I thought I would add a
few facts to the speculation about what is really known about the epidemiology and toxicology involved in aircraft assisted suicides. It turns out that there are
substantial studies that have been written.
If you are a bottom-line kind of person and want to avoid further reading, I can tell you that the events are rare especially events involving commercial aircraft where the incident is ruled a suicide by aviation authorities. The events are so rare that prediction is
doubtful. In many cases the descriptions
of suicidal statements and behavior occur on the day of the events and there
are further extenuating circumstances like the use of alcohol and other intoxicants.
If you are really interested in these events, there are numerous places
where you can see the analysis of what happened and what the ruling was by the National
Transportation Safety Board (NTSB).
The media reaction is
similar to what is seen following mass shootings in the United States. After the initial shock, there is typically a
period of speculation about the causes of the disaster of the form: “What motivates
a person to do something like this?”
There is the invariable dissection of their life in the media. Were they bullied? What was their personality like? What was on
their computer? Were there any clues
that were missed that suggested that one day they would start shooting people? Were psychiatrists involved? How did they get the firearms? When all of those familiar touchstones are
exhausted (and it does not take long), the analysis starts to take on the
characteristics of groups with agendas.
Gun advocates will suggest that this person was not a typical gun owner
and therefore tighter gun laws are not needed.
Gun control advocates will provide the counter arguments that usually
involve how easy it was for this person to get a gun. There is a political impasse largely due to
the power of the gun lobby and some politicians start to talk about “being in
the wrong place at the wrong time.”
Mental health advocates, especially anyone who wants to talk about the
real problems of mental illness and violence are as disenfranchised as the gun
control advocates. Nothing ever happens. The screening advocates step up and suggest
that many of these incidents could be prevented if we just “screened” enough
people. Anyone familiar with Bayesian
statistics knows why that won’t work and may cause more harm than good.
After that impasse, a
second wave of speculation starts driven largely by people who ascribe to the
theory that psychiatric medications and psychiatric treatment can cause
homicidal behavior. There are a couple
of schools of thought on that one. The
first has to do with medications and the idea that specific medications like
SSRIs can lead to homicidal behavior.
The other has to do with the fact that seeing a psychiatrist is
associated with homicidal behavior and therefore psychiatric treatment must at
some level cause homicidal behavior or at the very least the psychiatrist is
responsible for not stopping it. As I
explored in a previous posts – there is not a shred of evidence that any of
that is true. There is however more
evidence about pilot safety, pilot use of antidepressants, and incidents ruled
pilot suicide than I have seen discussed in the media. Here are a few bits of solid data to ponder
during the expected swell of speculation about causes, who is to blame, and
possible solutions.
1.
The denominator is huge:
When the FAA or NTSB looks at all certified pilots
in the US that includes a total of roughly 620,000 people per year including
classifications for student, recreational, sport, private and commercial. Roughly 1/3 of the FAA certified pilots are
classified as commercial. The US government also collects detailed statistics on the total number of passengers flown per year (815.3 million), the total number of flights per year (9.821 million) and a host of associated statistics on the Bureau of Transportation Statistics web site.
2.
The numerator is very small:
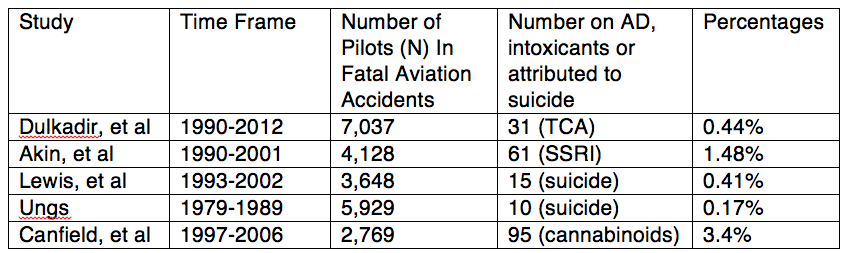
A quick glance at the table below on either
antidepressant use by pilots or the total incidents rules as suicide shows that
a small proportion of the total deaths are associated with either suicide or
antidepressant use. The proportions of
the total pilots in the data base is much smaller and the rates of both suicide
and antidepressant use are much lower than expected on a population wide
basis. Data from the Aviation Safety Network suggests that there were 8 to 10 incidents involving commercial aircraft and pilots since 1976 or about 9 in the last 40 years.
3.
The data on pilot use of antidepressants in fatal crashes:
Until
about 2006, the FAA prohibited the use of antidepressants by commercial
pilots. They have since modified their
stance to allow for specific antidepressants.
The European Aviation Safety Administration has publicly posted
information of the safety of pilots and necessary screening for psychiatric
disorders as well as prohibitions on certain diagnoses. There have been studies that look at positive
toxicology for antidepressants in the cases of fatally injured pilots. These studies have looked for the presence of
tricyclic antidepressants (TCAs) and selective serotonin reuptake inhibitors
(SSRIs) in in fatal crashes. Tricyclic
antidepressants were the predominant antidepressants prescribed before the
approval and release of fluoxetine in 1987.
One study by Dulkadir, et al looked at fatal crashes between 1990 and
2012. In this study the researchers
received biological samples from 7,037 fatally injured pilots out of a total of
8,429 fatal accidents. 2,664 were
positive for drugs on toxicological analysis.
Of those positive samples TCAs were found in 31 samples, TCAs alone in 9
and TCAs with other drugs in 22. None of
the pilots involved reported TCA use during their aviation medical exam. The authors point out that at the time
covered in this study that TCAs were not approved for pilot use and that
selective serotonin reuptake inhibitor antidepressants or SSRIs were approved
on a case by case basis. That is a
prevalence of TCA use in this database is less than 0.5% ( 31/7,037
aviators). That number is much lower
than estimates of population wide use of antidepressants.
Where the blood levels
were determined they clearly indicate that some overdoses had occurred (see
Table II and III). Blood concentrations
greater that 1,000 ng/ml are usually very consistent with overdoses and that is
the case with nortriptyline and imipramine/desipramine in these tables. The authors were able to determine that the
TCAs were prescribed for depression in three cases, pain in two cases, and
chronic insomnia in one case. Other
antidepressants were listed along with opioids, anticonvulsants, cold
medications, antihypertensives, benzodiazepines, muscle relaxants, diabetes
medications and ethanol were detected but the epidemiology was not reported. In both the studies by Akin and Dulkadir
“drugs and alcohol and/or a medical condition” was given as “a probable cause
or contributing factor in about 1/3 of the accidents where antidepressants were
detected.
There was an earlier
study of the epidemiology of SSRIs in pilot fatalities from 1990-2001 (Akin, et
al) that showed they were involved in 61/4,128 pilot fatalities or a total of
1.48%.
The available data
suggests that pilot suicide by aircraft is very rare and much lower than the
pilot suicide rate by all methods. There
is also a suggestion that the suicide rate in pilots has actually decreased. Searching the NTSB database yielded 74 fatal accidents using the search term "suicide" dating back to 1966.
Explanations given in
the article for the fewer pilots taking TCAs was that they are more toxic and
less preferred agents. Certainly in the
1990s SSRIs were heavily promoted along with the medical treatment of
depression.
4. Intoxicants are found in toxicology specimens –
The study by Canfield,
et al identified a greater percentage of specimens that were positive for
cannabinoids (relative to antidepressants) and additional performance impairing
drugs in 38% of the individuals who tested positive to cannabinoids. They also looked at the mean THC
concentration in the blood and concluded that during 1997-2001 it was 2.7 ng/ml
and for 2002-2006 it was 7.2 ng/ml. The
rate of increase in THC levels over those years exceeded the increase in cannabis
potency as reported by the National Institute of Drug Use (NIDA) over the same
years (2.7 fold as opposed to 1.5 fold).
Some authors have concluded that THC levels between 2 and 5 ng/ml
represent the lower and upper ranges of significant impairment from cannabis
use on performance tests measuring driving skill (see Ramaekers, et al) in recreational cannabis users.
The study by Bills, et al looked at the toxicology in a cohort of 36 pilots who committed suicide by aircraft during a 21 year period from 1983 and 2003. Each suicide case was matched against 2 randomly selected control accidents. In this study, the pilot characteristics included positive toxicology for alcohol, prescription drugs, and illegal drugs in 24.3%, 21.6%, and 13.5% of cases respectively. An exhaustive list of drugs found was not available in the paper. The authors were also not able to compare the toxicology of the cases to controls because 84% of the controls survived and their toxicology was unknown.
5. The baseline rate of pilot suicide is low or is it? -
Bialik looked at the issue of workplace suicide, the data quality estimates for pilots in the US. One of the key references was a paper by Tiesman, et al that looked at the issue of workers who suicide in the workplace. It used databases from the CDC (National Occupational Mortality Surveillance (NOMS)) and Bureau of Labor Statistics (Census of Fatal Occupational Injury (CFOI)). The NOMS database has no granularity and does given intentional self harm as a search parameter. Unfortunately only "transportation occupations" can be searched grouped by age, race, and sex. I did not find the number of deaths or the PMR (Proportionate Mortality Ratio) to be useful. The NOMS did have granularity with specific occupations and there was a homicide definition but none for suicide or intentional self harm. Bialik concludes that pilots in general may have a slightly higher rate of suicide than the population in general but there are problems with that estimate and he was able to consult with an epidemiologist from the CDC.
Another approach to looking at this issue to to find a study with a very well characterized database that looks at the occupational issue. Roberts, et al meets that criterion in a 2013 study of high-risk occupations for suicide. The researchers looked at the numbers of suicides and numbers in all occupations in England and Wales for specific time intervals. They determined the 30 occupations with the highest suicide rates (generally greater than 20/100,000). In comparing the time intervals (1979–80, 1982–83) to (2001–2005) they determined shift in the ranking and discussed possible causes of those changes. Pilots were not listed in the top 30 occupations by suicide rate. The only transportation workers listed were "rail transport operating staff". They noted that suicide rates for professional occupations decreased over the time interval studied while there were sharp increases in the suicide rates for manual occupations. As a comparison the 2013 suicide rate in the US was 12.6 per 100,000.
6. The accident rate due to suicide attempts in commercial aviation is lower than that found in general aviation - The study by Bills, et al looked at the toxicology in a cohort of 36 pilots who committed suicide by aircraft during a 21 year period from 1983 and 2003. Each suicide case was matched against 2 randomly selected control accidents. In this study, the pilot characteristics included positive toxicology for alcohol, prescription drugs, and illegal drugs in 24.3%, 21.6%, and 13.5% of cases respectively. An exhaustive list of drugs found was not available in the paper. The authors were also not able to compare the toxicology of the cases to controls because 84% of the controls survived and their toxicology was unknown.
5. The baseline rate of pilot suicide is low or is it? -
Bialik looked at the issue of workplace suicide, the data quality estimates for pilots in the US. One of the key references was a paper by Tiesman, et al that looked at the issue of workers who suicide in the workplace. It used databases from the CDC (National Occupational Mortality Surveillance (NOMS)) and Bureau of Labor Statistics (Census of Fatal Occupational Injury (CFOI)). The NOMS database has no granularity and does given intentional self harm as a search parameter. Unfortunately only "transportation occupations" can be searched grouped by age, race, and sex. I did not find the number of deaths or the PMR (Proportionate Mortality Ratio) to be useful. The NOMS did have granularity with specific occupations and there was a homicide definition but none for suicide or intentional self harm. Bialik concludes that pilots in general may have a slightly higher rate of suicide than the population in general but there are problems with that estimate and he was able to consult with an epidemiologist from the CDC.
Another approach to looking at this issue to to find a study with a very well characterized database that looks at the occupational issue. Roberts, et al meets that criterion in a 2013 study of high-risk occupations for suicide. The researchers looked at the numbers of suicides and numbers in all occupations in England and Wales for specific time intervals. They determined the 30 occupations with the highest suicide rates (generally greater than 20/100,000). In comparing the time intervals (1979–80, 1982–83) to (2001–2005) they determined shift in the ranking and discussed possible causes of those changes. Pilots were not listed in the top 30 occupations by suicide rate. The only transportation workers listed were "rail transport operating staff". They noted that suicide rates for professional occupations decreased over the time interval studied while there were sharp increases in the suicide rates for manual occupations. As a comparison the 2013 suicide rate in the US was 12.6 per 100,000.
These incidents are tracked by the Aviation Safety Network and their web site currently lists intentional incidents and accidents caused by pilots dating back to 1976 in commercial flights. There is a separate list of aircraft accidents caused by pilot suicide and that lists 9 suicides in the same time period but proportionally more associated fatalities.
7. Pilots can already self report substance use problems -
There have been some suggestions that screening would be enhanced if pilots could self report problems without the fear of recrimination - the same way that licensed health care professionals are allowed to do in many states. The focus would be on treatment rather than punishment. The health care professional experience demonstrates that this leads to significantly more self reports and that is consistent with the goal of public safety. Since pilot certification occurs at the federal level and health care professional licensing occurs at the state level - there is an opportunity to develop a more standardized approach to the potentially compromised pilot that depends more on self-report than screening. There is currently an "occupational substance abuse treatment program" called HIMS that states at least part of their goal is to preserve careers. A broader focus to include voluntary self- report of psychiatric conditions and suicidal thinking would result in more referrals for treatment and potentially impact the suicide rate.
8. Aviation regulators and the aviation industry collect data that the healthcare industry can only marvel at -
Reading through the sheer amount of data and how it is acquired it is evident that anyone involved in aviation has a single-minded focus on safety. The methods of data acquisition through flight recorders and the checks and balances on the ground are far superior to any safety standards in the health care industry in the United States. As a basic thought experiment, can you imagine recording similar outcome data from patients rapidly discharged from hospitals in the US? I am talking about real data and not the survey that the nurse hands a patient after they have coached them on what to check off.
I don't have to imagine what that data would look like. I know what that data looks like and it is quite ugly. It is more than a little ironic that health care experts, especially in this case psychiatrists and other behavioral experts are going to rush in and correct what is wrong with the aviation industry. By comparison, health care measurement and incident analysis is all smoke and mirrors. They don't know how to collect relevant data and many of the outcome measures are strictly political and meaningless. If anything we should be bringing in aviation safety experts to run hospitals instead of MBAs.
With what I have read, I doubt that there is any possible improvement beyond voluntary reporting and making sure that there is always a second crew member in the cabin on commercial airliners. In some of the commercial aircraft crashes the planes were stolen by staff who were not pilots and crashed. But in the case of air disasters that resulted in multiple passenger deaths a second person in the cabin is a clear safeguard. I am not an expert on how many people are in air crews, but I know that there is also a flight engineer in the cabin in some cases. Given that these incidents are rare by any combination of numerators and denominators that are chosen and the fact that screening for rare events is generally not successful, screening for these rare events is not likely to work. Flight crews currently undergo random urine toxicology to prevent the use of intoxicants that can impair the ability of a pilot. Anecdotal evidence would suggest that is useful, but in the case of addictions there are often attempts to circumvent this intervention or use a drug that is not detectable. The experience of health care professional screening programs would suggest that voluntary reporting can both improve public safety and preserve careers. That seems like a useful approach for pilots.
Most importantly, the aviation industry is a model for safety assurance and the investigation of incidents where there were lapses. It holds many lessons for the health care industry.
George Dawson, MD, DFAPA
Akin A, Chaturvedi AK. Selective serotonin reuptake inhibitors in pilot fatalities of civil aviation accidents, 1990-2001. Aviat Space Environ Med 2003; 74(11):1169–76
Canfield DV, Dubowski KM, Whinnery JE, Lewis RJ, Ritter RM, Rogers PB. Increased cannabinoids concentrations found in specimens from fatal aviation accidents between 1997 and 2006. Forensic Sci Int. 2010 Apr 15;197(1-3):85-8. doi: 10.1016/j.forsciint.2009.12.060. Epub 2010 Jan 13. PubMed PMID: 20074884.
Zeki Dulkadir, Gülhane, Arvind K. Chaturvedi, Kristi J. Craft, Jeffery S. Hickerson, Kacey D. Cliburn. Antidepressants Found in Pilots Fatally Injured in Civil Aviation Accidents. Federal Aviation Administration, Office of Aerospace Medicine, Nov 2014.
Russell J. Lewis, Estrella M. Forster, James E. Whinnery, Nicholas L. Webster. Aircraft-Assisted Pilot Suicides in the United States, 2003-2012 Civil Aerospace Medical InstituteFederal Aviation Administration. Oklahoma City, OK 73125 February 2014
Ungs TJ. Suicide by use of aircraft in the United States, 1979-1989. Aviat Space Environ Med. 1994 Oct;65(10 Pt 1):953-6. PubMed PMID: 7832739.
Bills CB, Grabowski JG, Li G. Suicide by aircraft: a comparative analysis. Aviat Space Environ Med. 2005 Aug;76(8):715-9. PubMed PMID: 16110685.
Ramaekers JG, Moeller MR, van Ruitenbeek P, Theunissen EL, Schneider E, Kauert G. Cognition and motor control as a function of Delta9-THC concentration in serum and oral fluid: limits of impairment. Drug Alcohol Depend. 2006 Nov 8;85(2):114-22. Epub 2006 May 24. PubMed PMID: 16723194.
Roberts SE, Jaremin B, Lloyd K. High-risk occupations for suicide.
Psychol Med. 2013 Jun;43(6):1231-40. doi: 10.1017/S0033291712002024. Epub 2012
Oct 26. PubMed PMID: 23098158; PubMed Central PMCID: PMC3642721.
Aviation x Antidepressant Medline Search April 2015: http://www.ncbi.nlm.nih.gov/sites/myncbi/1-MAvBcofi/collections/47791909/public/
Carl Bialik. We Don't Know How Often Pilots Commit Suicide. FiveThirtyEight (a very sophisticated blog)