Wednesday, January 6, 2016
Minnesota State Hospitals Need To Be Managed To Minimize Aggression
When is that going to happen? How much time will it take?
According to new Minneapolis StarTribune article by Chris Serres the situation at the state's second largest state mental hospital has worsened to the point that it has caught the attention of regulators from the Centers for Medicare and Medicaid Services (CMS). CMS put the state on notice that it at risk for losing $3.5 million in federal funding if they don't correct patient safety issues at the hospital by March 5. The hospital is described as having experienced a "surge" in violence and aggression with associated injuries since the state Legislature passed a 48 hour rule mandating that jail inmates identified in as having mental health problems be directly admitted to Anoka Regional Metro Regional Treatment Center. The jail inmates were given priority status over any civilly committed persons in community hospitals. The article points out that there have been 38 aggression-related injuries involving 24 patients in 2013 and 48 aggression-related injuries involving 28 patients in 2014. A direct assault on a staff person is described in the article.
I have a few suggestions for legislators, bureaucrats, and citizens of the State of Minnesota on how this can be resolved as soon as possible. Let me preface this by saying that I have no special knowledge about what is happening at AMRTC apart from what is in the Seres article. I am one of a handful of psychiatrists in the state who have worked in these settings and am qualified to comment on these issues. I have a formal request in to the Department of Human Services to review a copy of the CMS report because I cannot find it on the Internet, the DHS web site, the CMS web site, or the office of the Inspector General. My suggestions follow:
1. Rescind the 48 hour rule to send unscreened jail inmates to AMRTC immediately:
Any psychiatrist could have provided consultation at the time on the reasons why this will not work, but the biggest reason is that psychiatric symptoms or even a psychiatric diagnosis does not necessarily mean that a psychiatric hospital is the best place for the patient. Patients admitted to inpatient units are screened for psychiatric disorders and not on the basis of alleged criminal behavior. In terms of logistics within the state hospital system patients who are dangerously aggressive have generally been committed as mentally ill and dangerous and generally sent to the Security Hospital at St. Peter. It is fairly common to encounter sociopathic and psychopathic patients in community psychiatric hospital. It soon becomes obvious that apart from the personality disorder and the associated aggressive and inappropriate behaviors that there are no treatable problems. This patients often become aggressive toward staff or exploit other patients and are immediately discharged from inpatient settings. Inpatient psychiatric settings are not the correct place to address antisocial persons or in many cases antisocial persons even with a psychiatric diagnosis because of their danger to staff and other patients.
There is the associated issue of there being a strong incentive to send patients who may be difficult to work with but who are not psychiatrically ill to the hospital just because the rule exists. Transfers like that always occur to psychiatric units if someone has carte blanche for admitting people and psychiatrists don't screen them. Aggression can be minimized only when the entire unit is managed with a safety focus and that includes screening anyone with aggression who is admitted.
2. Reanalyze the culture at AMRTC with an emphasis on staff safety:
It is really impossible to run a psychiatric hospital if the staff responsible for the care of the patients are threatened and/or burned out. The article lead me to believe that both things are happening and compounded by the fact that hospital staff is being mandated to work extra hours. In the initial stages that may require the presence of additional security staff. I have seen similar situations where the level of antisocial and aggressive behavior on an inpatient unit became overwhelming resulting in a riot situation that required police intervention. Some attempts at splitting up large state hospitals to smaller local facilities in the state have resulted in similar incidents.
A critical element of the culture that has come to light in recent years is the fact that there appears to be a top down initiative in the management of state facilities. Aggressive behavior has been an ongoing problem at state facilities. Psychiatric input into that problem is not clear. It is clear that in at least some cases, programs were implemented by management staff who have no expertise in managing aggression and violence in inpatient settings.
Like most psychiatric problems aggression is a treatable problem, but it has to be addressed directly. It is best address in an environment that identifies it as a treatable problem immediately rather than an untreatable characteristic or one that has a root cause that must be addressed first. There is not better way to treat aggression than identifying it as a primary problem that is incompatible with a therapeutic environment.
3. Take a serious look at how inpatient psychiatric facilities are supposed to run:
State governments and managed care systems have both had deleterious effects on psychiatric care on inpatient units. These management systems have a lot in common in determining what happens on the inpatient side. The absolute worst case scenario is containment only. People are basically held usually based on the premise that they are dangerous in some way. Dangerous in this context generally means at risk for aggressive or suicidal behavior. They are discharged when that dangerousness passes either by the administration of medication, the person resolving a crisis in their life, or until they convince staff that they are no longer dangerous. This approach to inpatient care seriously dumbs down psychiatry, treats patients like widgets on an assembly line rather than individuals, and creates the illusion that anyone can do inpatient psychiatry. Dangerousness after all is not a psychiatric diagnosis. It also creates the illusion that an inpatient psychiatric unit is tantamount to incarceration or jail. It leads to a correctional atmosphere in what should be a therapeutic hospital environment. In a correctional atmosphere, the staff seem to be policing the patients rather than working with them on common goals. This attitude has also led at least one state official to suggest that psychiatrists in this environment are optional. A local mental health advocate has said the same thing. If that is true - why is it that the state of aggression in this hospital has gotten to the point that the union representative in the article is suggesting that the institution is being run by the patients?
4. Rexamine the funding and rationing of psychiatric care in Minnesota:
The article mentions a backlog of patients at AMRTC due to the fact that many of them cannot be discharged. This has been a problem in Minnesota for as long as I can remember. Patients are committed in acute care hospitals and end up waiting there too long for transfer to AMRTC. Once they get to AMRTC they meet criteria for discharge and there is nowhere for them to go, largely because they still have chronic psychiatric symptoms that are socially unacceptable or that preclude their safety in the community. Anyone who is covered by standard health insurance is no longer covered if they are committed to a state hospital. People can end up undergoing civil commitment because their insurance companies do not provide the level of care that they require in the community. The entire system of fragmented and rationed care can be viewed as a way for the government and managed care companies to minimize their funding of necessary care, especially in patients with complex problems. A basic option here is to expand care based on treatment parameters rather than rationing criteria. Develop treatment based and quality goals rather than rationing goals that provide minimal and frequently inadequate care. One of the basic principles of community psychiatry is that the funding needs to follow the patient. If patients are committed and transferred to state hospitals and they are on private insurance plans - those plans need to have continued financial responsibility for those patients. If a patient with private insurance needs treatment in jail, those services need to be covered by private insurance rather than being shifted to law enforcement. The entire system of rationing and cost shifting is also a strong incentive to transfer any mentally ill inmate to AMRTC because law enforcement is covering the cost of medical and psychiatric care.
5. Facilities for mentally ill inmates that recognizes their vulnerability:
One of the concerns that I have always had for any inmate with a mental illness, is that they are generally much more vulnerable to any form of manipulation or intimidation by career criminals and sociopaths. The second concern is that many patients with mental illnesses end up in jail because they are symptomatic and/or confused and end up trespassing or in dangerous situations. They are often not able to follow instructions by the police. Some Minnesota counties have mechanisms to safeguard this population. One of them is having them screened in jail for competency to proceed to trial by qualified psychiatrists and psychologists. The resolution in those cases is that the patient is transferred to an inpatient psychiatric unit for stabilization and the pending legal charges are usually dropped. They can frequently be discharged from the acute care hospital without transfer to a state hospital. In cases where this does not occur, every effort should be made to segregate the vulnerable inmates who are mentally ill from the general jail or prison population. The ideal situation would allow for more programming to prevent some of the common correctional problems like isolation that lead to increasing symptoms.
These are a few suggestions to resolve the current problems with aggression noted to exist at at AMRTC. Over the years that I have been following this story, there is also the question of what is really going on in these facilities? Why are these problems so difficult to resolve when acute care hospitals have fewer problems and are dealing with more acutely agitated and frequently intoxicated individuals. Why does the bureaucracy think they can resolve these problems without using psychiatric expertise or at least methods that have been proven to work in psychiatric institutions? And what about the alternate and seemingly more permissive methods of dealing with aggression? Can anyone come out with a comment on whether or not they have succeeded or failed? There is a lack of transparency when it comes to seeking the answers to these questions.
These are all important questions that need to be answered. I hope to receive the CMS report and make further comments on this situation. There is a lack of transparency about what the state is doing to resolve this situation. When the state assumes the care of mentally ill individuals - people who by definition are vulnerable adults, transparency is important to assure their adequate care and reassure the families of all of the patients admitted to this hospital.
George Dawson, MD, DFAPA
References:
1: Chris Serres. State psychiatric hospital in Anoka threatened with loss of federal funding. Minneapolis StarTribune January 4, 2016.
Attribution:
The jail photograph at the top of this blog is by Andrew Bardwell from Cleveland, Ohio, USA (Jail Cell) [CC BY-SA 2.0 (http://creativecommons.org/licenses/by-sa/2.0)], via Wikimedia Commons. The URL is: https://commons.wikimedia.org/wiki/File%3ACela.jpg
Friday, January 1, 2016
New England Journal of Medicine Discovers Assertive Community Treatment
I have been a reader and subscriber to the New England Journal of Medicine (NEJM) every year since medical school. One of the first courses they taught us in those days was Biochemistry and being an undergrad chem major I had a natural affiliation with many of the biochem professors. The format in those days was lectures focused on the major topics and seminars to take a more detailed look at the experimental and theoretical aspects of the field. They were fairly intensive discussions and critiques of research papers selected by the professors. The department head was the mastermind behind this technique and one days he discussed his rationale for it. He hoped that every medical student coming through that course would continue to read current research. He strongly recommended subscribing to and reading the NEJM not just in Medical School but for years to come. In my case it worked.
One of the sections that you don't hear too much about is the clinicopathological exercise that comes out each week. It is basically a publication of formal case records of Massachusetts General Hospital and the associated findings and discussions. These case reports are interesting for a couple of reasons - they show patterns of illness that clinicians can familiarize themselves with and they show at least some of the diagnostic thinking of experts. During the time I have been reading them, they also discuss psychiatric comorbidity of physical illness and medical etiologies of psychiatric symptoms. At one point I was a member of an informatics group and was very interested in studying this section of the NEJM from a psychiatric perspective. At that time it seemed that I was the only psychiatrist with that interest. With modern technology a study like this is more possible than ever. For example, searching the case records feature of the NEJM from December 1989 to December 2015 yields a total of 31 cases of psychosis. The etiologies of these cases range from purely medical etiologies, to delirium associated with the medical condition to pure psychiatric disorders with no specific medical etiology. I have never seen this referred to as a teaching source for psychiatric residents admitting patients to acute care hospitals or consultation liaison services, but I could see it serving that function. Instead of the usual lectures on medical psychiatry that typically contain PowerPoint slides of the "240 medical etiologies of psychosis" - a discussion of common mechanisms noted in these cases might be more instructive and be a better source for acquiring pattern matching capacity to broaden diagnostic capabilities. It also put the DSM approach to psychiatry in proper perspective. Knowing the lists and definitions of psychosis is nowhere enough to be a psychiatrist in a medical setting. A seminar including this material can make these points and teach valuable skills.
That brings me to the case this week A Homeless Woman with Headache, Hypertension, and Psychosis. Two of the authors are psychiatrists and the third is an internist. The authors describe a 40 year old homeless woman with a diagnosis of schizophrenia and severe hypertension and how they established care over a number of years using the Assertive Community Treatment (ACT) model of care. The patient's history was remarkable for a 12 year history of psychosis characterized primarily by paranoid and grandiose delusions. She was homeless sleeping in public buildings for about 4 years and that seemed to be due to the thought that she needed to stay outside to watch over people. She had a brief episode of treatment with olanzapine during a hospitalization about 5 years prior to the initiation of care by the authors, but did not follow up with the medication or outpatient treatment. She was also briefly treated with hydrochlorothiazide 4 years earlier with no follow up care or medication. She was admitted for treatment of a severe headache and a blood pressure of 212 systolic. At the time of the admission physical BP were noted to be 208/118 and 240/130 with a pulse of 95 bpm. She had bilateral pitting edema to the knees and bilateral stasis dermatitis. She had auditory hallucinations consisting of voice of God and Satan and grandiose delusions. Lab data showed a microcytic anemia. She had standard labs to rule out myocardial infarction and vitamin deficiency states. Blood pressure was acutely stabilized and she was discharged on lisinopril, thiamine, multivitamin, omeprazole, and ferrous sulfate. The final diagnoses include schizophrenia, cognitive impairment associated with schizophrenia, hypertension, and homelessness.
The authors provide a good discussion of diagnosis of primary and secondary psychotic disorders and provide some guidance on timely medical testing for metabolic, intoxicant, and neurological abnormalities. Delirium is identified as more of a medical emergency and necessitating more scrutiny. The idea that delirium can be mistaken for psychosis is a valuable point that is often missed during emergency assessment especially if the patient has a pre-existing psychiatric diagnosis on their medical record. The authors sum up screening tests that are necessary for all patient with psychosis and the tests that are reserved for specific clinical concerns like encephalitis, seizures, structural brain disease, and inflammatory conditions. They also suggest screening for treatable conditions and inflammatory conditions.
There is a good section on the follow up care that this patient received. She was seen in a clinic for the homeless, where problems were gradually noted and worked on with her full cooperation. This is not the typical approach in medicine where it is assumed that the patient will tolerate a complete history and physical exam and then cooperate with any suggested medical testing and treatment. In this case, the practical problems of foot care were addressed. She was eventually seen in 60 visits over two years. By visit 19 she described concerns about cognitive symptoms and by visit 33 she was accepting treatment for psychosis with olanzapine. She eventually allowed a more complete treatment of here associated physical symptoms including an MRI scan of the brain and treatment for migraine headaches. The authors point out that tolerating medical and psychiatric uncertainty is a critical skill in treating people who need to habituate to medical systems of care. A more direct approach is alienating. It does tend to create anxiety in physicians about what is being missed and not addressed in a timely manner. There is always a trade off in engaging people for long term care in more stable social settings and pushing to maximize diagnosis and treatment in a way that they might not be able to tolerate. The ACT model stresses the former.
There are some very relevant ACT concepts illustrated in this article. First and foremost the rate at which medical interventions are prescribed depends almost entirely on the patient's ability to accept them. This is at odds with the timeliness of medical interventions that most physicians are taught. I say "almost entirely" in this case because the authors were very fortunate that the patient cooperated with treatment of extreme hypertension. One of the common hospital consultations for psychiatric is a person with a mental illness and life-threatening illness who is not able to recognize it. Even on the subacute side of care there are many tragedies due to patient with mental illness not being able to make decisions that could have saved their life.
I think that there are also some very practical applications for psychiatry on an outpatient basis. Most patients with severe mental illnesses are never going to see a primary care provider 60 times before starting treatment. It only happens in a subsidized setting with physicians who are highly motivated to see a certain approach work. The care model described in the paper is certainly not the collaborative care model that some authors, the American Psychiatric Association (APA), and the managed care industry keeps talking about. There is also the obvious point that people don't go into primary care because they like talking with people who have severe mental illnesses. Psychiatrists need to see these people either in ACT teams or community mental health centers. It won't work in a standard managed care clinic seeing a patient who is this ill - 2- 4 times a year for 10 - 15 minutes. ACT psychiatrists need to know about primary care providers who work better with the chronically mentally ill or people with addictions and make the appropriate referrals. All psychiatrists should be focused on blood pressure measurements and work on getting reliable data. Funding for psychiatric treatment often precludes ancillary staff present in all other medical settings to make these determinations. Existing collaborative care models in primary care clinics can get blood pressure measurements on the chart but restrict patient access to psychiatrists.
This Case Report is a good example of what can happen with a real collaborative care model that focuses on the needs of a person with severe chronic mental illness. It is a model of care that I learned 30 years ago from one of the originators and it is more relevant today than ever. It is also a model of care that is currently rationed and provided in the states where it is available to a small minority of patients. It is not the method of collaborative care that you hear about from the APA, the managed care industry, or government officials. It should be widely available to all psychiatric patients with complex problems.
George Dawson, MD, DFAPA
References:
1: Shtasel DL, Freudenreich O, Baggett TP. CASE RECORDS of the MASSACHUSETTS GENERAL HOSPITAL. Case 40-2015. A 40-Year-Old Homeless Woman with Headache, Hypertension, and Psychosis. N Engl J Med. 2015 Dec 24;373(26):2563-70. doi: 10.1056/NEJMcpc1405204. PubMed PMID: 26699172.
2: New England Journal of Medicine Case Records of MGH x psychosis (on Medline). Shows 101 references as opposed to 31 on NEJM search engine and 10 on basic Medline search.
3: Marx AJ, Test MA, Stein LI. Extrohospital management of severe mental illness.Feasibility and effects of social functioning. Arch Gen Psychiatry. 1973 Oct;29(4):505-11. PubMed PMID: 4748311.
4: Stein LI, Test MA, Marx AJ. Alternative to the hospital: a controlled study.Am J Psychiatry. 1975 May;132(5):517-22. PubMed PMID: 164129.
5: Test MA, Stein LI. Alternative to mental hospital treatment. III. Social cost. Arch Gen Psychiatry. 1980 Apr;37(4):409-12. PubMed PMID: 7362426.
6: Stein LI, Test MA. Alternative to mental hospital treatment. I. Conceptualmodel, treatment program, and clinical evaluation. Arch Gen Psychiatry. 1980 Apr;37(4):392-7. PubMed PMID: 7362425.
7: Weisbrod BA, Test MA, Stein LI. Alternative to mental hospital treatment. II. Economic benefit-cost analysis. Arch Gen Psychiatry. 1980 Apr;37(4):400-5. PubMed PMID: 6767462.
Attribution:
Photo at the top of this post is by Jonathan McIntosh (Own work) [CC BY 2.5 (http://creativecommons.org/licenses/by/2.5)], via Wikimedia Commons. Original photo at https://commons.wikimedia.org/wiki/File%3ARNC_04_protest_77.jpg
Attribution:
Photo at the top of this post is by Jonathan McIntosh (Own work) [CC BY 2.5 (http://creativecommons.org/licenses/by/2.5)], via Wikimedia Commons. Original photo at https://commons.wikimedia.org/wiki/File%3ARNC_04_protest_77.jpg
Sunday, December 20, 2015
Eric Kandel Comes To Minnesota
| Eric Kandel, MD |
Nobel Laureates don't come to Minnesota very often but they apparently come at least once a year to Gustavus Adolphus College and the annual Nobel Conference. This year's conference was particularly interesting to me because it starred the only modern psychiatrist to be a Nobel Laureate - Eric Kandel. He shared the podium with his wife and research collaborator Denise Kandel. Eric Kandel is a giant in neuroscience and has continued to extend his research well into the time in life where most people have been retired for years. In my addiction lectures, I use his well known paper Psychotherapy and the Single Synapse published in 1979 and his recent work on nicotine exposure and the risk of cocaine use entitled A Molecular Basis for Nicotine as a Gateway Drug published in 2014 as lecture references. Kandel has been a neuroscientist and a psychiatrist longer than I have been a psychiatrist. The other aspect of Kandel's more accessible work is his ability to integrate basic neuroscience and cognitive neuroscience into a coherent story of possibilities. The best example is the book The Age of Insight that I briefly reviewed on this blog. It is clear from reading Kandel that he has a lot on his mind and he is actively seeking answers and organizing his observations. Another feature that piqued my interest in this case was why he was presenting at an addiction conference in a state where many people believe that addiction treatment was invented. I did not find out about the conference until it was too late to take time off of work to attend. I was very pleased to find the presentations and Q&A sessions by Eric Kandel and Denise Kandel available online. There are a total of 4 videos and they will load and play in succession. There may be more videos with the Kandels but I only watched these four.
In the first session Kandel discusses some of the early discoveries in brain systems and how the idea of localization of brain function played out. For most physicians with a passing knowledge of aphasia and strokes it is a bit tedious. Eventually he gets to a discussion of memory localization and talks about implicit and explicit memory. That allows him to look at different features, animal models and the molecular biology of these types of memory. He goes on to look at age-associated memory loss and Alzheimer's Disease and the different brain substrates and mechanisms. At that point some of his slides illustrate chromatin and transcription sites but he does not get bogged down in the details as he defers the chromatin issue to a later presentation and discusses RbAp48 as a critical transcription factor in the formation of long term memories. He showed a plausible mechanism for exercise leading to osteocalcin secretion from bones and improvement in memory as one possible humoral factor associated with vigorous exercise. In terms of style points, he had great graphics especially the diagram of the DNA strand wrapped around histone octamers and how the transcription process is affected by various molecules. He was clearly there to present a lot of information to non-molecular biologists. He was a little hurried at times. He makes a few misstatements and gets distracted like all of us do during presentations. He interjects some humor along the way. As the presentation continues it is clear that this is important information.
The Q & A session was focused primarily on the question: "Is addiction a brain disease?" The other panelists and their biographical sketches can be viewed at this page. I did not realize it until after I had viewed all of the sessions that the lectures were not a good fit in terms of answering that question. The lectures were focused on the neurobiology of learning and how epigenetic changes due to nicotine exposure lead to other addictions. They were not lectures on the neurobiology of addiction per se, but there were some partially suggested mechanisms related to Kandel's work on memory. Addiction being a brain disease was really not the point of the lectures. It was obvious that the other panelists were at the minimum resistant to the idea but there was also open opposition. If you read the biographical sketches one of the panelists has written a book on why addiction is not a disease. If they really wanted to argue that point they could have brought me down for a Neurobiology of Addiction lecture and I could have dissected the arguments about addiction being a disease or not. A much better idea would be to bring Eric Nestler in for the lecture.
The panelists seemed of the opinion that plastic changes in the brain were normal and therefore plastic changes in the brain caused by addictive compounds was not a sign of pathology. Some seemed not to be focused on the brain at all but cultural or social factors that they thought were important. In at least one case, they seemed to suggest that addiction needs to occur in a certain context - that all addictions are not created equal. The example given was a wealthy white guy with a cocaine addiction could just jet off to the Caribbean and go swimming as a way to deal with his addiction. Someone else would not have that opportunity. Kandel had a singular focus that all human behavior, that everything that we are occurs because of what is happening in the brain. He kept going back to this idea and pointed out that alterations in brain plasticity certainly occur during addiction but they are negative and not positive changes. He of course agrees that social and psychological processes are important intervening factors but all of the processing occurs at the level of the brain. Some of the panelists seemed uncomfortable with this basic idea and he got into it with one of them, but eventually summarized the problem as a lack of a common culture. He extended that comment to include the idea that the panel is discussing these problems so that younger generations in the audience will not have to start at that contentious point. To me it came back to the mismatch between the Kandels' lectures on the epidemiology and molecular biology of nicotine as a gateway drug and the other panelists arguing that addiction was not a disease.
Denise Kandel began the third session reviewing the epidemiology of when people start using addictive substances and what the relationship is to nicotine. In general, nicotine use is a strong predictor of cocaine use and ongoing cocaine use. She analyzed three databases that are essentially cross sectional surveys of substance use including the NSDUH (National Survey On Drug Use and Health), MTF (Monitoring the Future) and NESARC (The National Epidemiologic Survey on Alcohol and Related Conditions). She discussed the concept of Translational Epidemiology or making population wide observations and then looking at models to explain the observations. She had what I would call a critical observation on the observed drop in cocaine use and cocaine related mortality and cigarette use. The recent drop in cocaine related mortality seems to correlate with a decrease in smoking. Eric Kandel stepped in for the basic science section to elaborate on the mechanism of histone acetylation and how that occurs from nicotine exposure. Denise Kandel returned to talk about the problems with e-cigarettes as potentiating factors for the use of other drugs and also as probably not a good way to stop smoking. If you had time to watch one of the videos I would recommend this one.
The final Q & A session was an interesting one. One of the panelists talked about the sociological theories of drug use rather than a gateway involving a biological substance. For example, the fact that you take a substance that makes you feel good, increases the likelihood that you will take additional compounds that will do the same and that you will associate with people who have common interests and they will encourage further drug use. Kandel had three comments during this session that I thought were very interesting. The first involved the scientific rationale of a reductionist approach. When you hear it explicitly stated rather than being used in a vague and rhetorical manner - it makes a lot more sense. The second had to do with a painting by Gustav Klimt called Judith beheading Holofernes (Judith I and the head of Holofernes). He tells the story about this biblical incident and discusses how this is a painting that combines elements of aggression and sensuality and how recent work by Anderson has shown that there is a 20% overlap between areas of the brain that govern aggressive behavior and areas that govern sexuality and reproductive behavior. At one point Kandel seemed frustrated by some other panel members and made a reference to reproducibility that may have startled a few of them. Denise Kandel had previously alluded to the bias against reductionism in her discussion with the statement: "It's a reductionist approach to which some members of this audience are going to object strenuously"
The videos were very affirming for me. When I think about the lectures I give on Kandel's work and some of the posts on this blog - I am confident that I have come to the same conclusions that he comes to about the brain and about reductionism. Of course it is easier for me, because he provides the conclusions and I merely teach them. I don't think that everybody has come to those conclusions either at a scientific or philosophical level. It is too easy to get hung up on polarizing questions and political debates about science these days, especially using imprecise definitions like the word disease or claiming that reductionism is a fatal flaw rather than a good way to do science. It is too easy to mistake journalism - in many cases hatchet-job journalism - for science. The other striking factor is that this is a brain centric view of the world and that seems like the only logical approach to me. Various critics will attack the brain centric view of neuroscience or psychiatry in ways that seem to miss the point. Much of the criticism comes down to the definitions of diseases or disorders and the idea that a biomedical approach to the brain means that only biomedical treatments are possible.
I think that it might be easier to reconcile the brain centric view if the ultimate result of that view is considered and that is tremendous computational power that results in billions of people with billions of unique conscious states. That is the ultimate product of what Dr. Kandel is talking about in terms of human learning - how it affects the conscious state and the associated brain substrate. That may have something to do with biomedical treatments, but it also applies to every other intervention that can be brought to bear to facilitate recovery. To make an even more obvious argument - the cure is in your head - not out in the ether somewhere. The corollary is that it is important to know what those mechanisms are.
If you have time, watch these videos. It is a rare chance to see one of the brightest guys in psychiatry and neuroscience in action. I would also encourage reading The Age of Insight. It left me with the impression that this is a scientist at the top of his game and it is inspirational reading.
George Dawson, MD, DFAPA
References:
1: Kandel ER. Psychotherapy and the single synapse. The impact of psychiatric thought on neurobiologic research. N Engl J Med. 1979 Nov 8;301(19):1028-37.
PubMed PMID: 40128.
3: Anderson DJ. Optogenetics, sex, and violence in the brain: implications for psychiatry. Biol Psychiatry. 2012 Jun 15;71(12):1081-9. doi: 10.1016/j.biopsych.2011.11.012. Epub 2011 Dec 29. Review. PubMed PMID: 22209636.
Attribution: The picture of Eric Kandel is By Bengt Oberger (Own work) [CC BY-SA 4.0 (http://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons. The file URL is: https://upload.wikimedia.org/wikipedia/commons/c/ca/Eric_Kandel_01.JPG.
Supplementary 1: I am fully aware of the fact that Denise Kandel and the other participants in the conference were there and are all scholars. The title of this post reflects that fact that the Nobel Laureate came to the Noble Conference.
Supplementary 2: This is a blog and it should be obvious that none of the speakers, institutions, or content producers mentioned in this blog post endorse this work or even know about it. This statement is for anyone who does not think it is that obvious. I did not attend this meeting and had no input into its content.
Sunday, December 13, 2015
The Beginnings Of True Pharmacosurveillance
 |
| From: Morbidity and Mortality Weekly Report (MMWR) October 16, 2015/ 64 (9): 1-14. |
Some reviews currently happen at some level in the US. In hospitals and care systems where there is routine review of physicians, some cases are reviewed prescribing patterns are observed and they are given feedback. That process is limited by a lack of standardization and objectivity. Just a few cases may be reviewed when today's information technology (IT) capability allow for reviewing all of a physician's caseload all of the time. The review is often part of a larger process like an annual review where there may be conflicting agendas like spinning the review to make the person look as good or as bad an an administrator wants them to look. Physicians can also be contacted by managed care organization (MCOs) or pharmaceutical benefit managers (PBMs) with letters expressing various concerns. Examples might be patients who have filled only one prescription for antidepressants, patients seeing multiple prescribers, and polypharmacy. These letters are often poorly thought out, probably don't apply to the physician or patient at the time the letter is sent, and seem to be heavier on public relations than the technical details of prescribing medications. In some cases these reviews can be totally inappropriate. To cite an example, a reviewer notifies nursing staff that a patient on lithium needs follow up and immediate blood tests upon discharge because the inpatient physician has not ordered the appropriate tests when they do not have the most recent records, have not spoken to that physician, and don't know that all of the testing has been done.
Another very relevant question for pharmacosurveillance is: "Who owns the data?" Any managed care company that I am aware of treats patient data as their own proprietary data whether they know what to do with it or not. I gave the previous example on this blog of asking a managed care executive for permission to use deidentified brain images for teaching purposes and being told: "Why would we want you to use our data?" despite the defined teaching purpose of the institution and a long history in medicine of teaching all of the available abnormal findings for the purpose of developing better diagnosticians. Prescription and pharmacy data has an even more clandestine history. Most physicians were not aware until very recently that all of their prescription data was collected from pharmacies everywhere by a company called IMS America and that information was used primarily by pharmaceutical company sales forces to monitor the products being prescribed and whether their detailing people were having an impact on those prescriptions. The individual physician was not able to see these records or look at the trends in their prescribing data over time. The data collection was centralized only for the purpose of selling the collected data to pharmaceutical companies or (for the past 15 years or so) buried in clinic or hospital electronic health records. The best a physician could do would be to request prescribing data on a particular patient from their pharmacy. That might result in 20 or 30 faxed pages of lines and lines of prescriptions, usually encompassing only the most recent years.
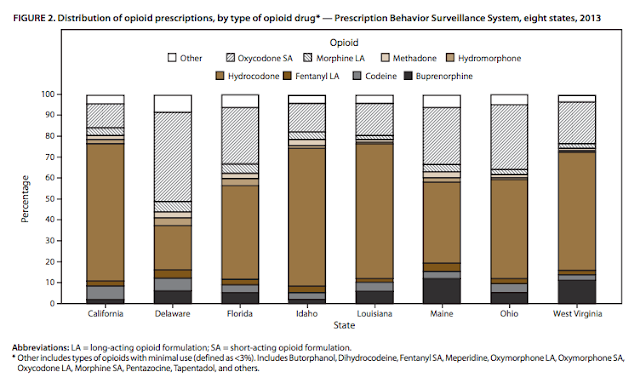
The state may not only claim the data, but set in place mandatory rules about how practitioners collect the data and transmit it to them. In the state of Minnesota, all practitioners treating depression are mandated to have their patient complete PHQ-9 rating scales for depression and have those results sent to the state. The state also monitors prescribing data on stimulant prescriptions for children and mandates that any person taking an antipsychotic medication needs to sign a written consent form. Currently 49 of 50 states participate in Prescription Drug Monitoring Programs (PDMPs) to track drugs classified on the Controlled Substances Act Schedules II - IV. The PDMP programs were originally set up to help law enforcement identify illegal activities with controlled substances but developed into a resource for physicians who wanted to know if their patient was getting multiple prescriptions or prescriptions that increased the risk of medications that they might be prescribing. These pre-existing systems led the CDC and the FDA to develop the Prescription Behavior Surveillance System (PBSS) to look at the trends in the prescriptions of controlled substances. Typically all pharmacies within a state submit data on controlled substances within a week of the prescription being filled. The PBSS categorizes all of the data into three categories: benzodiazepines, stimulants, and opioid analgesics. Buprenorphine is classified in the opioid analgesic category even though the primary use is for treating opioid dependent patients. Tramadol was not included in the database until it was reclassified in 2014. There is also a miscellaneous category that includes zolpidem and carisoprodol. I think it probably makes sense to include GABA enhancing sedative hypnotics like zolpidem, zaleplon, and eszopiclone in the benzodiazepine category.
The preliminary data from the PBSS system that was just released in October is very interesting. In terms of a representative sample, the eight states reported cover 1/4 of the US population and represent all 4 US Census Bureau Regions. Prescription rates were calculated as the prescription rate per 1,000 residents as given by the most recent Census data. Perhaps most surprising is that the rate of opioid prescribing approaches nearly one prescription for every state resident in some states in some states and the rate of opioid prescribing is twice as high as the rate of benzodiazepine or stimulant prescribing. There are two to four fold differences in state-to-state prescribing of controlled substances across the board. The top 1% of opioid prescribers in Delaware wrote for one out of four opioid prescriptions in the state. The top decile of prescribers account for 50-60% of opioid prescribing but that decile does not solely account for state-to-state differences. Specialists in pain clinics (pain medicine, surgery, physical medicine) were more likely to write more prescriptions per day but are thought to account for < 20% of all opioid prescriptions per day. The authors suggest that most of the prescriptions in that category are written by general practitioners, family medicine, internal medicine, and midlevel practitioners.
Overlapping prescriptions ( benzodiazepines and opioids and long-acting and short acting opioids) were common. Multiple provider episodes or MPEs defined as a resident filling a controlled substance prescription from 5 or more prescribers at 5 or more pharmacies in any 6 month period varied significantly by state, age, and the number of controlled substance schedules added. The totals ranged from a low of 4.4/100,000 residents in Louisiana to 66.8/100,000 in Ohio. An overall first impression of this system is that there are limitation but it clearly provides valuable information on prescribing behavior relevant to controlled substances.
The current epidemic of accidental overdose deaths was the driving force for the PBSS system. It shows that a pharmacosurveillance system is possible, but that there are some limitations. Data quality as inputted from the pharmacies needs to have quality control measures to assure consistency. An ideal system would also include a diagnosis or indication. Physician speciality would also be a useful marker. I think that the best use of a system like this would be to allow physicians to mine their own prescription data and see how they compare with other physicians in general and within their own speciality. Specific strategies could be developed for self correction at the earliest possible stages. I wrote about a pharmacosurveillance system used in Wales in a previous post. The top 5 drugs causing complications in that system were opioids, antibiotics, warfarin, heparin, and insulin - in that order. With a sophisticated system it would be possible to pick up significant adverse drug events and monitor those events as well.
All of the talk about patient safety these days is really about patient safety being practiced in the silos: health care businesses, hospitals, and clinics. Places where individual health care data is considered proprietary - at least until there is a complication big enough that the state authorities mandate that it be reported for investigation. These businesses have an inherent conflict of interest in reporting adverse drugs events and severe complications. Pharmacosurveillance should be out there across the entire health care landscape. It should not depend on reports about complications made by businesses that are in effect protected by patient privacy. Complications can be actively sought out and investigated any time a prescription suddenly stops or changes. This data also needs to be freely available to physicians so that they can look at their prescribing data relative to their peers and make changes where necessary.
It is time to view the process as as a way to learn about how to provide the safest possible environment for patient care, rather than a way to "catch" somebody when something goes wrong.
George Dawson, MD, DFAPA
References:
1: Paulozzi LJ, Mack, KA, Hockenberry JM. Vital Signs: Variation Among States in Prescribing of Opioid Pain Relievers and Benzodiazepines — United States. Morbidity and Mortality Weekly Report (MMWR) July 4, 2014 / 63(26): 563-568.
2: Paulozzi LJ, Strickler GK, Kreiner PW, Koris CM. Controlled Substance Prescribing Patterns —
Prescription Behavior Surveillance System, Eight States, 2013. Morbidity and Mortality Weekly Report (MMWR) October 16, 2015/ 64 (9): 1-14.
 |
| From Morbidity and Mortality Weekly Report (MMWR) October 16, 2015/ 64 (9): 1-14. |
Saturday, December 12, 2015
Medical Marijuana For Intractable Pain - The Minnesota Update
Minnesota made headlines at least within the state lately by qualifying intractable pain (typically known as chronic noncancer pain) as a condition for Minnesota's Medical Cannabis program. I find it politically interesting that when you want to take over medical systems of care the strategy is to eliminate the word medical wherever that is possible. But in this case when there is limited if any medical evidence for a treatment that carries significant risks and the initiative seems like part of a political movement toward the general legalization of marijuana that the word medical is added to seemingly legitimize the entire process. I don't think that there is anything medical about marijuana or cannabis. If you want it legalized, make that argument and don't pretend that a compound (or more appropriately compounds) that has been around for 5,000 years has suddenly become a miracle drug.
I previously posted about the original statute and will not repeat any of that in this post. The full details of the intractable pain indication are listed on a separate DHS web site including the definition of intractable pain. The statutory definition of intractable pain is quite complicated and seems to misunderstand the nature of chronic pain, ignore the addiction cofounder, and address the non-cannabis treatment of chronic pain with Schedule II to V drugs and issue that seems totally unrelated to cannabis use. To cite a couple of examples:
"§ Subdivision 1.Definition. For purposes of this section, "intractable pain"means a pain state in which the cause of the pain cannot be removed or otherwise treated with the consent of the patient and in which, in the generally accepted course of medical practice, no relief or cure of the cause of the pain is possible, or none has been found after reasonable efforts. Reasonable efforts for relieving or curing the cause of the pain may be determined on the basis of, but are not limited to, the following:
(1) when treating a nonterminally ill patient for intractable pain, evaluation by the attending physician and one or more physicians specializing in pain medicine or the treatment of the area, system, or organ of the body perceived as the source of the pain; or...." With chronic noncancer pain is is generally accepted that there is no medical treatment that will eliminate the pain. There is no medication that will totally alleviate the pain. That includes high potency opiate medications. Most of the literature suggests that whether high potency opiates, anticonvulsants, ar antidepressants are used the result is a moderate amount of pain relief at best and additional measures like physical therapy and psychotherapy are needed to produce optimal results. There is really minimal to no evidence that the addition of cannabis to existing pain medications will add anything. In this case, the statute also suggests that all of these pain patients will be referred to "one or more physicians specializing in pain medicine" or the part of the body that the pain is associated with. This statute seems like it could easily set-up a physician or group of physicians who could add cannabis to the medications that they are already prescribing. In other words the statute is providing a non-medical indication that can be used to alter medical practice on a large scale by the prescription of an addicting drug. We have seen previous epidemics of use and overprescribing based on similar theories.
Subd 2. from the same statute gets in to existing medical practice for reasons that are not apparent to me. It includes the following introductory paragraph and goes on to cite the non-applicability of the statute to the issue of treating substance use disorders, use for non-therapeutic purposes, providing a scheduled drug for the purpose of terminating life in a person with intractable pain, and using a non-approved drug. Based on my experience Schedule II-V drugs are widely used for non-therapeutic purposes if use for any indication outside of analgesia is considered a non-therapeutic purpose. A few examples include taking extra medication for insomnia, anxiety, depression as well as mixing the medication with alcohol for an added effect. It seems more than a little naive to me to think that a controlled substance with broad effects on the conscious state that potentially reinforces its own use will be not be used for other purposes. That includes the use of cannabis and marijuana.
"§ Subd. 2.Prescription and administration of controlled substances for intractable pain. Notwithstanding any other provision of this chapter, a physician may prescribe or administer a controlled substance in Schedules II to V of section 152.02 to an individual in the course of the physician's treatment of the individual for a diagnosed condition causing intractable pain. No physician shall be subject to disciplinary action by the Board of Medical Practice for appropriately prescribing or administering a controlled substance in Schedules II to V of section 152.02 in the course of treatment of an individual for intractable pain, provided the physician keeps accurate records of the purpose, use, prescription, and disposal of controlled substances, writes accurate prescriptions, and prescribes medications in conformance with chapter 147."
There is some science added to the Intractable Pain page in the form of a review entitled: Medical Cannabis For Non-Cancer Pain-A Systematic Review. It was prepared in the standard manner of most current literature reviews critiquing the quality of the studies and looking at what the evidence shows. Most people who are uninterested in the details of these reviews could benefit from reading the executive summary. Like most of these systematic reviews the authors conclude that the overall evidence is sketchy, that a few studies established a response better than placebo, that the clinical trials are of short duration and patient selection is not likely to reflect who might use the drug in Minnesota, and that most of the trials looked at adjunctive treatment of cannabis and limited forms rather than cannabis monotherapy. They also conclude that cannabinoids were associated greater risk of any adverse events, serious adverse events, and events associated with withdrawal from the study than placebo. The authors were aware of a recent review in JAMA provided an interesting analysis of that data in the context of their review on pages 22 and 23. The authors point out that their review (unlike the JAMA review) did not use data from unpublished studies in the meta-analysis of treatment effects. Their re-analysis of the JAMA review data generally shows either evidence that does not show superiority over placebo or in the case where it does - the evidence is of low or insufficient strength.
I am not going to include an exhaustive review of the toxicity of cannabis or the developmental concerns of cannabis exposure in utero or in the developing adolescent brain. I am considering a separate post on that topic. For the purposes of an intractable pain post, I will add a couple points about politics and regulation. The first point is that chronic pain is a complex disorder. It resembles what is commonly conceptualized as a psychiatric disorder much closer than what is considered a standard medical or surgical disorder. Chronic pain is multidimensional and is frequently associated with depression, anxiety, and insomnia. Pain ratings on any given day can reflect the state of those other conditions. Cannabis can affect all of those other conditions in unpredictable ways. The best example I can think of is the chronic marijuana smoker who starts in order to treat anxiety and stops years later because the anxiety is worse and he is now experiencing panic attacks or paranoia. Anything that complicates the other dimensions of chronic pain will not be an acceptable overall treatment. The second point is that some chronic pain patients end up taking a drug in an addictive manner independent of pain relief. That is true for marijuana, opioids, and benzodiazepines. Many patients will openly admit that they are using the drug because they like the effects, but it is not doing a thing for their pain. The final point is that some people do not discriminate between numbness and analgesia. The drug they take for pain has to induce a numb state - one where they generally have a difficult time functioning. I include these points about chronic pain trials because these additional phenomena are usually not examined in the clinical trials. The trial occurs as if every subject can rate their pain like they can take a blood pressure reading and that loses a lot of important information in the process. The studies in the reviews listed here for cannabis in non-cancer pain can show weak positive effects and those kinds of studies will eventually be approved by the FDA as evidenced by some FDA actions where the regulatory considerations trump the scientific ones. With marijuana being described as a fast growing $3 billion dollar a year business with a projected maximum market of $36.8 billion annually, you can bet there will be a large commercial lobby pushing for approval of whatever products they want to bring to market.
I don't plan on getting too riled up about the Minnesota experiment and the political indications for "medical" marijuana. It is clearly a response to the current cultural swing to view cannabis as a benign product and use the medical avenue to get total legalization. When marijuana use gets as widespread as alcohol use, the population toxicity will be more evident. In the meantime, I hope physicians don't get pulled into the politics - especially psychiatrists.
I don't plan on registering on the Medical Cannabis Registry and certifying patients for the political indications for its use. I consider that to be a foolish endeavor. It would be much easier to take physicians out of the loop instead of having them pretend to select patients for a drug with no medical indications. If anything, the widespread use of marijuana or cannabis for whatever the reason will complicate psychiatric practice and increase the costs of treatment that is already rationed by healthcare businesses and the government.
George Dawson, MD, DFAPA
Refs:
1: Butler M, Krebs E, Sunderlin B, Kane RL. Medical Cannabis for Non-Cancer Pain: A Systematic Review. Prepared for: Office of Medical Cannabis Minnesota Department of Health, October 2015.
2: Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for Medical Use: A Systematic Review and Meta-analysis. JAMA.2015;313(24):2456-2473. doi:10.1001/jama.2015.6358.
Attribution:
Jennifer Martin (Own work) [CC BY-SA 4.0 (http://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons at: https://commons.wikimedia.org/wiki/File%3AMarijuana_Plant_01.JPG
I don't plan on getting too riled up about the Minnesota experiment and the political indications for "medical" marijuana. It is clearly a response to the current cultural swing to view cannabis as a benign product and use the medical avenue to get total legalization. When marijuana use gets as widespread as alcohol use, the population toxicity will be more evident. In the meantime, I hope physicians don't get pulled into the politics - especially psychiatrists.
I don't plan on registering on the Medical Cannabis Registry and certifying patients for the political indications for its use. I consider that to be a foolish endeavor. It would be much easier to take physicians out of the loop instead of having them pretend to select patients for a drug with no medical indications. If anything, the widespread use of marijuana or cannabis for whatever the reason will complicate psychiatric practice and increase the costs of treatment that is already rationed by healthcare businesses and the government.
George Dawson, MD, DFAPA
Refs:
1: Butler M, Krebs E, Sunderlin B, Kane RL. Medical Cannabis for Non-Cancer Pain: A Systematic Review. Prepared for: Office of Medical Cannabis Minnesota Department of Health, October 2015.
2: Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for Medical Use: A Systematic Review and Meta-analysis. JAMA.2015;313(24):2456-2473. doi:10.1001/jama.2015.6358.
Attribution:
Jennifer Martin (Own work) [CC BY-SA 4.0 (http://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons at: https://commons.wikimedia.org/wiki/File%3AMarijuana_Plant_01.JPG
Friday, December 11, 2015
Does Identifying Bipolar I Disorder Come Down To 6 Proteins?
The Mayo Clinic puts on very good conferences in Psychiatry. Two of the last three that I have attended had a strong biological and genetic emphasis. I was interested when I saw a reference in my Facebook feed to a study of potential biological markers of Bipolar I Disorder. It was even better that the article was published in the open access journal Translational Psychiatry. In the current article the authors looks at the results from the analysis of serum protein levels in controls and adults seeking treatment for depression and bipolar disorder. The sera of their subjects and controls was analyzed by Myriad RBM in a quantitative immunoassay designed to search for biomarkers through large numbers of proteins. The actual product and the proteins analyzed are described on the company's web page. All of the six proteins identified as possibly being discriminating as listed in the above graphic including growth differentiation factor 15 (GDF-15), hemopexin (HPX), hepsin (HPN), matrix metalloproteinase-7 (MMP-7), retinol-binding protein 4 (RBP-4), and transthyretin (TTR) can be located on this page and additional information is provided about the specific proteins
The authors emphasize in several places that this is a pilot or exploratory study but also point out that sufficient power to detect odds ratios for pairwise comparisons between mood disorders versus controls, bipolar disorder versus controls, and bipolar I versus controls. They looked at 272 proteins from 288 samples (141 controls, 52 Unipolar depression, 49 Bipolar II, and 46 Bipolar I). It was a one time cross sectional sample and no longitudinal sampling was done. Rigorous patient selection was used to reduce the risk of substance abuse disorders and inflammatory conditions. In a table describing patient characteristics, the cases had significantly greater BMI, greater lifetime illicit drug use, greater BMI, greater percentage of smokers, and fewer years of education. Existing symptoms were rated with the following scales IDS-C (depression), PHQ-9 (depression), GAD-7 (anxiety), YMRS (mania), and AUDIT (alcohol use). The cases were also being actively treated with antipsychotics, AED mood stabilizers, lithium, antidepressants, sedative/hypnotics, and thyroxine supplement.
The graphic from the article labelled figure 2 above shows the differences in protein concentrations for the six proteins that were significantly different after Bonferroni correction by diagnosis. As can be seen from the figure all six proteins were at the highest levels in Bipolar I disorder. ROC curves and the ROC-AUC was used to determine which proteins were better predictors of Bipolar I Disorder. The text contains theoretical and speculative discussions of these particular proteins, what they have been associated with so far, and what importance that has for the issue of why their concentrations may vary in bipolar disorder.
There are a number of relevant considerations when looking at this type of proteomic analysis. The most obvious is the assumption that the underlying dynamics of the biological substrate can be measured in meaningful ways by knowing the protein signature of those systems. Although most of us are used to looking at cartoon depictions of neuron and synapses but the reality is much more complex. Recent work in Science shows that there are 62 proteins associated with synaptic bouton (2) and vesicle trafficking and that the copy number of these proteins varies greatly. The authors of that paper speculate that the production and number of those proteins may vary because some physical locations within the neuron may allow for an enrichment effect. One of the implicit assumptions in the Frye, et al paper is that psychiatric disorders may have a unique configuration in terms of synaptic architecture and that it will be reflected in the proteins responsible for that architecture. A further assumption is these CNS protein changes are all going to be reflected in the periphery and detectable in blood samples.
Although it is premature to draw many conclusions about the data in this study, the implications may be far reaching. It will be an interesting day in psychiatry if and when proteins will be used as biomarkers. It will be an interesting day even if variants can be found and reliably detected. Until then students of neuroscience and psychiatry will be able to appreciate that information flow in these systems is significant and we are just on the cusp of being able to understand it. We are just at the stage of moving from cartoon versions of neurons - to the real thing.
George Dawson, MD, DFAPA
References:
1: Frye MA, Nassan M, Jenkins GD, Kung S, Veldic M, Palmer BA, Feeder SE, Tye SJ, Choi DS, Biernacka JM. Feasibility of investigating differential proteomic expression in depression: implications for biomarker development in mood disorders. Transl Psychiatry. 2015 Dec 8;5:e689. doi: 10.1038/tp.2015.185. PubMed PMID: 26645624.
2: Wilhelm BG, Mandad S, Truckenbrodt S, Kröhnert K, Schäfer C, Rammner B, Koo SJ, Claßen GA, Krauss M, Haucke V, Urlaub H, Rizzoli SO. Composition of isolated synaptic boutons reveals the amounts of vesicle trafficking proteins. Science. 2014 May 30;344(6187):1023-8. doi: 10.1126/science.1252884. PubMed PMID: 24876496.
Attribution:
The figure at the top of this post is from the above reference 1 and is used per the conditions of a Creative Commons Attribution 4.0 International License.
Attribution:
The figure at the top of this post is from the above reference 1 and is used per the conditions of a Creative Commons Attribution 4.0 International License.
Sunday, December 6, 2015
Better Living Through Pharmacology
One of the great unspoken biases in psychopharmacology is the belief system about the medication. What is the medication supposed to do after all? Is it supposed to be life-changing in terms of positive improvements? Is it supposed to eradicate all types of depression and anxiety? Is it supposed to create the perfect cognitive and emotional state? Is it supposed to turn an average student into an MIT professor? Is it just supposed to treat a symptom and if so - how many symptoms? Does it need to address some underlying physiological disturbance or can anyone take it and get the same benefits? These are all unspoken biases about psychiatric medications that need to be explored with people who are taking the medications. I don't think that a psychiatrist should even take for granted that a patient knows the difference between depression or anxiety or why thinking that Attention Deficit Hyperactivity Disorder (ADHD) with essentially no impairment in professional, academic, or social life is not the same as having that diagnosis.
One of the best examples is the myth of the perfect mind. If ADHD is finally diagnosed and treated, that means the person's mental functioning will either be normalized or be much better than it was in the past. It should be possible to read entire book chapters and even books for the first time. That is true isn't it? It turns out that the effects of most medications for ADHD are modest and rarely life changing. I have talked with many people who had clear diagnoses of ADHD as children who did not like the side effects of the medication and stopped taking it or even faked taking it in school. They developed strategies for coping in the world and were able to achieve academic and vocational success. Even some of the strongest proponents of medical treatment of ADHD will agree that proper care also involves lifestyle and management strategies and in some cases formal therapies in addition to medication. That does not mean that some people will not do better with medications and worse with lifestyle modification, but it does mean that there is much more latitude in the treatment of this disorder than is commonly assumed. It is fair to say that in many clinics these days, there are clinicians actively looking fro any treatable psychiatric disorder. The theory seems to be: "If I treat the social anxiety disorder, bipolar disorder, ADHD, panic attacks, and insomnia this person will be a lot better off." There is really no evidence that this is true or that there is even a good way to select what disorders should be treated first.
The patient side of this problem seems to be the myth of the perfect mind extended to many conditions. It is evident in a number of ways. Some people present with some very basic knowledge of psychopharmacology. They may suggest that their "serotonin" or "dopamine" is out of whack and that they heard that there are specific medications to correct that. In some cases they will suggest a medication. In other cases, a person will not be very stress tolerant and suggest that they need something that will either reduce day to day stress or significant stress from predictable major life stressors like the disruption of a job or relationship. They seem to think that there is a medication that will both reduce the emotional reaction to this pain but also remove the cognitive elements from their mental life. Depending on the person's baseline cognitive state, they can become quite demanding if they think that they are not getting adequate relief or it is not happening fast enough. The risk in these situations is starting to take a number of medications with substantial side effects that frequently precludes them getting back to their baseline conscious state. There is often a focus on a person's baseline in psychiatry or medicine, but that baseline is almost never adequately characterized. That is true in the case of blood pressure but more true in the case of mental illnesses. In the case of severe mental illnesses like bipolar disorder baseline is almost always defined in terms of the presence or absence of a few symptoms. Wide areas of a person's life like their baseline intellectual functioning, social behavior, and typical stream of consciousness are rarely considered - even in research studies.
Addiction makes everything worse and therefore it also provides the best illustration. The graphs at the top of the page show two drug response curves with the blue lines showing a good response. A person who is using an addictive drug and the high risk response to that drug is conditioned to expect the drug response curve on the right - a continued therapeutic response for increasing doses of the medication. In that case there is no element of safety or toxicity. True drug responses are represented by the curve on the left - an interval of response followed by toxicity and limited response at the higher levels. Addictions have a second effect by creating a bias that mental states can be fine tuned within the space of hours by drugs. Any feeling state can be immediately modified by the addition of benzodiazepines, stimulants, opioids or alcohol. This is often erroneously referred to as "self-medication" and it is a strong conditioned response that generalizes to the treatment of disorders with non-addicting drugs.
The psychological effects of these patterns are significant. They can lead to continued addiction and disrupted care. A person may have the belief: "If this doctor can't give me something that will get rid of the negative way I feel right now - I will take something to get rid of it." It may lead to disruption of the therapeutic alliance, through anger and open criticism about the lack of immediate effects or minimization of physician concern about side effects and a general lack of concern about toxicity on the part of the patient. There is often an associated belief: "I have a very high tolerance for drugs and you can give me higher starting doses and higher maintenance doses of drugs than you give most people." Many people in this situation experience very high levels of anxiety if they are not getting high doses or the physician does not seem to be increasing the medication fast enough.
The thoughts and feelings about medications is one of the most difficult areas in psychiatry. Contrary to what is written by critics - nobody is complaining about being overmedicated. Most of the complaints I hear about are about not getting enough medication and not getting to those high doses fast enough. The solution is rarely to provide the medication and amount requested. The solution is to spend enough time talking with the patient about these issues. I generally start with the limitations of the defined treatment and a medication strategy that is risk avoidant. In that initial conversation I usually tell the person whether or not they have a diagnosis or if I agree with a pre-existing diagnosis. If I detect signs that unrealistic expectations about the medication are present I move into that area, point out that the medication will not lead to a perfect mind, and what they have to do in addition to taking medication. If I find that they are really focused on medication issues to the point that they are experiencing anxiety from it - I usually encourage them to think about something else and provide some examples of what else can be done.
There is some literature on psychodynamic issues and medication in the transference that I have not found very useful. I suppose you could say that from what I have written the medication has meaning far beyond its pharmacology. There is an interpersonal and intrapsychic context. I think it is addressable in what is usually considered straightforward supportive psychotherapy, but it definitely needs to be addressed. It is a frequent cause of medication or treatment "failures".
George Dawson, MD, DFAPA
Subscribe to:
Posts (Atom)




