Sunday, June 11, 2017
Lithium and Pregnancy - The Latest From the NEJM
Lithium and pregnancy have always been a major concern for psychiatrists, obstetricians, and of course women who need to take the medication for mood stabilization. In the Lithium Encyclopedia (published in 1983) - there is a chapter on the physiological effects of pregnancy and how that potentially affects lithium balance and a separate chapter on teratogenesis. That chapter describes the Lithium Baby Registry that was established in 1970 to collect information on the effects of lithium in pregnancy. In the first 10 years, 225 infants exposed to lithium were described and 25 had congenital malformations. Of these births 18/25 had cardiovascular abnormalities including Ebstein's anomaly, 7 were stillborn, 2 had Down's syndrome and 1 had intracerebral toxoplasmosis. The results suggested that lithium was a cardiovascular teratogen, but there was a question of reporting bias. That is, results consistent with the study concern about lithium being a teratogen were more likely to be reported than normal births.
Those references set the knowledge about lithium and pregnancy for all residents trained in my era in the late 1980s. The standard question by attendings and on examinations was: "What is the cardiac anomaly associated with intrauterine exposure to lithium?". The answer was Ebstein's anomaly. The follow up question was expected: "And what is Ebstein's anomaly?" In those days the short answer was downward displacement of the tricuspid valve into the right ventricle. Today Ebstein anomaly (no longer a possessive) is described in greater detail. A modern reference describes the extension of the tricupsid valve into the right atrium to the extent that most of the functional chamber chamber is collapse to a very small volume. In some cases it is collapsed to the right ventricular outflow tract. The downward valve displacement is due to a number of morphological abnormalities in the tricuspid valve. The myocardium is also abnormal because the valve tissue has failed to completely separate from the myocardium during fetal development - a process called delamination. That is associated with a thin and poorly contractile myocardium and poor right ventricle performance. There are several associated cardiac abnormalities including ventricular septal defect, patent foramen ovale, patent ductus arterious, and accessory conduction pathways that can lead to arrhythmias. The associated clinical syndromes of cyanosis, congestive heart failure and arrhythmia can occur in infancy to adulthood depending on the degree of anatomical disruption. The complications can be fatal at any age (2).
Ebstein abnormality is a preventable complication and one that must be avoided. In real life that is easier to say than do. In a controlled hospital or clinic environment it is a very straightforward process to take a history and determine the obstetric history and last menstrual period. Urine and serum pregnancy tests can be done for confirmation. The best advice to physicians in this situation is to treat very woman of childbearing age as if they were pregnant until proven otherwise. In my experience life is less regimented. There are lapses in contraception and planning that lead to pregnancies in women taking lithium who know that exposure to the infant is an avoidable risk. Many of these women are on lithium maintenance. Since lithium remains a mainstay of treatment for bipolar disorder and may be a superior agent in postpartum psychosis - the question of teratogenicity remains an important one.
There have been a number of estimates of congenital malformations due to psychiatric medications and I recently reviewed a few of them and cited extensive database references. In one of the reviews very large databases were examined looking for major congenital malformations to lithium exposed women especially Ebstein anomaly.
The New England Journal of Medicine published another large retrospective database study of the question of lithium exposure in pregnancy and risk of cardiac malformations. Their database involve a Medicaid cohort of 1,325,563 pregnancies over the ten year period between 2000 and 2010. In this cohort there were cardiac malformations noted in 16 of 663 (2.4%) lithium exposed infants. Lower rates of cardiac malformations were noted in nonexposed infants (1.15%) and lamotrigine exposed infants (1.39%). In addition there appeared to be a dose related effect with increasing risk ratio noted with increasing doses of lithium. For example at the dose of 600 mg or less/day the risk ratio was 1.11 but the risk ratio increased to 1.11 and 3.22 for doses of 601-900 mg/day and greater than 900 mg respectively.
The authors have a detailed report on how the cardiac malformations were determined. They make an interesting point that a misclassification bias can occur with Ebstein anomaly. Some clinicians may make the diagnosis of right ventricular outflow tract obstruction defects or Ebstein anomaly based on whether or not there has been a history of exposure to lithium. That may make it more likely to misclassify Ebstein anomaly. They provide data for the total prevalence of all cardiac malformations and cardiac malformations classified as right ventricular outflow obstruction. They were focused on "major cardiac defects that were likely to be consequential for the infant." The diagnostic codes had to be listed several times or associated with surgery.
The calculated prevalence of Ebstein abnormality in unexposed pregnancies was 7 cases per 100,000 live births. They did not provide the prevalence of Ebstein anomaly in the lithium exposed due to the low number. After a detailed analysis and analysis of possible sources of error like terminate pregnancies where lithium exposure occurred the authors conclude that lithium had a modest effect in terms of increased risk of cardiac malformations. Their final estimate was an increased risk of 1 additional case per 100 live births if the exposure occurred early in the pregnancy. They describe this as a modest increase in risk of cardiac malformations due to lithium. The difference in the ratio of cardiac malformations in this study (16/663) compared with the Lithium Baby Registry (18/225) is probably due to a more rigorous methodology.
The authors looked at five sources of error in their final discussion of the results. For clinical psychiatrists the most relevant point was that other factors affecting treatment decisions in pregnancy were not investigated. They are considerable given that it is highly likely that the women being treated with lithium have severe mood disorders and suicide in the postpartum period in the number one cause of death. This study can best be viewed as a study that supports current clinical practice to avoid first trimester exposure to lithium by careful screening and then planning if additional adjustments need to be made for planned pregnancies based on the trimester. In those cases of accidental exposure, consultation with high risk obstetrics and a decision based on a detailed discussion with the patient is usually the preferred option.
George Dawson, MD, DFAPA
References:
1. Jefferson JW, Greist JH, Ackerman DL. Lithium Encyclopedia for Clinical Practice. Washington, DC; American Psychiatric Press, Inc., 1983: 264-265.
2. Connolly HM, Qureshi, MY. Clinical manifestations and diagnosis of Ebstein anomaly. In UpToDate, Greutmann M, Fulton DR, Yeon SB (Accessed on June 9, 2017).
3. Patorno E, Huybrechts KF, Bateman BT, Cohen JM, Desai RJ, Mogun H, Cohen LS, Hernandez-Diaz S. Lithium Use in Pregnancy and the Risk of Cardiac Malformations. N Engl J Med. 2017 Jun 8;376(23):2245-2254. doi: 10.1056/NEJMoa1612222.
Saturday, June 3, 2017
Enhancing The Volkow-Collins Approach To The Opioid Epidemic
Nora Volkow, MD - Director of the National Institute on Drug Abuse and Francis S. Collins, MD, PhD - Director of the National Institutes of Health co-authored a paper on the role of science in the current opioid crisis. Full text of the article is available free online from the New England Journal of Medicine at the reference given below. In the article the authors review the scientific interventions at three levels of care in treating opioid addiction and use, treating and preventing overdoses, and the treatment of chronic pain. The treatment of chronic non-cancer pain (CNCP) with opioids can be realistically viewed as the precipitant of this epidemic. The brief 4 page review is a good rapid review of the science behind these interventions. The level of cooperation between NIDA and NIH with private industry may surprise a few people but as the authors point out - the level of mortality with the current epidemic needs to be approached with urgency at all levels.
At the level of opioid overdose prevention and reversal - more potent and long lasting opioid antagonists are being developed to counter exposure to fentanyl and carfentanil appearing at an increasing rate on the street. Narcan Nasal Spray is probably the most effective and practical outcome of the industry-NIDA partnership. A wearable device that can detect signals of an impending overdose and administer a μ-opioid receptor antagonist is mentioned. At the level of addiction treatment methadone, buprenorphine, and extended-release naltrexone are all mentioned as current treatments for opioid use disorder. Access to providers is discussed as a limiting factor. vaccines and novel receptor approaches are discussed as potentially new pharmacological approaches to the problem. New approaches to chronic pain are discussed in greater detail. Cooperation between the NIH and industry is emphasized again in terms of getting these approaches to market and clinical use. In the concluding section - the emphasis on NIH-industry partnerships is a central theme. The argument makes imminent sense, but after two decades of rancorous debate about the effects of pharmaceutical company pizza on prescribing - this level of access to the highest level of taxpayer funded research is somewhat stunning.
But what else might be immediately useful? I can concentrate just on buprenorphine and come up with a couple. Anyone working with this compound and people who are addicted to opioids routinely encounters problems with its use. It is common to treat people who still have withdrawal symptoms and cravings on the recommended doses and remain at high risk for relapse even after being treated with what is described as one of the best current therapies. Taking a look at the recommended dose range from the package insert:
The upper limit of the recommended dose is 24mg/6mg buprenorphine/naloxone per day for SUBOXONE. The reported lack of significant increase in brain mu‐receptor occupancy between doses of 16 mg and 32 mg implies that there should be little difference in clinical effectiveness at doses between 16 mg and 24 mg in most patients. When a patient expresses a need for a higher dose, consider the possible causes (e.g., environmental stressors or psychosocial issues that increase cravings or possible drug interactions). Before increasing the patient’s dose, explore other alternatives. Also consider the possibility that the patient may be exaggerating symptoms to obtain additional medication for diversion. (p 34-35).
And:
The recommended target dose is 16 mg buprenorphine/4 mg naloxone per day. Clinical studies have shown that this is a clinically effective dose. Although lower doses may be effective in some patients, for most patients, a 16 mg dose should alleviate withdrawal symptoms and block or attenuate the effects of other opioid agonists for at least 24 hours. (p. 34)
In clinical practice there is a wide range of effects to buprenorphine doses. The FDA approved considerations show the subjectivity involved in adjusting the dose. But that is even an understatement. There needs to be a much greater investigation of the causes of continued craving and withdrawal symptoms when the patient is taking a recommended dose of buprenorphine. This may be a genetically determined phenomenon either at the pharmacokinetic or pharmacodynamic level. That is only partially accounted for by drug interactions.
Investigation of withdrawal symptoms and continued craving is more than just a passing concern. It potentially determines who will be able to remain on maintenance therapy and stay off of heroin. It is important because a significant number of these patients are being actively treated for psychiatric disorders with antidepressants, anxiolytics, atypical antipsychotics and mood stabilizers. How much of that medication use is due to inadequate treatment with buprenorphine and the common symptoms of insomnia, anxiety, and depression associated with opioid withdrawal. These are all very complex clinical situations. Many of these patients have a life long history of stress intolerance and there can be a reluctance on the part of clinicians especially if they have no mental health training to explore and treat those problems. Once the patient has been indoctrinated into the idea that a maintenance medication is going to help them stay off heroin - it is a difficult transition to now say that all of these other factors are now important and need to be addressed. That is especially true when some of the existing buprenorphine studies minimize counseling or are publicly presented as "counseling adds nothing to the results obtained with buprenorphine." Finally, there is a large social media movement of people who want to stop buprenorphine and are warning others about it. What is behind this widespread dissatisfaction and what needs to be done to resolve it? The overall impression that all of the issues in this paragraph leaves is that buprenorphine is another heavily hyped medication that does not live up to the claims. All of these areas could use much clearer input from NIDA through additional scientific investigation.
Additional studies on drug interactions with buprenorphine are critically needed. I use a standard commercially available drug interaction software package. Any time I enter a psychiatric medication I get a warning to consider to modify therapy and a list of 230 potential drug-drug pharmacodynamic interactions at the CNS level. Since there is a high prevalence of patients on maintenance psychiatric medications this represents a deterrent to some physicians, especially if they are not psychiatrists and they are in a state with an unfavorable malpractice environment.
The next issue is determining who is susceptible to opioid overuse and dependence. In my mind the phenotype is very clear. The person who takes the first opioid tells me that they either "fall in love with it" or they experienced an intense euphoric and almost hypomanic effect. They felt transformed by the medication into a person that they had always wanted to be. Side effects are modestly effective deterrents, but I have been told that side effects and a complete lack of analgesia are acceptable in order to get the intense, euphoric high. How can these people be identified? The authors discuss biomarkers for pain and pain relief - but the single-most important biomarker would identify this high risk group of patients for addiction. There are currently commercial databases out there that poll their members on various traits and symptoms. Can NIH or NIDA design the polling questions and look for markers in these existing databases?
Even before that marker is identified, is there a simple strategy that could be used in clinical practice? Could a clinician tell a patient to self monitor for the intense euphoria and report back to the physician as soon as possible if it occurs? Could the patient be told to just dispose of the pills by bringing them in to the pharmacy if euphoria and thoughts of dose escalation occur?
These are some thoughts that come to mind that might be immediately useful. They would address both the limitations of medication assisted treatment and identifying the at-risk population for primary prevention of opioid use problems.
George Dawson, MD, DFAPA
Wednesday, May 31, 2017
Lawyers, Libertarians, and Journalists On the Opioid Epidemic
It was a perfect confluence of events today. At one point or another I heard or read about somebody's theory of why there was an opioid epidemic, deaths from drug use, and who was to blame. Although some of the discussants were quite heated they all had one thing in common - they were all dead wrong.
Let me start with the lead story - the Attorney General of the State of Ohio suing drug manufacturers for the massive opioid problem in that state. I say massive because there are an estimated 200,000 opioid users in the state and an associated mortality. If you listen to the story (1) many local coroners and morgues are overwhelmed by the body count. I heard the story on Minnesota Public Radio on the drive home tonight. Ohio Attorney General Mike DeWine is suing Purdue Pharma, Johnson & Johnson, Teva Pharmaceuticals, Endo Health Solutions and Allergan for their role in the opioid epidemic. Apparently the state of Mississippi filed the first law suit in the area. The AG alleges that these companies basically convinced physicians through their questionable marketing efforts that these drugs were much safer than they really were and more effective for the conditions that they were supposed to treat. Robert Siegel the reporter made an attempt to blame physicians instead and asked why they were not named in the law suit. The AG's position was that the culture of medicine was affected by the false promotion and that it will take a while to change things around. See the press release here for the exact position of the AG. A copy of the entire complaint by the AG is available here.
The second story (2) came to my attention on my Facebook feed. This was a case of Ross Ulbricht - who was apparently convicted and sentenced to life in prison based on operating a darknet market that he created called Silk Road. The conviction was apparently for money laundering, conspiracy to traffic narcotics, and computer hacking. My interest in this case has nothing to do with the charges, the defendant himself, the conviction or the sentencing but the reaction on various web sites about the case. There is a consensus on some of these web sites that he was offering valuable service for adults who want to come together and freely exchange items that it might be difficult for them to exchange in other places. The associated arguments are that competent mature adults should be able to do this, that any interest the state has in suppressing such activity is an inappropriate intrusion on individual rights, and that in fact a service like this was essentially competing against cartels and may put them out of business. Some suggested that there was a conspiracy between the state and cartels to put sites like this out of business.
All of these arguments fall flat to an addiction psychiatrist like me. They seriously underestimate the effect that an addiction has on the brain and conscious state of an addicted individual. Imagine what it is like to get out of bed in the morning and the very first conscious thought is: "How can I score some dope today so that I can function?" At that stage you are no longer a competent adult able to weigh decisions and make them in your best interest. All of your decisions are weighted in the direction of ongoing drug use and addiction. That is true if you are on the darknet looking for drugs or standing on a street corner in Ohio. That is true if you are sitting in a physician's office and telling them what you think they need to hear to enable them to prescribe you more opioids.
The second aspect of opioid addiction that is difficult to understand is the genetic predisposition to addiction. There are still a lot of pop psychology theories about addiction being just a bad habit or a lack of moral character that seem to explain the differences between people with addiction and people without addictions. The fact is a substantial part of the population is genetically vulnerable to addiction and it is just a matter of whether or not they are exposed to a highly addictive drug. If I had to estimate, my best guess would be that number is at least 40% of the population. By that I mean that 40% of the population will get an extremely euphorigenic response to opioids (whether or not they work for pain). They will remember that response and if exposed to more opioids are much more likely to use them than not use them.
That is what makes it so hard to stop this epidemic. Without those two basic features of addiction there is no unlimited demand for addictive medications from pharmaceutical companies. There is no need to go to a part of town that a person would never typically travel in to purchase diverted prescription opioids or heroin. There is no need to search out opioids or other addictive drugs on the Internet or the dark net.
Doctors don't get off the hook. All physicians are taught about controlled substances and the schedule of controlled substances. All physicians know that opioids are scheduled according to their addictive potential. The problem is that most physicians do not know how to interact with people who have significant addictions, and even experts can be fooled. Most physicians have an incredibly naive approach to addiction and how they can prevent it or approach it once it is established. The cultural norm that physicians help people by prescribing them medications, combined with the fact that physicians are trained to help people, creates a powerful force to continue to prescribe addictive pain medications. The absence of competent detox facilities is another.
Pharmaceutical companies, doctors, judges and prosecutors - the pro and anti-blame rhetoric around this issue is intense and unrelenting. It is not any easier to stop the current opioid epidemic when lawyers, libertarians, and reporters are spreading the blame around to anyone or anything other than the real cause of the problem - the addiction itself.
Start there - treat it as a public health problem and start to make progress.
George Dawson, MD, DFAPA
References:
2: Brian Doherty. Ross Ulbricht Loses His Appeal Over Conviction and Sentencing in Silk Road Case. Hit and Run Blog. Reason.com May 31, 2017.
Supplementary:
A reminder about the Ross Ulbricht case. I am not focused on the case per se or the War on Drugs. I am solely focused on the argument that anything can be openly traded on a market between consenting adults. I do not dispute the argument that the sentence was excessive or any other arguments for that matter.
Minnesota Street Drug Bulletin - Designer Benzodiazepines
 |
| Benzodiazepine structures clonazepam (upper left) and alprazolam (lower left) are both prescription benzodiazepines. Clonazolam (upper right) and etizolam (lower right) are not. |
Designer benzodiazepines are benzodiazepine class drugs that are not approved for therapeutic use in any country. They are analogues that were synthesized by drug companies, and in some cases went to clinical trials and published results but never made to to market. The name makes is seem like there are chemists out there synthesizing these drugs for a purpose, but there are not. They are all part of the original research for benzodiazepine class medications that has not really seen any innovation in decades. These drug are a current problem because there are online sources allow people to purchase them in tablet, capsule, powder, and blotter form. There are several online venues where users talk about their experience and which drug creates the "best" high. Medical staff need to realize that many of these drugs are undetectable as molecules. They show up as "false positives" in standard toxicology testing largely due to a lack of reference material. Drug users are often told that the drug is undetectable in standard toxicology assessments and that the drugs are also not listed as a standard prohibited substance and therefore it is a "legal" high. That is a fairly weak argument when users are overtly intoxicated and sustain all of the consequences of intoxication.
Just as a check I looked at a list of 13 designer benzodiazepines (1) (clonazolam, deschloroetizolam, diclazepam, estazolam, etizolam, flubromazepam, flubromazolam, flutazolam, 3-hydroxyphenazepam, meclonazepam, nifoxipam, phenazepam, and pyrazolam) and compared them to the most recent posted list of Controlled Substances from the DEA. Only one of those compounds (estazolam) is listed on the most current list dated 05-May-17. It is listed as a Schedule IV drug. I have no way of knowing which compounds are being considered for the list. Just being on the list does not deter the illegal sale of controlled substances, but the designer designation generally means that there is far less known about the drug in terms of safety. In some cases the toxicology lags behind exposures because the physicians treating intoxication, withdrawal, and overdoses with these compounds are uncertain about what they are treating. The patient or collateral contacts of the patient may not know what the drug is and that lag time creates additional danger for the patient.
The first time I searched for clonazolam on Medline, I was impressed with the fact that there were only 5 references in the medical literature including the analysis reference that listed 13 designer benzodiazepines. In fact, they all had to do with analysis but also described the complications of intoxicated driving (2) while taking them and the complications of life threatening intoxication (3). The minimal online information available suggests that it has very high potency. There are doses suggested in the range of high potency benzodiazepines but there are no clinical applications. As a result, there are no FDA package inserts or even reliable data from other agencies. It is not listed in the British National Formulary (bnf.org). Despite this lack of clinical information and application, it is immediately obvious that large quantities are available for purchase online. On these sites it is described as a research chemical with no clinical applications. It is also described as not for human consumption - a label I am familiar with from synthetic cannabinoids. The current problem is that as long as this chemical or its precursors are not listed as controlled substances anyone can purchase it for any purpose. The suggested prices quoted for this drug are far below the street price of diverted prescription benzodiazepines. That makes these compounds ideal for illegal trafficking.
Searching etizolam on Medline resulted in 96 references and 13 clinical trials. Some of the trials were as recent as 2009. The trials were for anxiety disorders and based on the abstracts the results sound equivocal ranging from improvement over 4 weeks to (4) to no improvement (5). The striking feature of the trials is the dose of etizolam being 0.5 mg BID indicating that it is a high potency benzodiazepine. The fact that several studies were done and the drug was never approved suggests either the lack of sufficiently powered studies or some side effect that was obvious only to the pharmaceutical company or regulators. In some cases the drug is also too difficult to use clinically. There are several examples of benzodiazepine class medications that were determined to be problematic after use and either banned at that point or an additional warning was issued.
One of the more disturbing trends recently in the number of benzodiazepine compounds that are involved in polypharmacy overdoses. In the most recent analysis of overdoses by the CDC - 2 of the top 10 compounds were alprazolam and diazepam - both prescription benzodiazepines. In both cases 95% of these overdoses involved concomitant drugs. In the US, 30% of fatal opioid overdoses involve benzodiazepines. Due to the current problems with analysis, it is highly likely that designer benzodiazepines involved in overdose deaths are not detected. This is a compelling reason to not use designer benzodiazepines.
Reading through some of the web sites that promote the use of these compounds, it is ironic that there are messages out that that these drugs can be used safely with adequate research by the user on the Internet. Prescription medications are understood to have qualified safety when they are approved by the FDA and prescribed by a qualified physician. There are still completely unanticipated reactions and these approved medications are not generally tested with other addictive compounds. There are reactions that can only be detected by pharmacosurveillance of a much larger database. In the case of these designer benzodiazepines, they are not approved, not prescribed, and highly potent drugs being sold by sources with no responsibility to the user.
Anyone seeking to get high in that context should be questioning the value of getting high.
George Dawson, MD, DFAPA
References:
1: Pettersson Bergstrand M, Helander A, Hansson T, Beck O. Detectability of designer benzodiazepines in CEDIA, EMIT II Plus, HEIA, and KIMS II immunochemical screening assays. Drug Test Anal. 2017 Apr;9(4):640-645. doi: 10.1002/dta.2003. Epub 2016 Jul 1. PubMed PMID: 27366870.
3: Łukasik-Głębocka M, Sommerfeld K, Teżyk A, Zielińska-Psuja B, Panieński P,Żaba C. Flubromazolam--A new life-threatening designer benzodiazepine. Clin
Toxicol (Phila). 2016;54(1):66-8. doi: 10.3109/15563650.2015.1112907. Epub 2015
Nov 20. PubMed PMID: 26585557.
4: Savoldi F, Somenzini G, Ecari U. Etizolam versus placebo in the treatment ofpanic disorder with agoraphobia: a double-blind study. Curr Med Res Opin. 1990;12(3):185-90. PubMed PMID: 2272192..
5: De Candia MP, Di Sciascio G, Durbano F, Mencacci C, Rubiera M, Aguglia E, Garavini A, Bersani G, Di Sotto A, Placidi G, Cesana BM. Effects of treatment with etizolam 0.5 mg BID on cognitive performance: a 3-week, multicenter, randomized, double-blind, placebo-controlled, two-treatment, three-period, noninferiority crossover study in patients with anxiety disorder. Clin Ther. 2009 Dec;31(12):2851-9. doi: 10.1016/j.clinthera.2009.12.010. PubMed PMID: 20110024.
4: Savoldi F, Somenzini G, Ecari U. Etizolam versus placebo in the treatment ofpanic disorder with agoraphobia: a double-blind study. Curr Med Res Opin. 1990;12(3):185-90. PubMed PMID: 2272192..
5: De Candia MP, Di Sciascio G, Durbano F, Mencacci C, Rubiera M, Aguglia E, Garavini A, Bersani G, Di Sotto A, Placidi G, Cesana BM. Effects of treatment with etizolam 0.5 mg BID on cognitive performance: a 3-week, multicenter, randomized, double-blind, placebo-controlled, two-treatment, three-period, noninferiority crossover study in patients with anxiety disorder. Clin Ther. 2009 Dec;31(12):2851-9. doi: 10.1016/j.clinthera.2009.12.010. PubMed PMID: 20110024.
Saturday, May 27, 2017
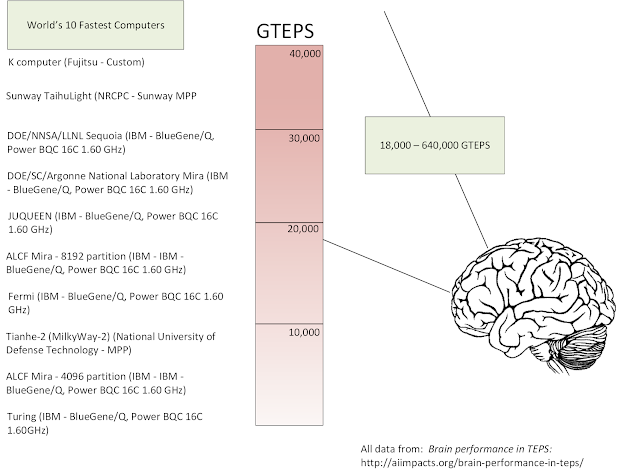
Human Brain Performance Compared To Supercomputers
For about the past year, I have been using transversed edges per second (TEPS) in my lectures about neurobiology to give a rough estimate of the computing power of the human brain and a rougher estimate of where brain power compares with artificial intelligence (AI). I finally found the detailed information on the AI Impacts web site and wanted to post it here, both for future reference and to possibly generate more interest in this topic for psychiatrists.
I have been interested in human computer comparisons since I gave a Grand Rounds on the topic back in the 1990s. Back then I was very interested in bandwidth in the human brain and trying to calculate it. My basic approach was to look at the major bus systems in the brain and their fiber counts and try to estimate how much information was passing down that bus. In engineering terms a bus is a path that the computer or processors use to communicate with other devices or processors. The rate at which that communication passes down that pathway is a major limitation in terms of computing speed to the rate at which tasks are transmitter to peripheral devices. Engineers typically specify the characteristics of these communication paths. A good example are the standard USB connectors on your computer. Today there are USB 2.0 and USB 3.0 connectors. The USB 2.0 devices can support a data transfer rate of 480 Mbps or 60 MBs. The USB 3.0 connection supports 5 gbps or 640 MBs.
In the work I was doing in the 1990s, I looked at the major structures in the brain that I considered to be bus-like the fascicles and the corpus callosum. Unfortunately there were not many fiber count estimates for these structures. It turns out that very few neuroanatomists count fibers or neurons. The ones who do are very exacting. The second issue was the information transfer rate. If fiber counts could be established was there any reliable estimate of the information contained in spikes. I was fortunate at the time that a book came out that was somewhat acclaimed at the time called Spikes. In it the authors, attempted to calculate the exact amount of information in these spikes. They used a fast Fourier transform (FFT) methodology that I was familiar with from quantitative EEG (QEEG). From available data t the time I was limited to calculating the bandwidth of the corpus callosum. I used a fiber (axon) count of 200 million. It turns out that the corpus callosum is a heterogeneous bus with about 160,000 very large fibers. Using a bit rate of 300 bits/sec for each spiking neuron multiplied by the entire bus results in a total of 60 Gbs. I had a preliminary calculation but realized I had about another 11 white matter fiber tracts connecting lobes, hemispheres and the limbic system. I did not have the fiber counts for any of these structures and the top neuroanatomist in the world could not help me.
Then I found an interesting question posted in a coffee shop. In the process of investigating it, I found some preliminary data about a group that was using a calculation called tranversed edges per second (TEPS) and showing at least on a preliminary basis that the human brain is currently calculating at a rate that is currently on par with supercomputers. I found additional papers from the group, just this week. The articles can be read and understood by anyone. They are interesting to read to look at the authors basic assumptions as well as how they might be wrong. They give rough estimates in some cases about how large the error might be if their assumptions are wrong. They provide detailed references and footnotes for their assumptions and calculations.
Their basic model assumes that the human brain is comprised of interconnected nodes in the same way that a supercomputer connects with processors or clusters of processors. This basic pattern has been described in some situations in the brain but the details are hard to find. There is also a question about the level for analysis of the nodes. For example are large structures the best choice and if not how many smaller networks and nodes are relevant for the analysis. In high performance computing (HPC) several bottlenecks are anticipated as nodes try to connect with one another including bus latency, bus length in some cases, and the smaller scale of any circuity delays on the processor. The ability to scale or divide the signal without losing the signal across several pathways is also relevant. For the purpose of their analysis, these authors use one of the estimated numbers of neurons in the brain (2 x 1011). The authors use a figure of 1.8-3.2 x 1014 synapses. Division yields synaptic connections for each neuron at 3,600-6,400.
The TEPS benchmark is discussed in detail on the Graph 500 web site under 8.2 Performance Metrics (TEPS). Reference 1 contains a more basic accessible definition as the "time required to perform a breadth first search of a large random graph requiring propagating information across every edge of the graph." The information propagation is between nodes or nodes and memory locations. The Graph 500 site also contains a listing of top performing supercomputer system and a description of their total number of processors and cores. The rankings are all in billions of TEPS or GTEPS in terms of the performance benchmark with 216 systems ranked ranging from 0.0214748 to 38621.4 GTEPS.
For the human brain calculation, the authors use the conversion of TEPS = synapse-spikes/second = number of synapses in the brain x average spikes/second in neurons = 1.8-3.2 x 1014 x 0.1-2 = 0.18 - 6.4 x 1014 TEPS or 18 - 640 trillion TEPS.
What are the implications of these calculations? If accurate, they do illustrate that human brain performance is limited by node to node communication like computers. The AI researchers are not physicians, but it it obvious that taking more nodes or buses off line will progressively impact the computational aspects of the human brain. We already know that happens at the microscopic level with progressive brain diseases and at the functional level with processes that directly affect brain metabolism but leave the neurons and synapses intact. The original research in this area with early estimates was performed by researchers interested specifically in when computers would get to the computational level of the human brain. Several of these researchers discuss the implications of this level of artificial intelligence and what it implies for the future.
For the purpose of my neurobiology lecture, my emphasis in on the fact that most people don't know that they have such a robust computational device in their head. We tend to think that a robust memory is the mark of computation performance and ignore the fact that is why humans can match patterns faster than computers and comprehend context faster than computers. We also have a green model that is more cost effective.
These are all great reasons for taking care of it.
George Dawson, MD, DFAPA
References:
1: AI Impacts: Brain performance in TEPS: http://aiimpacts.org/brain-performance-in-teps/
2: AI Impacts: Human level hardware: http://aiimpacts.org/category/ai-timelines/hardware-and-ai-timelines/human-level-hardware/
3: AI Impacts: Brain Performance in FLOPS: http://aiimpacts.org/brain-performance-in-flops/
4: Rieke F, Warland D, de Ruyter van Steveninck, Bialek W. Spikes: Exploring the neural code. The MIT Press, Cambridge, MA 1997, 395 pp.
Attribution:
Slides below are from my original 1997 presentation (scanned from Ektachrome). Click to enlarge any slide. I am currently working on a better slide to incorporate the work of the AI Impacts and Graph 500 groups on a single slide with an additional explanatory slide.
Additional reference:
My copy of Spikes:
Thoroughly Read:
Sunday, May 21, 2017
Minnesota Street Drug Bulletin - Carfentanil
 |
| Opioids morphine (upper left) and hydrocodone (lower left) and synthetic opioids fentanyl (upper right) and carfentanil (lower right) |
I don't know how widely known the issue with potent opioids on the street is - but I am concerned that the information is not getting out to the people who need to hear it. There are warnings that are read mostly by health care providers. There are politicians talking about tougher penalties and legal approaches to solving the problem. Like many people, I don't believe that the War on Drugs has been very successful. At the same time, there are not many readily available options, there is a historical precedent for control of narcotics, and we will never know what the outcome might have been without legal action against illicit drugs. I don't think that a failed War on Drugs means that there should be mass legalization of drugs. The reason is obvious. We are in the middle of an opioid epidemic that has been initiated and sustained by legal prescription opioids. This epidemic says more about the nature of addiction than legal deterrents. It is very clear that people with addictions will not hesitate to obtain what once were legally prescribed medications and use them. It is very clear that designating legal addictive drugs does not reduce the black market for highly addictive drugs or create more tax revenues for governments - both common arguments for drug legalization. All of these abstract arguments don't reflect what happens on the street.
I have personally talked with hundreds of opioid addicts over the course of my career. In the 1980s and 1990s - there was a small population of users largely due to limited access. Heroin and illicit opioid prices were relatively high and the barriers to use were also high. Widespread exposure to opioids in high school was unheard of. Most of the people I treated were part of a small, relatively fixed population of heroin users and some were on methadone maintenance. That has all drastically changed in the last 15 years.
Now it is common for me to talk with young people in their 20s who were exposed to opioids when they got opioid prescriptions for injuries that used to be treated with ibuprofen or acetaminophen. In some cases their peers in high school suggested they should try taking hydrocodone or oxycodone to get high. In many cases those drugs were scavenged from unused medications in the family medicine cabinet. Like many people in their teens and early 20s there is a cultural movement among users that they have a special body of knowledge about these drugs. That reinforces drug taking behavior and keeps them in contact with people who are actively using and supplying these drugs. In some cases it leads to mistakes in how the drugs are taken and what they are mixed with. Drug users often have illusory relationships with drug dealers that makes it seem like these dealers care more about them than their friends and family do. With continued and progressive use, opioid users might not notice how their judgment is more and more impaired - often to the point that they don't care if they die in the process of trying to get high. To be clear, these people will deny any intent to harm themselves but get to a situation where they are using a questionable amount of drugs and realize it could be a problem but at that point they no longer care. Heroin overdoses and deaths are common in small towns across America. That was unheard of in the 20th century.
Against that backdrop - carfentanil has hit the streets in Minnesota. Carfentanil is an extremely potent opioid that was never intended for therapeutic use in humans. It is a large animal veterinary tranquilizer. Its toxicity in humans is not disputed. The most significant incident was the use of a gas that probably contained carfentanil in a hostage situation at the Dubrovka theatre in Moscow. There were 40 Chechen rebels holding 912 hostages. Russian security forces pumped in a gas that killed all of the rebels and 130 hostages. The gas was described as a sleeping gas and later fentanyl. Recent research suggests that the gas was a combination of carfentanil and remifentanil. Some authors suggest that this was an anesthetic, but I have not been able to find any clinical application of this opioid in humans. Potent opioids like fentanyl are used as anesthetic agents as well as pain medications.
One of the ways that drug dealers amplify their profits is by taking a relatively inexpensive but potent product and diluting it down and selling the diluted product. I have a previous post that shows how drug dealers can take $3800 of the synthetic cannabinoid AMB-FUBINACA and produce about a half million dollars worth of product containing about 64 mg of the original compound sprayed over shredded plant material. I am not about to post how carfentanil can be diluted. There are media reports that talk about how much more potent the drug is relative to both fentanyl and morphine. Anyone trying to guess about how the raw drug can be cut is making a big mistake. The amount of drug that can lead to a lethal overdose is so small that any non-uniform distribution in a powder or tablet can result in a lethal overdose. The drug is so potent that even touching the powder can result in an overdose and health care workers have been warned not to touch the powder for that reason.
The problem is that carfentanil is being sold as a number of different products on the street. People are being given carfentanil as powders and tablets and being told that it is heroin, oxycodone, hydrocodone, and even benzodiazepines. This is an extremely dangerous practice and several Minnesotans have already died because of it.
Don't make the mistake of even trying opioids to get high. If you are currently addicted to opioids go to detox and get treatment. Don't make the mistake that you have another 5 or 10 years to get clean. If you need to take opioids, get Medication Assisted Treatment with buprenorphine or methadone, rather than continuing to use what is available on the street. With FDA approved medications used under a physician's supervision - you know exactly what you are getting. The Minnesota Department of Health recommends education in overdose prevention and naloxone administration.
I can tell you that you can't trust what you are buying on the street.
But deep down you already know that. Carfentanil is just another clear-cut example.
George Dawson, MD, DFAPA
References:
1: Influx of Fentanyl-laced Counterfeit Pills and Toxic Fentanyl-related Compounds Further Increases Risk of Fentanyl-related Overdose and Fatalities.
2: Health Advisory: Drug Overdose Deaths Linked to Carfentanil Minnesota Department of Health Mar 31, 2017 12:00 CDT
3: Carfentanil Medline references
Attribution:
All molecules at the top of this post were downloaded from PubChem and are in the public domain.
Friday, May 19, 2017
Luncheon Consensus - Management Continues To Do Nothing About Hospital Violence
I had lunch last weekend with staff from several psychiatric facilities in the Twin Cities. The group included nurses, nurse practitioners, and health unit coordinators. Many of them were at the retirement party that I described a couple of years ago. At one point in time we all worked on the same inpatient unit and that was the common bond. Over the several hour long lunch the discussion gravitated to one of our favorite topics - violence and aggression in hospitals against medical and nursing staff. There was the usual litany of injuries - concussions, a stabbing, beatings, and musculoskeletal injuries. At one point I heard how a staff nurse in her fifties with knee replacement surgery and back problems had to interject herself between a patient she was admitting and a violent and aggressive person who walked in off the street. In that situation she had to hope that security got there in time to protect her. I listened to another nurse tell me how the assault charges were determined after she was assaulted - first degree assault only because she had a concussion. The other forms of being punched and kicked that she sustained that day were all lesser forms of assault. I also heard how some members of the hospital administration minimized the incident and how her assailant eventually was not charged with anything.
This is one of many areas where the army of health care administrators really don't seem to be able to do anything productive. Every hospital in the country has posted non-discrimination policies. They discuss how every patient will be treated respectfully. These same rules do not apply to their own staff. When staff are assaulted there is a common belief that it is an occupational hazard. It is all part of the job. The other crucial part of the problem occurs at the committee level in higher levels of administration. When ever there is a potential problem resulting in injury, a standard administrative strategy is to move it to a committee or Task Force. That is where real problems occur because there is no expertise on the committee in assessing and resolving problems with violence in medical settings. That lack of expertise is common. A corollary is that administrators are in the position that they do not believe that they can defer to clinical staff with much more expertise because of the chain of command. That is a recipe for inaction and manipulation. If a staff person brings up a concern that the administrators can't solve - the issue is tabled or the person is not asked to come back. Even more problematic, some administrators embark on their own ideas about how to solve the problem. I have listed some instances of this happening on this blog that have resulted in more staff injuries. A final strategy is to bring in consultants. I have seen situations where expensive business consultants are brought in to either tell the staff that their patients are not any more aggressive than the patients seen in other hospitals in the state. If that doesn't work - bring in a consultant who will try to demonstrate that he or she knows more than the current staff. Both administrative strategies fall flat when the staff is dealing with some of the more significant problems with aggression in the state and they have the most experienced clinicians.
No - the violent outbreaks that are described in most hospitals are the result of administrative failures at several levels. A failure to recognize the issue exists. A failure to recognize that your staff has the expertise to deal with it. A failure to recognize that aggression toward the staff is not the result of staff failing to treat people in a particular way or due to a deficiency of the staff person. And most of all - a failure to facilitate a team approach among the staff in the hospital or clinic with the most expertise. It is really that easy.
In our discussion, several instances of these manipulative responses to hospital violence were noted. Even very basic requests for additional security staff and to prevent aggressive people from walking in off the street are ignored. There is no shortage of meetings and I have participated in many. One of the administrative strategies is blaming physicians for the problem. There is nothing like having a dedicated and skilled staff with as much expertise as can be found anywhere - suddenly being blamed for the problem. In some of these situations the administrators bring in "consultants" to tell senior clinics who have been treating the problem for 20 years. I am speculating that is right out of "Power Plays 101" in administrator school. It is not difficult to see how all of this administrative drama and expense fails to solve the problem. In most cases it ends up looking like nobody is even trying. A scapegoat has been found - let's leave it at that.
There has been a laudable effort by nurses. In my home state, the Minnesota Nurses Association (MNA) has been very vocal in terms of the number of aggressive incidents toward nurses in Minnesota hospitals very year. A 2004 study showed that that nurses were physically assaulted at a rate of 13.2 assaults per 100 persons per year. 17% of nurses were threatened and 34% were verbally abused in the preceding 12 months of the study. The MNA has also been active to get legislation to legally protect nurses from aggression and assault. This link to their proposal does not indicate whether either of their proposals have been successful.
It appears that there are no comparable efforts by the state psychiatric association or medical association. I am sure that if this luncheon group meets again, there will be reports of further injuries and a continued lack of response to the violence and aggression toward health care workers.
It probably makes sense in terms of the American inertia in dealing with violence and aggression in general. But it also makes sense because health care administrators really don't do anything to support clinicians or improve the environment where they work.
Replacing all of those administrators is the best place to start.
George Dawson, MD, DFAPA
References:
1: Phillips JP. Workplace Violence against Health Care Workers in the United States. N Engl J Med. 2016 Apr 28;374(17):1661-9. doi: 10.1056/NEJMra1501998. Review. PubMed PMID: 27119238.
2: Nachreiner NM, Gerberich SG, McGovern PM, Church TR, Hansen HE, Geisser MS,Ryan AD. Relation between policies and work related assault: Minnesota Nurses' Study. Occup Environ Med. 2005 Oct;62(10):675-81. PubMed PMID: 16169912; PubMed Central PMCID: PMC1740877.
3: Gerberich SG, Church TR, McGovern PM, Hansen HE, Nachreiner NM, Geisser MS,
Ryan AD, Mongin SJ, Watt GD. An epidemiological study of the magnitude and
consequences of work related violence: the Minnesota Nurses' Study. Occup Environ
Med. 2004 Jun;61(6):495-503. PubMed PMID: 15150388; PubMed Central PMCID:
PMC1763639
Supplemental:
Aggression and violence and their prevention is one of my interests on this blog. A sampling of posts can be found at this link or by selecting any of the links from the right margin.
Supplemental:
Aggression and violence and their prevention is one of my interests on this blog. A sampling of posts can be found at this link or by selecting any of the links from the right margin.
Subscribe to:
Posts (Atom)