many times. I was not familiar with Brandolini's Law until I read the essay. Simply stated:
Brandolini’s Law: “The amount of energy needed to refute bullshit is an order of magnitude bigger than to produce it.”
It is also more simply known as the The Bullshit Asymmetry Principle.
Williamson uses a political example from a libertarian web site. The central piece of that article was that ocean pH was not decreasing and that climate change would lead to reduced carbon dioxide in the oceans. Because the climate is not changing there is no worry that the ocean pH would change. The original publication denied Williamson's rebuttal. An opinion piece in a professional journal led the author of libertarian piece to write online that his work should be "squashed like a slug". Nothing like elite scientific dialogue is there?
In the UK there is apparently a press watchdog called UK Independent Press Standards Organization (IPSO). Williamson filed a complaint with them about the factual accuracy of the piece and is awaiting their verdict. He goes on to illustrate how Brandolini's Law comes in to play in this situation. The original author these days can essentially be anyone from a journalist to a blogger. He points out that online journalism "seems to be subject to few if any rules." That leaves anyone in the position of responding to a factually inaccurate claim at a distinct disadvantage. There may not be any formal complaint procedure and there is probably no editorial hierarchy. Many web sites count on bloggers and writers to produce content that they can attach advertising to and this content seem to have very little oversight in terms of accuracy. Much of this content on social web sites makes up what has been referred to as fake news.
Williamson's position is very clear. He thinks that these inaccuracies need to be responded to and corrected. He accurately points out that the audience for the correction is not the authors, but readers who are interested in accuracy and science. I don't think that the division is that clear for a number of reasons. A large number of people really don't care. They are involved in the emotion generated by the issue and don't make decisions based on facts. That general attitude is promulgated by the political process in most countries. This is rarely a rational discussion of the main issues of the day. I think this goes a lot deeper than generating rebuttals. There needs to be education on the difference between science and everything else. A good example is Creationist based rhetoric and the denial of evolution. Creationist advocates do not seem to recognize that they are engaged in a process that is nothing like science and therefore cannot scientifically prove anything. They fail to recognize the basic issue that science is a process and not an immutable collection of writings written by ancient prophets and subject to many interpretations. That failure of recognition also leads to a failure to recognize that they are completely outside the field of science. They fail to recognize where they are and that the best critics of a scientific theory are the scientists in the field.
This failure of recognition is much wider than Creationists. Journalists produce many examples, not the least of which is a consistent bias against psychiatry. That bias is present whether or not there is editorial oversight. A great example is the journalistic tendency to propose what psychiatry is and then proceed to attack that straw man. And interestingly these outsiders with no training in medicine or psychiatry are often joined by insiders pushing the same arguments. In one case a prominent journal editor came out and endorsed an anti-psychiatry book, proclaiming legitimate criticism when in fact the book was rhetorical. I would not presume that medical editors are without common biases. There are many forces producing misinformation.
I diverge a bit with Williamson's approach on refuting the misinformation and hoping for the best. I think that there are additional considerations. One thing is very clear - the head-in-the-sand approach taken by physician professional organizations in response to misinformation is clearly not a good idea and is sure to lose in the current propaganda war of misinformation and political corruption. If there is a lesson with the current Presidential campaign it is that there is a very small margin between a typical fact less campaign and one where anything at all can be said whether it is true of not - and nobody seems to care about it.
That is foreboding for all levels of public policy, especially when the political spoils includes being able to appoint agency heads with not only a lack of basic footing in science but also a lack of knowledge about what constitutes science. For the country to run and maintain some standards in science, technology, and engineering there needs to be a basic understanding of these fields in all branches of government and at the highest levels. There is currently no better example of what happens when the unscientific manage the store than what has happened to American medicine. We are not only cursed by work rules that are made up as we go and have little to do with the practice of medicine, but we we have to live with pseudo-scientific management practices that affect our work flow and and detract from the lifelong task of learning the science of medicine. A few strategies I can offer as a blogger follow. I also have additional strategies that I am going to keep to myself until just the right time.
1. Don't feel compelled to engage - Twitter is an excellent example of how this principle is applied. Suddenly you are being given the third degree by some poster. That turns into misinterpretations of your statements and positions and before you know it personal attacks. But it doesn't stop there. A new account pops up and mysteriously continues the attack. Call them trolls or whatever you like but recognize the tactic. They don't really care what you have to say and are quite happy to waste your time. Don't engage. Twitter gives you the option to block them and that works the best.
2. Present the facts but counter the rhetoric - It is important to recognize the common forms of rhetoric without being pedantic. The best way to do that is by pointing out the erroneous aspects of the argument and the overall form without naming the fallacy. This sounds easy and it should be - but physicians and psychiatrists seem to be spellbound at times by the simplest arguments. One common example is anytime a business executive shows up and talks about "cost effectiveness" - everybody shuts down. Nobody seems to understand that this is just business rhetoric. It should be as obvious as the fact that with 30 years of intensive management and "cost effectiveness" - per capita health care costs are 40% higher than the country with the next highest per capita expenditures and health care is certainly no better. In the case of treating mental illnesses and substance use disorders it is much worse. Somebody needs to stand up and say: "We are doing our part - when are you going to start to do yours." or "Get out of the way and let us do our work." or "Give us the resources to provide the adequate service or shut it down." Rationing is clearly a very ineffective and costly way to provide health care services.
3. Recognize bullshit no matter where it comes from - Many of the arguments for health care reform are just plain erroneous. And why wouldn't they be. We now have a continuous supply of what are essentially blogposts on the front of our most respected medical journals. How could anyone expect that 12 or 52 health care reform ideas each year for years would be worth anything? All of the top posts that they have been implemented like the electronic health record, managed care as business intermediaries for government purchasers, pharmaceutical benefit managers, creating various financial incentives - have all been progressively worse ideas. Sifting through the misinformation to correct what is false, what are lies, and what is bullshit is a tedious but necessary task. As long as medical journals legitimize this constant stream of unscientific information - countering it will remain an onerous task. The sources of bullshit go far beyond blogs and traditional journalism.
4. Don't let anyone define you - A common strategy these days is that detractors tend to jump in and set the stage with false criticism. It was easy to see this in political debates. In medicine and psychiatry the same process happens and I have pointed out the dynamic on this blog. I also posted a recent summary of how the release of the DSM-5 was a major source of misinformation, lies, and bullshit in 2015 but there are many more examples in psychiatry.
5. Don't let the barbarians at the gate get you down - I tell aspiring physicians and aspiring psychiatrists the same thing - don't let the detractors or in these days trolls - get you down. Psychiatry is a tough field because there will always be a lot of people blaming you for their problems. This is where Brandolini's Law really applies. There are numerous dialogues on web sites available where the game is to post as much misinformation, bullshit and lies about psychiatry in particular. Entire web sites exist for that purpose. Entering into that discussion and taking the opposite side of the argument can be more futile than the Law suggests. It may take several orders of magnitude of effort and even then it may be futile. The best approach is to just get the information out there in cyberspace in an independent forum where you know that it can be safely viewed. That is one of the reasons that this blog exists.
6. The Internet is still the Wild West and that will probably never change in its current form - Williamson suggests that it may be possible to "harness the collective power of the Internet to improve its quality." He suggests the global scientific community reviewing sites and rating them like film rating sites. I am far less optimistic. The first problem is the scope of that project. The second would be consistency in ratings. The third is that a rating in some sense is legitimizing. It is a far better approach to ignore the ignorant. The reality is that reputation protection web sites basically work by generating a lot of information designed to bury the obnoxious web site. Most people find that if they contact a search engine about a web site that may be slandering them that they are met with a a relatively hostile response and a complete lack of interest in correcting anything. That is true for even the largest search engines. Google for example, clearly doesn't give a damn about your reputation.
7. Brandolini's Law is a significant deterrent to keeping professionals engaged in educating the public - Physicians certainly find this out in a hurry if they decide to post a rebuttal in political or media forums that are populated by the ignorant, trolls, or those with a specific agenda. That is more true of psychiatrists than any other specialty. That has a dual effect of limiting feedback to those who might be interested and eliminating the most informed criticism. It also has the added effect of adding professionals who may have legitimate criticism to antipsychiatry web sites where scientific criticism is clearly not the agenda. It is a dangerous path of least resistance when legitimate professionals start posting on web sites dedicated to the destruction of the profession.
These are just a few ideas about Brandolini's Law. I did not write the most important one down and that is you can always just go off the grid. Even then there are problems. I talked with a psychiatrist about 10 years ago who was asked to give presentations at local churches on depression. He eventually gave up because there were people in the audience who for various reasons were so disruptive that it prevented him from giving the interested people the information that they wanted. Only psychiatrists could end up being heckled in church. Bullshit can be presented in person just as easily as is can by typed online.
Williamson refers to a "rising tide of populism threatens the future of evidence-based government." I don't think that we have ever had evidence based government in the US. I see it as mostly a power dynamic here - influencing people by emotional ideas and shouting them down.
The only reason why that Brandolini's Law doesn't work in reality in the case of psychiatry is that at the end of the day, there are still people with severe mental illness - no matter who tries to deny it and a group of people called psychiatrists who are interested in helping them. That is not necessarily enough to prevent the widespread demoralization of a profession.
George Dawson, MD, DFAPA
In the UK there is apparently a press watchdog called UK Independent Press Standards Organization (IPSO). Williamson filed a complaint with them about the factual accuracy of the piece and is awaiting their verdict. He goes on to illustrate how Brandolini's Law comes in to play in this situation. The original author these days can essentially be anyone from a journalist to a blogger. He points out that online journalism "seems to be subject to few if any rules." That leaves anyone in the position of responding to a factually inaccurate claim at a distinct disadvantage. There may not be any formal complaint procedure and there is probably no editorial hierarchy. Many web sites count on bloggers and writers to produce content that they can attach advertising to and this content seem to have very little oversight in terms of accuracy. Much of this content on social web sites makes up what has been referred to as fake news.
Williamson's position is very clear. He thinks that these inaccuracies need to be responded to and corrected. He accurately points out that the audience for the correction is not the authors, but readers who are interested in accuracy and science. I don't think that the division is that clear for a number of reasons. A large number of people really don't care. They are involved in the emotion generated by the issue and don't make decisions based on facts. That general attitude is promulgated by the political process in most countries. This is rarely a rational discussion of the main issues of the day. I think this goes a lot deeper than generating rebuttals. There needs to be education on the difference between science and everything else. A good example is Creationist based rhetoric and the denial of evolution. Creationist advocates do not seem to recognize that they are engaged in a process that is nothing like science and therefore cannot scientifically prove anything. They fail to recognize the basic issue that science is a process and not an immutable collection of writings written by ancient prophets and subject to many interpretations. That failure of recognition also leads to a failure to recognize that they are completely outside the field of science. They fail to recognize where they are and that the best critics of a scientific theory are the scientists in the field.
This failure of recognition is much wider than Creationists. Journalists produce many examples, not the least of which is a consistent bias against psychiatry. That bias is present whether or not there is editorial oversight. A great example is the journalistic tendency to propose what psychiatry is and then proceed to attack that straw man. And interestingly these outsiders with no training in medicine or psychiatry are often joined by insiders pushing the same arguments. In one case a prominent journal editor came out and endorsed an anti-psychiatry book, proclaiming legitimate criticism when in fact the book was rhetorical. I would not presume that medical editors are without common biases. There are many forces producing misinformation.
I diverge a bit with Williamson's approach on refuting the misinformation and hoping for the best. I think that there are additional considerations. One thing is very clear - the head-in-the-sand approach taken by physician professional organizations in response to misinformation is clearly not a good idea and is sure to lose in the current propaganda war of misinformation and political corruption. If there is a lesson with the current Presidential campaign it is that there is a very small margin between a typical fact less campaign and one where anything at all can be said whether it is true of not - and nobody seems to care about it.
That is foreboding for all levels of public policy, especially when the political spoils includes being able to appoint agency heads with not only a lack of basic footing in science but also a lack of knowledge about what constitutes science. For the country to run and maintain some standards in science, technology, and engineering there needs to be a basic understanding of these fields in all branches of government and at the highest levels. There is currently no better example of what happens when the unscientific manage the store than what has happened to American medicine. We are not only cursed by work rules that are made up as we go and have little to do with the practice of medicine, but we we have to live with pseudo-scientific management practices that affect our work flow and and detract from the lifelong task of learning the science of medicine. A few strategies I can offer as a blogger follow. I also have additional strategies that I am going to keep to myself until just the right time.
1. Don't feel compelled to engage - Twitter is an excellent example of how this principle is applied. Suddenly you are being given the third degree by some poster. That turns into misinterpretations of your statements and positions and before you know it personal attacks. But it doesn't stop there. A new account pops up and mysteriously continues the attack. Call them trolls or whatever you like but recognize the tactic. They don't really care what you have to say and are quite happy to waste your time. Don't engage. Twitter gives you the option to block them and that works the best.
2. Present the facts but counter the rhetoric - It is important to recognize the common forms of rhetoric without being pedantic. The best way to do that is by pointing out the erroneous aspects of the argument and the overall form without naming the fallacy. This sounds easy and it should be - but physicians and psychiatrists seem to be spellbound at times by the simplest arguments. One common example is anytime a business executive shows up and talks about "cost effectiveness" - everybody shuts down. Nobody seems to understand that this is just business rhetoric. It should be as obvious as the fact that with 30 years of intensive management and "cost effectiveness" - per capita health care costs are 40% higher than the country with the next highest per capita expenditures and health care is certainly no better. In the case of treating mental illnesses and substance use disorders it is much worse. Somebody needs to stand up and say: "We are doing our part - when are you going to start to do yours." or "Get out of the way and let us do our work." or "Give us the resources to provide the adequate service or shut it down." Rationing is clearly a very ineffective and costly way to provide health care services.
3. Recognize bullshit no matter where it comes from - Many of the arguments for health care reform are just plain erroneous. And why wouldn't they be. We now have a continuous supply of what are essentially blogposts on the front of our most respected medical journals. How could anyone expect that 12 or 52 health care reform ideas each year for years would be worth anything? All of the top posts that they have been implemented like the electronic health record, managed care as business intermediaries for government purchasers, pharmaceutical benefit managers, creating various financial incentives - have all been progressively worse ideas. Sifting through the misinformation to correct what is false, what are lies, and what is bullshit is a tedious but necessary task. As long as medical journals legitimize this constant stream of unscientific information - countering it will remain an onerous task. The sources of bullshit go far beyond blogs and traditional journalism.
4. Don't let anyone define you - A common strategy these days is that detractors tend to jump in and set the stage with false criticism. It was easy to see this in political debates. In medicine and psychiatry the same process happens and I have pointed out the dynamic on this blog. I also posted a recent summary of how the release of the DSM-5 was a major source of misinformation, lies, and bullshit in 2015 but there are many more examples in psychiatry.
5. Don't let the barbarians at the gate get you down - I tell aspiring physicians and aspiring psychiatrists the same thing - don't let the detractors or in these days trolls - get you down. Psychiatry is a tough field because there will always be a lot of people blaming you for their problems. This is where Brandolini's Law really applies. There are numerous dialogues on web sites available where the game is to post as much misinformation, bullshit and lies about psychiatry in particular. Entire web sites exist for that purpose. Entering into that discussion and taking the opposite side of the argument can be more futile than the Law suggests. It may take several orders of magnitude of effort and even then it may be futile. The best approach is to just get the information out there in cyberspace in an independent forum where you know that it can be safely viewed. That is one of the reasons that this blog exists.
6. The Internet is still the Wild West and that will probably never change in its current form - Williamson suggests that it may be possible to "harness the collective power of the Internet to improve its quality." He suggests the global scientific community reviewing sites and rating them like film rating sites. I am far less optimistic. The first problem is the scope of that project. The second would be consistency in ratings. The third is that a rating in some sense is legitimizing. It is a far better approach to ignore the ignorant. The reality is that reputation protection web sites basically work by generating a lot of information designed to bury the obnoxious web site. Most people find that if they contact a search engine about a web site that may be slandering them that they are met with a a relatively hostile response and a complete lack of interest in correcting anything. That is true for even the largest search engines. Google for example, clearly doesn't give a damn about your reputation.
7. Brandolini's Law is a significant deterrent to keeping professionals engaged in educating the public - Physicians certainly find this out in a hurry if they decide to post a rebuttal in political or media forums that are populated by the ignorant, trolls, or those with a specific agenda. That is more true of psychiatrists than any other specialty. That has a dual effect of limiting feedback to those who might be interested and eliminating the most informed criticism. It also has the added effect of adding professionals who may have legitimate criticism to antipsychiatry web sites where scientific criticism is clearly not the agenda. It is a dangerous path of least resistance when legitimate professionals start posting on web sites dedicated to the destruction of the profession.
These are just a few ideas about Brandolini's Law. I did not write the most important one down and that is you can always just go off the grid. Even then there are problems. I talked with a psychiatrist about 10 years ago who was asked to give presentations at local churches on depression. He eventually gave up because there were people in the audience who for various reasons were so disruptive that it prevented him from giving the interested people the information that they wanted. Only psychiatrists could end up being heckled in church. Bullshit can be presented in person just as easily as is can by typed online.
Williamson refers to a "rising tide of populism threatens the future of evidence-based government." I don't think that we have ever had evidence based government in the US. I see it as mostly a power dynamic here - influencing people by emotional ideas and shouting them down.
The only reason why that Brandolini's Law doesn't work in reality in the case of psychiatry is that at the end of the day, there are still people with severe mental illness - no matter who tries to deny it and a group of people called psychiatrists who are interested in helping them. That is not necessarily enough to prevent the widespread demoralization of a profession.
George Dawson, MD, DFAPA
Reference:
1: Phil Williamson. Take the time and effort to correct misinformation. Nature 8 December 2016; 540: 171.
Supplementary 1:
My brother saw this post and commented that Brandolini's Law has "never been more true."
I reflected on that true statement and the continued widespread ignorance of science and came up with the following observation that might have been made by Casey Stengel:
"Good science cancels out bullshit and vice versa."
1: Phil Williamson. Take the time and effort to correct misinformation. Nature 8 December 2016; 540: 171.
Supplementary 1:
My brother saw this post and commented that Brandolini's Law has "never been more true."
I reflected on that true statement and the continued widespread ignorance of science and came up with the following observation that might have been made by Casey Stengel:
That probably captures why misinformation grows as exponentially as scientific information in any society. It levels the playing field (to some degree) between the informed and the uniformed.
Friday, December 9, 2016
Is The FDA Contraindication On Bupropion Wrong?
Since moving to a strictly outpatient consulting practice, I have been amazed at the number of women who are taking bupropion despite the above contraindication. I have probable seen 50 women who were under my care in this situation. In other words, I did not prescribe the bupropion and before seeing this would not have considered prescribing against an FDA contraindication. The patients I see often have additional contraindications including a history of seizures, sedative hypnotic drug withdrawal, or alcohol withdrawal. Seizures are the final common pathway for this subset of contraindications. I have never really observed a seizure from bupropion and the vast majority of the patients with the contraindications have never had a seizure. I have certainly observed and treated seizures in inpatient settings and understand that there is a low but significant risk of mortality with seizures. I have also not observed a significant complication of seizures, but at the time I worked in an inpatient hospital environment with rapid access to nursing staff, medications, and experts. None of the patients that I have initiated treatment on with bupropion have reported seizures, but I was strictly following the contraindication as listed in the FDA package insert.
My dilemma in this situation is always whether or not to continue the bupropion, especially when the patient tells me that it is the only medication that has been effective for them. Patients who are seen in their late thirties or later generally have been tried on numerous antidepressants from several classes and that complicates the clinical picture. Most of them have never seen a psychiatrist and all of the medication trials have been done by primary care physicians. It is common to see SSRI and bupropion combinations initiated by nonpsychiatrists. In my current capacity, I am not treating any of these patients long term. I see them anywhere from 1 to 3 months and at that time they return to see their personal physician or psychiatrist. I try to contact their personal psychiatrist about the issue but communication among physicians is often difficult to complete.
As I began to see more and more of these patients my first question was a scientific one. I was aware of the the trials that lead to the decision about eating disorders. There were all based on immediate release preparations rather than the sustained release (SR) or extended release (XL) versions. It certainly is possible that I am only seeing the success stories and that the patients with seizure related complications never come to my attention, but the practice of prescribing bupropion to a population that the FDA considers high risk seemed to be on the rise rather than decreasing. Is it possible that all of the other prescribers had also not heard of this complication. I knew that most of the patients were never apprised of the contraindication. I know that because I had them read the contraindication section of the package insert for themselves. Most would say that nobody have ever told them about this especially the part about any prior diagnosis of anorexia nervosa or bulimia. It is difficult to tell a 45 year old woman who had bulimia nervosa in college and recovered that the bupropion that she has been taking for the last 10 years without any side effects needs to be stopped because of this contraindication. The psychiatrists I talked with all minimized the wording in the warning. They ignored the part about "prior diagnosis". In fact some initiated treatment as the patient was completing treatment in a specialized eating disorders program.
I turned to the FDA web site for additional guidance on the agencies definition of contraindication. Was it as relative as these psychiatrists were telling me? It turns out the definitions used by the FDA in package inserts are defined in the Code of Federal Regulations (CFR). The section defining contraindications follows (p. 6 of 18):
(5) 4 Contraindications. This section must describe any situations in which the drug should not be used because the risk of use (e.g., certain potentially fatal adverse reactions) clearly outweighs any possible therapeutic benefit. Those situations include use of the drug in patients who, because of their particular age, sex, concomitant therapy, disease state, or other condition, have a substantial risk of being harmed by the drug and for whom no potential benefit makes the risk acceptable. Known hazards and not theoretical possibilities must be listed (e.g., if severe hypersensitivity to the drug has not been demonstrated, it should not be listed as a contraindication). If no contraindications are known, this section must state "None."
People seem to think that there is room for interpreting this definition of contraindication and it does beyond the APA Ethics Committee. I got the same opinion from an attorney. I also consulted a national expert on eating disorders. That expert opined that the contraindication was relative in both a history of eating disorders and acute eating disorders. The expert also had inside knowledge of why the FDA might have issued the contraindication in the context of scant evidence.
I have previously posted that the FDA seems to exhibit some biases when it comes to psychiatric disorders. In some cases they seem to not consider the severity of the the disorder in considering contraindications. There should be no question that eating disorders and depression are very serious conditions, serious enough that therapeutic options may include some risk.
In the meantime, I have decided to take some action. The FDA web site is a wall with no way in for people like me with a legitimate problem. I sent letters out to the US Senators from my state to try to find a way in. My goal is to get this contraindication taken out so it reflects current clinical practice and the experience of depressed patients with both a past history of an eating disorder or an eating disorder.
If you are a person with that history or a psychiatrist who prescribes bupropion in the face of this contraindication, please join me in advocating for this change.
George Dawson, MD, DFAPA
References:
1: Dunner DL, Zisook S, Billow AA, Batey SR, Johnston JA, Ascher JA. A prospective safety surveillance study for bupropion sustained-release in the treatment of depression. J Clin Psychiatry. 1998 Jul;59(7):366-73. PubMed PMID: 9714265.
2: Horne RL, Ferguson JM, Pope HG Jr, Hudson JI, Lineberry CG, Ascher J, Cato A. Treatment of bulimia with bupropion: a multicenter controlled trial. J Clin Psychiatry. 1988 Jul;49(7):262-6. PubMed PMID: 3134343.
Sunday, December 4, 2016
Please Use That CPAP Machine!
The best way to start out this post is by taking a look at the above graphic. This is the graphic of a 60 year old man with diagnosed obstructive sleep apnea who is using a continuous positive airway pressure (CPAP) machine. CPAP creates an airsplint in the airway to prevent airway collapse and snoring but more importantly hypoxemia due to obstruction. The bottom graph is downloaded from his CPAP machine and it shows the number of apneic and hypopneic episodes. What is not shown on the graph is that around October 12 this patient got an upper respiratory infection. As the nasal congestion worsened he changed his CPAP mask from nasal CPAP to a full face mask. He had a number of air leaks from this mask and as he found out later - he experienced nightly air leaks. Some of the air leakage was enough to wake up his wife who was sleeping in the same bed. As the hypopneic episodes worsened - he started to wake up with palpitations in the morning. The orange timeline shows that this patient developed atrial fibrillation for about 2 minutes on 10/28/2016 and 90 minutes on 11/15/2016. At that point he went in to see his pulmonologist the the AHI index was downloaded.
Sleep is a central part of any psychiatric evaluation. Many of my colleagues and residents have gone on to do sleep medicine fellowships and I think it is a logical career path for any psychiatrist. General psychiatrists need to know quite a lot about sleep and how to assess and treat sleep problems. During my assessments, obstructive sleep apnea (OSA) is a very common problem and it is a standard series of questions in my evaluation. I am consistently impressed with number of people who have already been diagnosed with OSA by polysomnography and prescribed continuous positive airway pressure (CPAP) devices who either do not use them or who just gave up trying to use them. There are a number of misconceptions about OSA and CPAP that I thought I might address in this post.
1. OSA is a benign condition:
The best way to start this discussion is to look at a complex graphic of the association of OSA and CPAP with atrial fibrillation - a known comorbidity of OSA. In this case we have a 60 year old man with a known diagnosis of OSA. He has been on CPAP for about 8 years. Before the OSA diagnosis he had an episode of paroxysmal atrial fibrillation while exercising. After starting the CPAP he was asymptomatic for 5 years before getting an upper respiratory infection and changing the mask he was using with his CPAP machine. The first papers on OSA and cardiovascular risk began appearing in the 1990s. Since then further research has demonstrated cardiovascular, endocrine, and cognitive comorbidity. Recent research suggests that severe but not mild to moderate OSA increases risk for all cause mortality (1). In the case of the above patient 40-50% of patients with atrial fibrillation have obstructive sleep apnea (2). In addition to clear disease states OSA puts people at increased risk for motor vehicle accidents and occupational hazards from both cognitive symptoms and excessive daytime somnolence.
2. CPAP is an elective intervention:
I am always shocked by the number of men who view a sleep study and the use of CPAP as elective procedures. I doubt that a lack of adequate explanation of the problem and its implications is the issue, especially once the diagnosis is made in a sleep lab. During my assessments I am often discussing chronic fatigue, insomnia, hypersomnolence, cognitive problems, depression, attentional problems and anxiety as prominent features of the disorder. The wish on the part of the patient is that I can give them a pill that will solve some of all of these problems. There was a time in the early days of OSA (about 1985) when a specific tricyclic antidepressant was thought to treat be useful in treating the disorder but that was disproven early on.
They have often been treated with sedative hypnotic or anxiolytic drugs for this same purpose. In some cases they are also taking opioid medications or muscle relaxants. Opioids have demonstrated dose-dependent respiratory ataxia (3). All of these medications decrease respiratory drive and either prolong apneic episodes or directly interfere with other respiratory mechanisms. Alcohol use is another complicating factor either by itself or in combination with other medications that adversely affect OSA or normal respiration.
3. If I lost some weight I probably don't need to use CPAP any more:
Although high body weight is a general feature of modern American society and some medications that are prescribed for psychiatric disorders can lead to significant weight gain and metabolic effects - many patients undergo profound weight changes in both directions. It is common to see patients with OSA who have had a significant weight loss and decided to stop using CPAP on that basis. They have not reconsulted with Sleep Medicine or had repeat polysomnography. They are placing too much value on the correlation between BMI and sleep apnea. Losing weight can result in resolution of OSA, but it is also possible to have OSA without obesity- suggesting that at a minimum Sleep Medicine should be reconsulted on the issue of discontinuing CPAP. The complex relationship between obesity and OSA was highlighted in a recent review (4). The authors point out that obesity, weight loss and sustained weight loss are difficult problems. Of the three controlled trials of a weight loss intervention there were improvements in AHI with weight loss and worsening of AHI with weight regained. They also looked at more extreme weight loss with with bariatric surgery and concluded that a drop of 1 BMI unit was associated with a 2.3 unit improvement in AHI, The authors compile a table of earlier studies that look at weight losses of 22% to 65% with accompanying improvement in AHI of up to 88%, but unfortunately in only 3 of those studies was AHI measured at < 5 or about 4% of subjects. In 18/19 studies the subjects had a post-op BMI of > 30. They conclude that the majority of bariatric surgery candidates remain overweight after the surgery and the many will still have moderate OSA and the need for CPAP. Their overall thesis is that OSA is a complex disorder and therefore no single intervention (like weight loss alone) can be used.
4. If I am not snoring as much - I don't need to use CPAP any more:
Snoring is caused by vibration of the same upper airway tissues that are involved in the obstruction. Snoring can be caused by number of acute and chronic conditions as well as being an artifact of normal genetically determined anatomy. More men and women snore than have sleep apnea. In many people snoring is positional and occurs much more often in the supine than side sleeping position. Snoring also depends on detection. Snoring and apneic spells directly observed by a sleep partner are more diagnostic than self report of waking up gasping or snoring - although those reports should also be investigated. Snoring - like body weight is an approximate correlate of OSA and the decision to stop CPAP should be made with the assistance of a Sleep Medicine physician. Modern CPAP equipment can provide a significant amount of in home data to assist with that decision.
These are a few considerations about the diagnosis of OSA and prescription of CPAP. Any person seeing me is strongly encouraged to do whatever is necessary to use their CPAP machine and reduce risk factors including any unnecessary medication that may affect respiration. I may be reluctant to consider some therapies that while not directly impacting on respiration may have some effect due to synergies with other compounds (like antidepressant and trazodone combinations for sleep). You can also count on hearing about comorbid conditions (like the atrial fibrillation in this case) that are clearly affected by OSA.
So if you have that diagnosis and had a CPAP machine - please use it. The modern autotitrating machines are much easier to use and allow for direct patient access to the data. It is now possible to download a smartphone app and get your relevant sleep data directly from the SD card on your machine in the morning. That gives you immediate detailed information on how you slept, what your AHI was, how the mask performed and what corrective action might be required. In some cases it allows your Sleep Medicine physician to adjust your machine setting remotely to optimize therapy and reduce the need for office visits for that purpose.
Sleep better and live better.
George Dawson, MD, DFAPA
References:
3: Walker JM, Farney RJ, Rhondeau SM, et al. Chronic Opioid Use is a Risk Factor for the Development of Central Sleep Apnea and Ataxic Breathing. Journal of Clinical Sleep Medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2007;3(5):455-461.
4: Romero-Corral A, Caples SM, Lopez-Jimenez F, Somers VK. Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest. 2010
Mar;137(3):711-9. doi: 10.1378/chest.09-0360. Review. PubMed PMID: 20202954; PubMed Central PMCID: PMC3021364.
5: Phillips B. Kryger MH. Management of obstructive sleep apnea hypopnea syndrome. In: Kryger MH, Roth T, Dement W, eds. Principle and Practice of Sleep Medicine, Fifth Edition. St. Louis, Missouri: Elsevier Saunders, 2011: 1278-1293.
Supplementary:
Some sleep medicine definitions used in the above post. For more technical definitions see reference 5 above:
Apnea: Cessation of airflow for at least 10 seconds. The technical definition depends on the sensors used for this measurement such as a drop in thermocouple excursion by 90% for 10 seconds. The thermocouple in this case would be measuring the temperature of exhaled air. Obstructive apneas are present when there is inspiratory effort during the apnea and central apneas are present when there is none. There can also be mixed apneas.
Hypopnea: Shallow breathing or a low respiratory rate for 10 seconds. The technical definition again depends on the equipment usually defined as a drop in nasal pressure excursion and a percentage of hemoglobin saturation.
AHI: Apnea Hypopnea Index - an index of severity of OSA defined as the number of apneic and hypopneic episodes per hour. The general goal of therapy is to have an AHI of less than 5.
BMI: Body mass index or weight in kilograms divided by the square of height in meters. Several sites like the CDC offer BMI calculators and brief instructions on how to interpret these numbers. Higher BMI and neck circumference increases the risk of OSA.
Subscribe to:
Posts (Atom)