As far as I can tell there are two basic considerations in whether or not you trust your physician. The first is combination of personality and cultural factors and the resulting expectations you have when you see a physician. That may have something to do with your actual experience, but also may have more to do with observations from the care of other people. As an example, you saw your father was cared for and thought it was excellent care and expect the same care for yourself. That can also backfire in the case where you believe the observed care was substandard and led you to be more skeptical of medical care administered by physicians. From a cultural standpoint, you may be from a culture that does not trust authority figures or even physicians. These are all very complicated issues, that I will illustrate with personal examples of treatment I have received over the years.
The second approach to whether or not you trust your physician,
is to adopt a very performance-based approach. That approach is the answer to
the question: “What has this doctor done for me and do I like those results?” Medicine
is a complex field made more complicated by subjective assessment of the patient
in their experience of care and treatment. As a psychiatrist, I see people who
are very satisfied with their care from physicians and surgeons and many who
are dissatisfied. I see people who have had the exact same procedure – let’s
say a hip replacement with identical functional results. One of these patients will tell me, that they
are doing very well and the other will describe disappointment. The disappointed patient will often tell me
they are only slightly improved than when their joint was “bone on bone”.
My own experience with physicians is mixed at best. When I
was a teenager, was in a doctor’s office and developed acute facial swelling,
wheezing, and my eyelids were swollen to the point I could barely see. The
explanation was given to my parents at the time was it was “psychosomatic” I
was not treated with anything. The next several years, the only treatment I got
was to get up at night go out into the cool night air and drink caffeinated
soda. Needless to say that was suboptimal. When I finally saw an allergist
about six years later I was “allergic to everything” and finally started taking
antihistamines. But eight years later when I was intern, I saw an allergy
specialist who spent the entire interview demanding to know what I wanted to
try immunotherapy. I guess it was his form of motivational interviewing. I never went back.
In medical school, I started to get gout attacks. With the
first attack I went the emergency department and spent six hours there. I was discharged with acetaminophen and
codeine – a medication that is essentially worthless for gout pain. During a
follow-up appointment in the orthopedic clinic, I was told that I probably
sprained my ankle in bed and they put a cast on it. Gout pain gradually
resolves after about two weeks and that is what happened. But the gout saga
does not end there. During residency I started to get acute wrist pain. I went
to a primary care clinic where the physician learned my history and then tried to
aspirate my wrist joint with a large needle. That was a skill set that he did
not have, but he did end up aspirating some tissue into the syringe that was
eventually identified as synovium from the joint. At some point, I also had a left inguinal
lymph node biopsy that went awry. I went back to work and started gushing blood
all over my khakis. The surgeon advised me to come to his office right away and
by then my shoes were full of blood. I left bloody footprints all over his
carpeting. He cut open the incision and
tied off the artery in the office while two nurses held me down.
That is a sampling of my negative experience. There is
actually a lot more, but despite these fiascoes I have been able to find
physicians that I trust and routinely go back to see. I have been seeing the same
primary care physician for the past 30 years - recommended by psychiatric colleague
who worked with him.
From a cultural standpoint, I was taught to be skeptical of
everyone. My father was a blue-collar worker who routinely talked about the
abuses of the administrative class and how working people were taken advantage
of. He was in a union and would routinely show me the house that the president of
the union lived in compared to our house.
That perspective is still ingrained at some level, but it does not prove
very useful when it comes to medical care. The reason is that at some point almost
everybody needs medical care and that typically includes care that involves
doing something that you would rather not do. That might be surgical procedure or taking medication for a long time or even getting an immunization. But the
choices are often fairly dire and that is continue to be miserable or die or
accept the recommended treatment. Despite my medical misadventures, I continue
to accept doctor’s recommendations even when they have significant risk.
I also come at this from the perspective of interacting
with thousands of patients, many of whom don’t trust doctors at all. In most
extreme circumstances, I had to interact productively with people who not only
did not trust doctors but were simultaneously being coerced into treatment by
the probate court system. In other words they were on involuntary holds,
probate court holds, or civil commitment. That was the best possible experience
to conceptualize the physician trust issue. A typical exchange follows:
MD: “Hi – I’m George
Dawson and I’m the psychiatrist here. It looks like I am seeing you because you
were admitted to this unit on a 72-hour hold.”
Pt: “I don’t trust psychiatrists. I just want to be
discharged.”
MD: “In order to do that, I have to make an assessment of
the situation and determine if you can be released or not.”
Pt: “Why should I trust you?”
MD: “I can’t think of a reason why you should. You just met
me. I would suggest that we proceed with the evaluation and see how that goes.
At the end of the evaluation I will let you know what my impression and
recommendations are. You can decide whether or not you trust me based on what
happens. If you decide to follow my recommendations you can also base your decision on whether or not those recommendations work for you. Does that seem
reasonable?”
That is the basic framework that I tried to outline for people
are focused on trust. The focus is on actual performance as well as
subjectivity. The subjective elements are a number of factors on the patient’s
side. They include all of the conscious
and unconscious factors involved in interpersonal assessments as well as any
overriding psychopathology. The most important element of the patient’s conscious
state is whether or not they can incorporate the information that they are
receiving from the physician into their responses and adapt a different framework
for the interaction. Not everybody is able to do that, but the great majority
of people are to some degree.
The above example is from what is probably the most
contentious situation. I think the
approach works even better in outpatient settings where people have had
adverse experiences in psychiatric care like my experiences with medical
care. In some of those situations a description
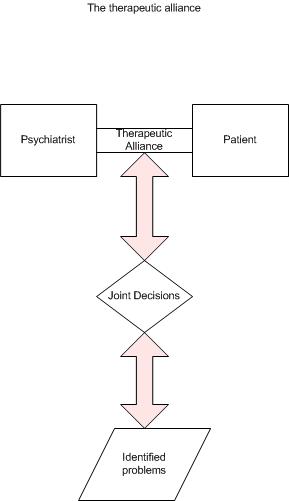
of the therapeutic alliance is useful. That might go something like this:
“It might be useful to discuss how these interviews
work. You and I are both focused on the
problems that you identify. We discuss
them and at some point, my job is to give you the best possible medical advice
on how to address them. Your job at that
point is to think about that advice and whether or not you find it useful and want
to use it. It is also possible that your problems are not medical or psychiatric in nature. I will let you know if I think so.”
That clarifies a few points. The interview is not a unilateral “analysis”. Many people have the psychiatric stereotype
that a psychiatrist can just look at you and figure out the problem. To this
day, many people that I casually meet still ask me if I am “analyzing them.” It also points out that I am interested in
what they identify as problems – not somebody else’s idea of the problem. Unless
that is explicit, many people go out of their way to tell me that it was their
idea to see me or go to treatment. Most
importantly – it emphasizes that this is a cooperative effort. I have no preconceived idea about their problem
or diagnosis. My ideas develop from the
discussion and there has to be agreement that I am on track.
That is my basic approach to the trust issue in interactions
with patients. There are many variations
on that theme. Although what I have
written here is from the physician perspective – I can add that from the
patient perspective the performance dimension is very important. My personal internist always takes enough
time to assess my problems and do an adequate evaluation. He has made some remarkable diagnoses based
on those evaluations. That performance
over time builds trust as well. It also
highlights another important aspect from the patient perspective and that is
empathy towards the physician. Is there
an understanding of how the physician’s cognitive ability and emotional
capacity can be affected by outside factors? Is there any allowance for even
minor physician errors or lapses in etiquette – like being very late for an appointment? People vary greatly in that capacity and often
it is necessary to keep a productive relationship going.
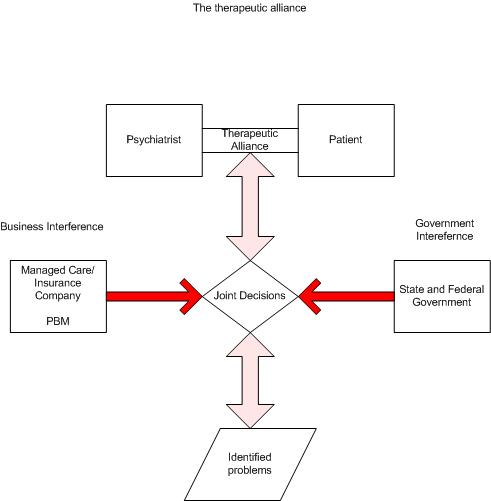
Most medicine these days is run by corporations rather than
physicians. That makes it harder to establish long term relationships with
physicians. In the above narrative I hope that I outlined the advantages of
that relationship as opposed to one that may be more like being asked 20
questions about a medical condition by different people every time you go into a clinic.
George Dawson, MD, DFAPA