This is an interesting topic from a personal, practical,
and consciousness level. I came by some of this knowledge the hard way and hope
to pass that along to people who can benefit from it. I also hope to reach the
people that are thinking right now “I can make the best of staying at home by only eating between 2 PM and 9 PM, increasing my
resistance workouts, and doing more intervals or HIIT (high-intensity interval
training)”. You might be able to but
there are some precautions along the way.
A couple of high points from my experience. About 10 years
ago, I was out on the local speedskating track. I had just started warming up
and noticed my heart rate monitor was at 160 bpm. I did not see that is being
out of the ordinary and after another couple of laps my monitor started
chirping away. The display read 240 bpm. There was also a warning light. I
checked my carotid pulse and sure enough I was in atrial fibrillation. That
began a 10-year saga of cardiac ultrasounds, stress tests, episodes of
anticoagulation, cardioversion, and antiarrhythmic therapy. The ultimate
diagnosis was lone atrial fibrillation. In other words, atrial fibrillation from
no known structural cause. The likely cause was long periods of time of running
my heart rate way beyond the maximum recommended heart rate for a guy my age.
Even before that I was out speedskating on the roads when I
went down and ended up with a large abrasion over my left lateral thigh. My
first thought was whether I should cover it with something. It was a clean
abrasion that I had washed thoroughly and immediately and it looked good. Over the next several days it no longer
looked good and was clearly infected. In the emergency department was given
an intramuscular injection of cephalexin with a number of capsules to take
home.
Both of these scenarios highlight the fact that exercise related
injury can lead to treatment in the ED (emergency department). During the time of a
pandemic you do not want to end up in an emergency department. So the first
lesson here is to avoid extremes and also high risk scenarios where you could
end up with an abrasion, a cut, head trauma, fracture, a sprain, or any other
sports injury that needs acute medical attention. I think there are practical ways
around that but it also takes addressing the exercise fanatic mindset.
1. Avoid the gym:
I can only speak for what happens in the men’s locker room
but hygiene at the gyms I have been in is atrocious. It is the primary reason I
stopped going to gyms even though my wife encourages me to go to her gym on a
regular basis. There is also the problem of risky behavior. I got tired of
seeing personal trainers trying to kill novices with some absurd exercise
routine, the roid rage folks
threatening one another, and having to intervene in order to prevent serious
injury. You can only advise that teenager with a loaded barbell resting on his
cervical spine that it is not a good idea so many times, before you get
known as the old white guy who is a know-it-all. Luckily many governors and mayors have shut
these facilities down as a transmission risk.
2. Maintenance not
maxing out:
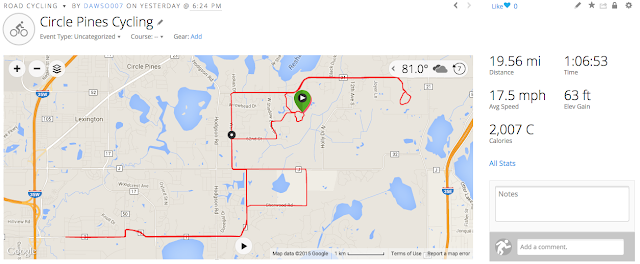
Most exercise fanatics collect a lot of data on their favorite
exercise routines. You can certainly do it with smart phones and activity
monitors these days but a lot of us also automatically keep track of reps,
times, and maximums. For example on a day-to-day basis I can predict my maximum
number of push-ups, pull-ups, back extensions, bicep curls, max power output on
my ergometer, and max road speed on a bike. When you think like an exercise
fanatic, you are always thinking about how to maximize those numbers. That also
happens to be the periods of likely injury. I naturally hit a wall at about age
55. Up to that point I thought it was indestructible in terms of exercise
tolerance. After that point, I questioned why I had been so foolish and not adhered
to some basic rules like maximum heart rate. First and foremost don’t push it like you are
20 when you are 40 or 50. Secondly, don’t push it to high age-appropriate
levels when there emergency services are limited by a pandemic and you don't want to be an additional burden on that resource.
3. Avoid the typical Internet suggestions:
During this period of social isolation there are any number
of exercise sites advising you on how to stay fit outside of the gym. They
range from exercises that focus on specific body regions to replacing exercise
equipment with everyday household items. Keep in mind that doing reps with a
gallon of milk or a can of paint is not like using that Cybex machine at the
gym. The biomechanics are completely different and even the grip can result in
injury. Don’t take innovation too far when it comes to exercises that you are
used to doing in a specific range of motion on well-designed equipment. Even
mimicking that young aerobics instructor video and she does various leg
extensions can be a problem. Start out with very few repetitions to make sure
it is safe before you try the whole workout. Even then there are exercise that are not appropriate for certain ages or injury patterns. Many athletes have learned this over a number of years from their physical therapist. Don't ever ignore the advice of a physical therapist.
4. Stop immediately if you are hurt; don’t exercise until
the pain is long gone. If it doesn’t go
you need an assessment.
Repetitive stress and overuse injuries are common with
aging and you have to overcome the propaganda that you heard in high school or
your early 20s that all you have to do is “shake it off” or that pain is
somehow therapeutic. I first noticed significant knee pain when I had to carry
a floor sander up three flights of stairs. It weighed about 250 pounds. I
remember thinking as I went up that stairway: “It feels like my knees are going
to blow out at any time”. I was about forty years old. By paying
close attention to that feeling I have been able to preserve my knees for
another 25 years. During that time they have served me well with thousands of
miles of cycling and speedskating. I pay close attention to that joint stress
perception when I am weightlifting or even doing push-ups or pull-ups. I plan
to avoid any of those situations during the pandemic social isolation.
These are a few tips to avoid injury and needing medical
care during a pandemic. To most people they are obvious. To exercise fanatics
they may not be. Being an exercise
fanatic is an interesting conscious state. Reality testing is intact to a large
extent. As an example I would never think that I could skate in the Olympics or
cycle in the Tour de France. At the same time my personal goals were probably
unrealistic for men my age and yet I reached many of them. The part of my
reality testing that was not intact involved the basic denial of the aging
human organism. For example, I recognized in a nick of time that my spine
could probably not tolerate lifting large amounts of weight anymore. As we age,
intervertebral discs degenerate and in many cases disappear. Osteophytes form. The old
human spine is a lot less stable then the young human spine. That has
implications for maximum load whether that load is a stack of weights or
running.
I used to think that men were particularly prone to the
exercise fanatic mindset but since then I have encountered many women with the
same biases. A significant number of them continued to exercise when they were
injured and ended up with permanent disabilities. Women may be more likely to
be told that their exercise is “an addiction” because of the over exercising
associated with an eating disorder diagnoses. They have that bias to live with
that men generally do not.
Stay fit during this time by staying with what you know, taking it easy, and
avoiding injury. If you are an exercise fanatic this is the wrong time to be
pushing your limits - and you might ask yourself if there is ever a right time. Even as a novice it is the wrong time to jump into a rigorous program because there is somebody selling it on the Internet and it looks good.
George Dawson, MD, DFAPA




.jpg)