There is always a lot of news about the prostate these days. It has become the poster child of the evidence based crowd. Just last week I saw the headline: "Men are more likely to die in a structure fire than from prostate cancer." This is all part of the political approach to epidemiology that emphasizes that even though most men will develop some type of prostate cancer by the age of 85, they are likely to die of other causes. Therefore PSA screening is not useful because it leads to more invasive procedures with complications like prostate biopsy and then procedures with even more complications like radical prostatectomy. The sordid aspect of this business has been pointing out the options that several celebrities who made decisions about prostate cancer and therapies. Depending on the side you take - you will cheer the representative decision. I noticed that the celebrities who died from prostate cancer including misdiagnosis are omitted from that equation.
In clinical practice, young men with recurrent prostatitis have always been a red flag for me. They often end up on very long courses of antibiotics and seem to have chronic symptoms. The symptoms don't match descriptions of acute prostatitis that are more similar to an acute urinary tract infection. The anatomy of the male urinary tract often needs to be reviewed, especially the relationship of the prostate and the urethra. I have treated many young men who were very angry at their Urologists because of these chronic symptoms even though they were not medically explained. If I see these situations today - I typically call the Urologist and suggest treatment only for a clear cut case of prostatitis and whether they have noticed any changes in the patient's behavior.
My focus in this post is bladder outlet obstruction and all of the associated phenomenon due to benign prostatic hyperplasia. According to UpToDate (10) it is more common in men and 10% of men greater than the age of 70 and 1/3 of men over the age of 80 will develop it. Treatment is necessary to prevent renal complications, bladder dysfunction, infection and in severe cases delirium. I don't intent to focus on the urological treatment - only as required to explain the situation. I am more interested in what happens with this disorder and how the presentation may appear to be psychiatric. I think that this is a neglected are in the literature. Please send me any references that I may have missed.
The neuroanatomy and physiology of micturation is a complicated process. At the local level, micturation is innervated by both the sympathetic and parasympathetic nerves. The sympathetic efferent innervation inhibits β3 adrenoreceptors to relax the detrussor muscle of the bladder and activates α1 receptors at the level of the urethra. Parasympathetic efferent innervation activates M3 muscarinic receptors in bladder smooth muscle and motor neurons stimulate acetylcholine nicotinic receptors in the external urethral sphincter to cause contraction. Relaxation of that sphincter muscle is facilitated by postsynaptic parasympathetic neurons that release ATP and nitric oxide. The efferent arm of micturation requires close coordination of that combination of motor and sympathetic nervous system components.
The afferent side of this function begins at the level of the bladder epithelium. These cells have complex signalling functions that can lead to local vascular and muscular responses in addition to sensory information being sent to higher centers. Bladder epithelium and underlying myelofibroblasts may function to send a stretch signal as the bladder fills. The actual mechanism that initiates that signal was not clear from the review I read. A local acetylcholine based mechanism was thought to led to local bladder contractions. This was thought to be the reason that antimuscarinic agents were used for bladder spasticity.
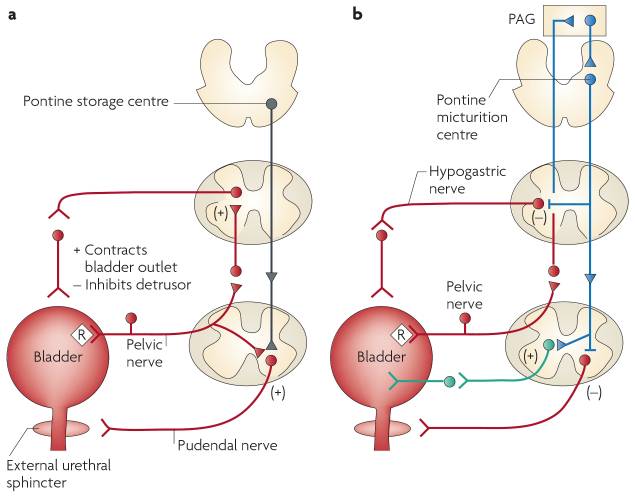
This process was not delineated very well until about the past 10-15 years. A combination of brain imaging during micturation and neuroscience techniques applied to determine the anatomic pathways. One of those techniques was the application of pseudorabies virus to the wall of the rat bladder. This technique leads to retrograde transport of the virus into affected structures. Viral markers go to structures in both the peripheral and central nervous system. A wide variety of cortical and subcortical structures are involved including the raphe nuclei, locus ceruleus, red nucleus, periaqueductal grey area, pontine micturation center, and cerebral cortex are involved. The parasympathetic excitatory reflex pathway is presented in the diagram below (1).
The circuits controlling continence
and micturation are shown below. The diagram on the left is the storage reflex
consisting of negative feedback to inhibit detrusor contractions and increase
urethral sphincter activity. In the voiding phase intense afferent activity in
the spinobulbospinal reflex pathways passes the pontine micturation center.
That leads to descending parasympathetic activity stimulates detrusor muscle
and inhibits urethral sphincter activity at the bladder outlet. Associated
structures at the brain level have been suggested by functional imaging
studies. The central mechanism suggested is release of tonic inhibition of the
micturation center by the frontal cortex. Some of the associated structures are
important limbic structures and have connectivity to other organ systems by
sympathetic tracts.
In the case of BPH, there is
increased intraluminal pressure in the proximal urethra or bladder outlet. This
alters the set point of the system. Voluntary voiding occurs but at higher
residual volume and detrussor pressure. That leads to typical symptoms of
frequent voiding, decreased urine flow, and small volumes. In extreme cases
total obstruction can occur on at least a temporary basis requiring temporary
catheter insertion to maintain urine flow.
Getting back to psychiatry, let me
illustrate the relevance of the problem.
Case 1: JD -
a 68 yr old man in fairly good health until about 3 months earlier. At that
time he started to experience profound sleep problems. He has obstructive sleep
apnea (OSA) and uses CPAP - but his parameters looking at the AHI and air
leakage are unchanged. He now has frequent nocturnal panic attacks that awaken him. Upon waking his heart is
pounding and he has palpitations. He purchased a single lead hand held ECG
device that takes a 30 second rhythm strip and recorded one ventricular
premature contraction in 30 seconds. He consulted both his pulmonologist and
cardiologist involved in the original OSA diagnosis. The pulmonologist looks at
his CPAP parameters and concludes that he does not need another sleep study.
The cardiologist tells him that these VPCs are benign and there is nothing to
worry about. JD is concerned because this is a definite change in his health
status and neither physician is concerned.
He went in to see his primary care
physician who examines him and jokes about the cardiac-bladder connection. He
does a prostate exam and concludes that his prostate is "about the 90th
percentile". No further evaluation or treatment is recommended.
His wife notices that he is sitting
up in a chair in the bedroom a lot more at night. He explains that he is having
palpitations and is very anxious at night. His wife tells him to see the
psychiatrist who is treating her for panic attacks. He makes an appointment and
goes in about 2 weeks later.
The psychiatrist does a complete
history and sleep assessment and concludes that these are not typical panic
attacks. JD recalls a number of dreams where he is running, exerting himself,
or very fearful in the dreams. He awakens with his heart pounding and
experiencing the irregular beats. As soon as he is able to void, the
tachycardia and palpitations resolve. The psychiatrist thinks they are related
to the episodes of urinary frequency and urgency associated with BPH and that
therapy targeted to address the bladder outlet obstruction will lead to a
resolution of the sleep problems and panic attacks. Since seeing his primary
care physician JD has acquired a wrist watch with a vibrating alarm. He uses it
to wake himself up at 2AM and 4AM and finds that pre-emptive bladder emptying
greatly reduces but does not eliminate the nocturnal panic attacks entirely.
The psychiatrist refers JD to a Urologist. He is assessed and treated with
tamsulosin - an alpha blocker that relaxes smooth muscle fibers in the bladder
neck and prostate. Taking the medication results in a significant improvement
but not a normalization of bladder emptying. JD is back to voiding once a
night. He has no nocturnal panic attacks or dreams where he is fearful or
exerting himself.
The background and case
illustrate a few points. Now that micturation is no longer a black box in the
brain, the affected structures and the types of symptoms that can be generated
need to be considered. It is an easy mistake to treat what seems like a panic
attack like a panic attack - especially when previous physicians have not been
impressed enough to work up or treat the problem. Nocturnal panic attacks in a
68 year old man with no previous psychiatric history suggests that there are
possible medical causes for these symptoms and in this case it was bladder
outlet obstruction. The closest syndrome to account for the findings in this
case is cystocerebral syndrome - typically delirium in elderly men with acute
urinary retention where no other cause can be identified (3-9). Decompressing
the bladder typically results in resolution of the acute confusion. That has
led several of the authors to postulate that an adrenergic rather than
anticholinergic mechanism is involved. I don't not have access to all of these papers
and cannot tell if the authors documented some of the problems noted in the
case described here (tachycardia, palpitations, VPCs, anxiety and panic) but
they are all presumptive hyperadrenergic mechanisms.
Whether sleep disturbance, panic
attacks, and eventual delirium can all occur in the same men with bladder
outlet obstruction is not known at this point. That progression of symptoms
seems to make sense but it is not well documented and may just be another
syndrome waiting for better characterization. One of the main differences may be the post void residual volume. In the case presented here that was about 200-300 ml. In the literature on cystocerebral syndrome there is usually urinary retention and a much larger volume - often 1 liter or more.
Until then BPH and the associated lower urinary tract symptoms (LUTS) are markers that psychiatrists and sleep medicine specialists need to pay close attention
to - especially if it comes with insomnia, panic attacks and palpitations.
George Dawson, MD, DFAPA
References:
1: Fowler CJ, Griffiths D, de Groat WC. The neural control of micturition. Nat Rev Neurosci. 2008 Jun;9(6):453-66. doi: 10.1038/nrn2401. Review. PubMed PMID: 18490916.
2: Griffiths DJ, Fowler CJ. The micturition switch and its forebrain influences. Acta Physiol (Oxf). 2013 Jan;207(1):93-109. doi: 10.1111/apha.12019. Epub 2012 Nov 16. Review. PubMed PMID: 23164237.
4: Washco V, Engel L, Smith DL, McCarron R. Distended bladder presenting with
altered mental status and venous obstruction. Ochsner J. 2015 Spring;15(1):70-3.
PubMed PMID: 25829883; PubMed Central PMCID: PMC4365850.
5: Saga K, Kuriyama A, Kawata T, Kimura K. Neurogenic bladder presenting with
cystocerebral syndrome. Intern Med. 2013;52(12):1443-4. PubMed PMID: 23774572.
6: Young P, Lasa JS, Finn BC, Quezel M, Bruetman JE. [Cystocerebral syndrome].
Rev Med Chil. 2008 Nov;136(11):1495-6. Spanish. PubMed PMID: 19301784.
7: Waardenburg IE. Delirium caused by urinary retention in elderly people: a case
report and literature review on the "cystocerebral syndrome". J Am Geriatr Soc.
2008 Dec;56(12):2371-2. doi: 10.1111/j.1532-5415.2008.02035.x. Review. PubMed
PMID: 19093953.
8: Blè A, Zuliani G, Quarenghi C, Gallerani M, Fellin R. Cystocerebral syndrome:
a case report and literature review. Aging (Milano). 2001 Aug;13(4):339-42.
Review. PubMed PMID: 11695503.
9: Liem PH, Carter WJ. Cystocerebral syndrome: a possible explanation. Arch
Intern Med. 1991 Sep;151(9):1884, 1886. PubMed PMID: 1888260.
8: Blackburn T, Dunn M. Cystocerebral syndrome. Acute urinary retention
presenting as confusion in elderly patients. Arch Intern Med. 1990
Dec;150(12):2577-8. PubMed PMID: 2244775.
10: Glen W Barrisford GW, Graeme MS, Steele S. Acute urinary retention. O'Leary MP, Hockberger, RS Editors. UpToDate. Waltham MA: UpToDate Inc. http://www.uptodate.com (Accessed on March 30, 2018.)
Graphic Credits
Both neuroanatomy and urology graphics in this post are from reference 1 and posted here:
Reprinted by permission from Nature/Springer: Fowler CJ, Griffiths D, de Groat WC. The neural control of micturition. Nat Rev Neurosci. 2008 Jun;9(6):453-66. doi: 10.1038/nrn2401. Review. PubMed PMID: 18490916. License number 4319020942759
The graphic of the empty sample cup is from Shutterstock per their standard licensing agreement.
10: Glen W Barrisford GW, Graeme MS, Steele S. Acute urinary retention. O'Leary MP, Hockberger, RS Editors. UpToDate. Waltham MA: UpToDate Inc. http://www.uptodate.com (Accessed on March 30, 2018.)
Graphic Credits
Both neuroanatomy and urology graphics in this post are from reference 1 and posted here:
Reprinted by permission from Nature/Springer: Fowler CJ, Griffiths D, de Groat WC. The neural control of micturition. Nat Rev Neurosci. 2008 Jun;9(6):453-66. doi: 10.1038/nrn2401. Review. PubMed PMID: 18490916. License number 4319020942759
The graphic of the empty sample cup is from Shutterstock per their standard licensing agreement.