The Door County Summer Institute (DCSI) was founded by Medical College of Wisconsin Professor Carlyle H. Chan, MD. It is held at the Landmark Lodge in Egg Harbor, Wisconsin. Egg Harbor is one of many small towns that dot the Door County peninsula bordered on the west by Green Bay and on the east by Lake Michigan. If you have a lake view from the Lodge, there is generally an unobstructed view of the expanse of Green Bay with a few visible islands on the horizon. The weather this time of the year is tropical for the midwest with temperatures in the 80s and the occasional thunderstorm.
The DCSI is a psychiatry conference and most of the people who attend are psychiatrists but there are also psychologists, social workers, NPs, PA-Cs and nonpsychiatrist physicians. The programs are very eclectic with topics ranging from psychopharmacology to terrorism. In the course I have attended there have been 1 to 3 instructors. The instructors are all generally considered to be experts in the fields they are presenting. The courses are generally 2 days in duration (mornings only) with plenty of discussion about places to see in the area that include, restaurants, art galleries, concerts, plays, and musical productions.
As I mentioned in a previous post, I attended four sessions on
Practical Neuropsychiatry for Clinicians presented by Sheldon Benjamin, MD. I consider myself to be a neuropsychiatrist. Early in my career, I attended behavioral neurology conferences and ran an Alzheimer's Disease and Memory Disorder Clinic co-staffed by a neurologist for about 12 years. I also evaluated neuropsychiatric problems in acute care settings. My hope was to get some complementary knowledge from an expert with a different career path and I was not disappointed.
The first session was spent on an overall neuropsychiatric approach to the patient and Dr. Benjamin made the observation that
neuropsychiatry is personalized medicine in that each formulation is uniquely developed for the individual and it also answers the question about what treatment will help that unique individual. On that basis, is is
not a nonspecific
label. His reasoning can be extended to the psychiatric formulation in general. As previously noted on this blog, a formulation is the most unique aspect of the evaluation and it needs to be included as well as the diagnoses. Any psychiatrist knows that people with the same diagnoses are unique individuals and that the diagnosis alone does not take into account the unique conscious states of individuals any more than any other medical diagnosis.
From there most of the rest of the first day was spent on a discussion of frontal lobe function and executive function. Rather than focus on the consensus list of neuropsychological tests thought to comprise executive function, he presented an adaptation of D. Frank Benson's schema to illustrate the basic dimensions (anticipation, monitoring) involved in goal selection and planning and the underlying behaviors. He emphasized the assessment of frontal function as being possible without any specialized testing and illustrated the point with a humorous example (1). Executive function was primarily a product of prefrontal cortical function but parietal cortex and cerebellar cortex were also involved on the basis of an analysis of cognitive and neuroimaging articles (2).
There was an emphasis on practical assessment frontal lobe
function and more specifically the ecological validity of the tasks. In other
words what do the tests mean in real life. The MoCA Test was used to illustrate
that tests of frontal executive function do not require any special equipment.
The trail making, clock drawing, and verbal fluency sections were highlighted
as requiring frontal executive function. The MoCA Test was described as
potentially problematic due to the new licensing procedure. Dr. Benjamin
presented several other tests that could be added to the bedside exam that
included both neurological examinations of for example anti-saccades and more
complex cognitive tasks such as complex problem-solving, inferential reasoning,
the script generation task, and a headline task. After the presentation there was
a brief workshop where patient was presented and participants needed to pick
one behavioral problem, develop a hypothesis, and suggest what tests could be
used. The ultimate goal was to consider
not just a useful test, but also potential rehabilitation approaches. A total
of 16 cognitive domains and 30 cognitive tasks were provided that could be used
to develop specific tests.
The final section of the first two days was about traumatic
brain injuries. I have a previous post
on an application from this section on classifying the severity of these
injuries. The epidemiology is striking
with a prevalence equivalent to patients with severe mental illnesses. The death rate is about 50,000 people per
year and at 1 year a many as 15% of people with a mild TBI remain
symptomatic. The myth discussed is that
we all grow up thinking that TBIs are relatively benign. I see that occurring regularly in the
patients I assess who have had multiple TBIs or concussions and who never saw a
physician for assessment. In many cases they resumed playing the sport immediately
where they were injured. That is a very
high-risk scenario. The
coupe-contre-coup injury was discussed as well as how to identify it on brain
imaging studies and autopsies. Several
specific mechanisms of injury were discussed including diffuse axonal injury
(DAI) and how that occurs during TBIs.
Shear forces used to be considered the main mechanism of injury but now
permeability changes are thought to occur that leads to lysis of axons in the
12-24 hour window.
Second Syndrome or Second Impact Syndrome was
mentioned as a complication of returning to play too soon and sustaining a
second concussion with a resulting massive injury. It apparently based on a 1984 report (3)
where a football player sustained a concussion in a fight and then another
concussion 4 days later playing football.
That second injury resulted in massive cerebral edema and death. The
purported mechanism is a vulnerable window of decreased brain metabolism. Concussed athletes have been examined with MR
spectroscopy. In this method, N-acetylaspartate
(NAA) is a marker of neuronal viability. Following concussions, NAA is
depressed to the lowest at about three days after the injury and it recovers by
30 days. In another study, if a second
injury occurred before 15 days – recover of the NAA marker did not occur until
45 days. Some sources consider this
syndrome to be controversial due to recall bias and a lack of reported cases in
other literature, but the depression of brain metabolism is concerning. Clinical symptoms of TBI may be underreported
or not reported at all during this recovery phase.
In the section on specific frontal syndromes, Dr. Benjamin
pointed out that he was pleasantly surprised by the Neurocognitive Disorders
section in the DSM-5. I agree with his
observation. There is highly detailed information about making those diagnoses
and what information is relevant. For the course he looked at personality changes
associated with various frontal syndromes such as orbitofrontal syndrome,
prefrontal syndromes, mixed frontal syndromes, ventromedial syndromes, and
secondary mood disorders.
That last two days of the course were focused on memory,
encephalitis lethargica, autoimmune syndromes, and the six landmark cases
necessary for neuropsychiatric literacy.
I will end with a summary of the six cases because for most readers of
this blog – they are readily accessible in the paper written by Benjamin, et al
(4). His discussion of the Phineas Gage case was remarkable given the amount of misinformation that exists. He presented a detailed timeline of the injury and how Gage was treated initially by the town physician and then by the railroad physician. New England Journal of Medicine subscribers may be surprised to learn that they have access to the full text of an 1848 account from attending physician Dr. Harlow (5). There are
43 references in the medical literature. For anyone not familiar with the case, he sustained a penetrating wound to the brain when a 43 inch, 13.5 pound iron rod used to tamp sand and gunpowder into a hole for excavating rock was propelled through his left orbit and left frontal lobe exiting out the top of his skull. Dr. Benjamin pointed out that there are numerous false accounts of the incident and I had read several suggesting that the rod had to be extracted from Gage's skull by the doctor in attendance. In fact, the rod blew through his head an landed about 30 feet away. The rod had been specially designed by Gage so that one end was tapered for prying. That is what led to the penetrating wound and is also what saved him. The year of this injury was 1848, before antibiotics and neurosurgery. Gage was transported to a hotel where he stayed and was able to walk up to his room on the second floor where he experienced transient delirium but he was able to recover and return home after 74 days. There are numerous accounts of his neuropsychiatric recovery. The commonest description is that he was "no longer Gage". He could no longer work as a railroad foreman, but sometime later traveled to Chile where he was a stagecoach driver managing a 6-horse stagecoach. He died about 12 years after the injury from
status epilepticus. The index case of severe frontal lobe damage illustrates preservation of cognitive and motor skills with some personality changes.
In conclusion, I
highly recommend Dr. Benjamin’s work and this course if you ever want to attend
a DCSI. More to the point, I highly
recommend that medically oriented psychiatrists develop skills in
neuropsychiatry by working these principles and skills into their practice like I
have over the past 30 years. When I say
medically oriented psychiatrists, I am generally referring to acute care
psychiatrists (inpatient, addiction and consultation liaison) and outpatient
psychiatrists who are seeing patients as identified as having cognitive
problems and possible dementias like geriatric psychiatrists or psychiatrists
who specialize in treating people with complex medical and psychiatric
problems. In my situation seeing inpatients with a variety of complex problems,
making associated medical diagnoses, and working closely with other consultants
was very effective in reaching this goal. An additional skill was reading all
brain imaging and taking an early interest in EEG and QEEG. Seeing all of the brain imaging of patients
has never been easier than with the current EHR. When we were using only paper records, I
would often trace an axial section of a CT or MRI and put that in the
patient’s chart but now it is right there.
I think it is also a critical factor in deciding what an ultimate practice
environment must look like for psychiatrists interested in this type of
practice. Th environment has to provide access to the necessary imaging,
neurophysiological, and laboratory testing as well as easy access to other consultants. Complex problems require an environment where
they can be addressed. Many current
practice environments for psychiatrists do not provide access to these tools or
state-of-the-art treatment modalities. In many of these settings it is difficult to find a working blood pressure device.
Given the appropriate medical setting, there has never been
a better time to be a neuropsychiatrist and train neuropsychiatrists for the
future.
George Dawson, MD, DFAPA
References:
1: Rockwood K, Chertkow H. A cellular-telephone model of assessing frontal lobe function in physicians. CMAJ. 2007 Dec 4;177(12):1533-5. PubMed PMID: 18056616.
Link (full text)
2: Nowrangi MA, Lyketsos C, Rao V, Munro CA. Systematic review of neuroimaging correlates of executive functioning: converging evidence from different clinical populations. J Neuropsychiatry Clin Neurosci. 2014 Apr 1;26(2):114-25. doi: 10.1176/appi.neuropsych.12070176. Review. PubMed PMID: 24763759.
Link (full text)
3: Kamins J,
Giza CC. Concussion-Mild Traumatic Brain Injury: Recoverable Injury with
Potential for Serious Sequelae. Neurosurg Clin N Am. 2016 Oct;27(4):441-52. doi:
10.1016/j.nec.2016.05.005. Review. PubMed PMID: 27637394; PubMed Central PMCID:
PMC5899515.
Full Text
4: Benjamin
S, MacGillivray L, Schildkrout B, Cohen-Oram A, Lauterbach MD, Levin LL. Six
Landmark Case Reports Essential for Neuropsychiatric Literacy. J Neuropsychiatry
Clin Neurosci. 2018 Fall;30(4):279-290. doi: 10.1176/appi.neuropsych.18020027.
Epub 2018 Aug 24. PubMed PMID: 30141725.
5. Harlow JM. Passage of an Iron Bar Through the Head. The Boston Medical and Surgical Journal. 1848 XXIX(20): 389-393.
6: Damasio H, Grabowski T, Frank R, Galaburda AM, Damasio AR. The return of Phineas Gage: clues about the brain from the skull of a famous patient. Science. 1994 May 20;264(5162):1102-5. Erratum in: Science 1994 Aug 26;265(5176):1159. PubMed
PMID: 8178168.
7: Haas LF. Phineas Gage and the science of brain localisation. J Neurol Neurosurg Psychiatry. 2001 Dec;71(6):761. PubMed PMID: 11723197; PubMed Central PMCID: PMC1737620.
Full Text
Supplementary 1:
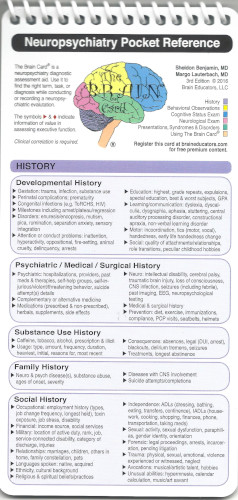
Don’t forget
Dr. Benjamin’s
Brain Card as an excellent resource. The nominal cots is used to fund a web site
that provides free access to additional clinical resources that are available
to
Brain Card holders for free.
Supplementary 2:
I anticipate some complaints from psychiatrists who will say that they do not have enough time to do detailed assessments like the ones suggested in this post. Despite the penetration of managed care and the fact that most physicians are employees, I contend that it is still possible to do detailed and intensive evaluations on patients with complex problems. My strategy for a long time was to do inpatient work where I could see people as many times a day as I needed to an I had access to resources like EEG labs and imaging studies. The ability to meet with families for a more in depth analysis of the problem was also a plus. Choosing the correct work setting goes a long way toward allowing this kind of work.